Article ID: 2019-0001-OA
Article ID: 2019-0001-OA
Maintenance hemodialysis (HD) therapy is essential for survival in patients with end-stage renal disease (ESRD); however, HD can also be life-threatening in the final stages of ESRD. Currently, no clear indicators and/or biomarkers exist regarding when HD should be forgone. In the present study, we examined temporal changes in multiple clinical parameters, including biochemical data, physical data, the use of specific medical treatments, nursing care levels, and the activities of daily living (ADL) in 47 ESRD patients who underwent maintenance HD and who died in our hospital. We also investigated the status of informed consents regarding the forgoing of HD in these patients. We found that while biochemical parameters were unaltered, physical parameters such as consciousness levels and blood pressure gradually deteriorated during hospitalization. The use of the following specific medical treatments significantly increased over time: vasopressor use, O2 inhalation, and ventilator use. The need for nursing care increased and the ADL levels decreased toward the time of death. Medical doctors gave information regarding forgoing HD to patients and/or their family/relatives in 55% of cases, obtained agreement to forego HD in 45% of cases, and HD was actually foregone in 38% of cases. Most clinical parameters were not significantly different between the patients whose HD sessions were forgone versus those in whom HD was continued, indicating that HD was foregone in the very last stages of life. The results suggest that physical parameters, the use of specific medical treatments, the levels of nursing care, and ADL are potential indicators for forgoing HD in the final stages of ESRD.
Maintenance hemodialysis (HD) therapy is essential for survival in patients with end-stage renal disease (ESRD). Consequently, withholding or withdrawing HD therapy is related to the death of these patients. However, HD therapy itself can be life-threatening in the final stages of ESRD.1,2,3 Indeed, extracorporeal circulation occasionally leads to a severe reduction in blood pressure in the final stages. Furthermore, HD therapy sometimes induces lethal arrhythmias resulting from an imbalance in electrolytes. Moreover, keeping vascular access safe during HD sessions is not feasible in some ESRD patients with dementia. Although there are a certain number of cases and situations in which HD should be forgone, currently, no clear indicators and/or biomarkers exist regarding the timing of forgoing HD in the final stages of ESRD.
Several studies have addressed the relationship between clinical parameters and long-term prognosis in ESRD patients. For example, serum levels of albumin and C-reactive protein and the body mass index are associated with mortality in HD patients.4,5,6,7 These biomarkers reflect the status of nutrition or inflammation, and they are useful for predicting long-term prognosis in ESRD patients. However, it remains unknown whether these parameters are also able to predict short-term prognosis in the terminal stages of ESRD. In the field of palliative care for advanced malignancies, multiple scoring systems, such as the Palliative Prognostic Score and the Palliative Prognostic Index, have been developed to predict short-term prognosis.8,9,10 In these systems, clinical parameters, such as edema and dyspnea, as well as biochemical parameters, including the white blood cell count, are used to accurately quantify the expected survival of terminally ill cancer patients. Although these scoring systems may be useful for ESRD patients complicated with advanced malignancies, they are unlikely to be adaptable for other ESRD patients. Novel scoring tools are required to evaluate prognosis during the final stages for most ESRD patients. As an initial step in establishing a scoring system to estimate short-term prognosis in the final stages of ESRD, data for deceased HD patients should be collected.
The aim of the present study was to determine parameters that may be useful to predict the short-term prognosis in the final stages of ESRD. We examined temporal changes in multiple clinical parameters, including biochemical data, physical data, the use of specific medical treatments, nursing care levels, and the activities of daily living (ADL) in ESRD patients who had undergone intermittent maintenance HD and who died in our hospital. Moreover, in these patients, we investigated whether explanations had been given by medical doctors regarding forgoing intermittent HD and whether patients and their family/relatives had given agreement for this to be implemented. Finally, we compared the clinical parameters at the last HD session between patients whose HD session had been forgone versus those in which HD had been continued.
This retrospective study was conducted at a single center in Japan. The study protocol was approved by the Ethics Committee of Keio University School of Medicine (IRB Approval Number: 20170245). The IRB waived the need to obtain written informed consent from the family/relatives of deceased patients, although the study protocol was disclosed and opting out was allowed. Between January 1st, 2014, and September 30th, 2017, 1072 ESRD patients underwent intermittent maintenance HD therapy during their hospitalization at Keio University Hospital. Among these patients, 47 died during their stay in hospital and were recruited to this study. In the present study, patients undergoing maintenance HD therapy were defined as those receiving intermittent HD therapy for longer than 2 months. If patients changed the dialysis modality from intermittent HD therapy to continuous hemodiafiltration therapy during their admission, the last HD session was defined as the last session of intermittent HD.
DataData regarding gender; age; ESRD etiology; the dates of admission, the last HD session, and death; the reasons for admission and death; the reasons of forgoing HD; HD duration; and family composition were obtained from medical records. Biochemical data, including the levels of hemoglobin, total protein, albumin, urea nitrogen, creatinine, potassium, phosphate, and C-reactive protein, as well as physical data, such as consciousness levels, systolic and diastolic blood pressure, and heart rate were also collected. Data regarding the presence or absence of intravenous fluid infusion, vasopressor use, red blood cell transfusion, narcotic use, O2 inhalation, ventilator use, chemotherapy, and radiation therapy were collected. Data regarding nursing requirement levels, such as the presence or absence of syringe pump care, respiratory care, wound care, and ADL, such as turning patients on beds, transfer between beds and chairs, changing clothes, eating, and oral care were obtained. Also obtained from medical records were data regarding the presence or absence of medical doctors’ explanations about the “do not attempt resuscitation (DNAR)” option and the forgoing of HD, as well as any agreements by patients and their family/relatives.
Statistical analysesNormally distributed continuous variables were expressed as the mean ± standard deviation (SD), non-normal variables were expressed as the median and interquartile range (IQR), and categorical data were expressed as percentage frequencies. To test differences between groups, Student’s unpaired t-test or one-way ANOVA with a post hoc Fisher’s protected least significant difference test was used for normally distributed variables. For non-normal variables, the Mann–Whitney test or Kruskal-Wallis one-way ANOVA on ranks test was employed, and for categorical data, the χ2 test or Fisher’s exact test was used. All statistical analyses were performed using SigmaPlot/SigmaStat 9 (Systat Software Inc., San Jose, CA, USA). P < 0.05 was considered significant.
Between January 1st, 2014, and September 30th, 2017, forty-seven patients undergoing maintenance HD died in our hospital (Table 1). Thirty-nine of them were men, and eight were women. The median age at death was 74.0 years (IQR: 65.0–79.0), and the HD duration was 34.0 months (IQR: 4.5–108.5). Patients had been admitted to the hospital for 42.0 days (IQR: 14.0–98.0), and the time from the last HD session until death was 2.0 days (IQR: 1.0–3.5). Five patients underwent continuous hemodiafiltration therapy after the last intermittent HD session, but they died within 2–12 days. The etiology of chronic kidney disease (CKD) was diabetes (21% of patients), hypertension (21%), primary glomerular diseases (17%), polycystic kidney disease (9%), multiple myeloma (9%), and others (23%). The reasons for admission to hospital were as follows: cardiovascular diseases (38%), gastroenterological disorders (23%), infectious diseases (17%), malignancies (13%), and others (9%). The causes of death were infectious diseases (44%), cardiovascular diseases (30%), malignancies (11%), gastroenterological diseases (9%), and others (6%). Of the 47 patients, 44 had at least a spouse and/or a relative in the first degree. Of the remaining three patients, one had a sister, one had a brother, and one had an uncle.
| Male (%) | 83 |
|---|---|
| Age at death (years) | 74.0 (IQR: 65.0–79.0) |
| HD duration (months) | 34.0 (IQR: 4.5–108.5) |
| Duration of hospitalization (days) | 42.0 (IQR: 14.0–98.0) |
| Duration from last HD to death (days) | 2.0 (IQR: 1.0–3.5) |
| CKD etiology (%) | |
| Diabetes | 21 |
| Hypertension | 21 |
| Primary glomerular diseases | 17 |
| Polycystic kidney disease | 9 |
| Multiple myeloma | 9 |
| Others | 23 |
| Causes of admission (%) | |
| Cardiovascular diseases | 38 |
| Gastroenterological diseases | 23 |
| Infectious diseases | 17 |
| Malignancies | 13 |
| Others | 9 |
| Causes of death (%) | |
| Cardiovascular diseases | 30 |
| Gastroenterological diseases | 9 |
| Infectious diseases | 44 |
| Malignancies | 11 |
| Others | 6 |
The median values and interquartile ranges (IQR) or percentages are shown.
Regarding 47 deceased patients, changes in biochemical and physical parameters were examined at four time points during their admission, including the time of admission, 2 weeks before death, before the last HD session, and immediately before the death. As shown in Fig. 1, biochemical parameters, including the levels of hemoglobin, total protein, albumin, urea nitrogen, creatinine, potassium, phosphate, and C-reactive protein were unaltered among the four time points examined during hospitalization. On the other hand, multiple physical parameters, including the consciousness levels, systolic blood pressure and diastolic blood pressure, but not the heart rate, significantly declined during the course of admission (Fig. 2). Indeed, the proportion of the HD patients with disturbed consciousness gradually increased during the period of hospitalization (Fig. 2A). In addition, systolic blood pressure (120 ± 30 mmHg at admission, 113 ± 26 mmHg at 2 weeks before death, 106 ± 21 mmHg at last HD session, and 90 ± 27 mmHg on the day of death) and diastolic blood pressure (62 ± 16 mmHg at admission, 61 ± 15 mmHg at 2 weeks before death, 60 ± 15 mmHg at last HD session, and 50 ± 17 mmHg on the day of death) both decreased over time (Fig. 2B,C). Likewise, the proportion of patients who exhibited a marked decrease in blood pressure during HD sessions gradually increased (19% at admission, 29% at 2 weeks before death, and 34% at the last HD session). These results suggest that physical parameters, such as consciousness levels and blood pressure, have a potential to be indicators for death in HD patients.
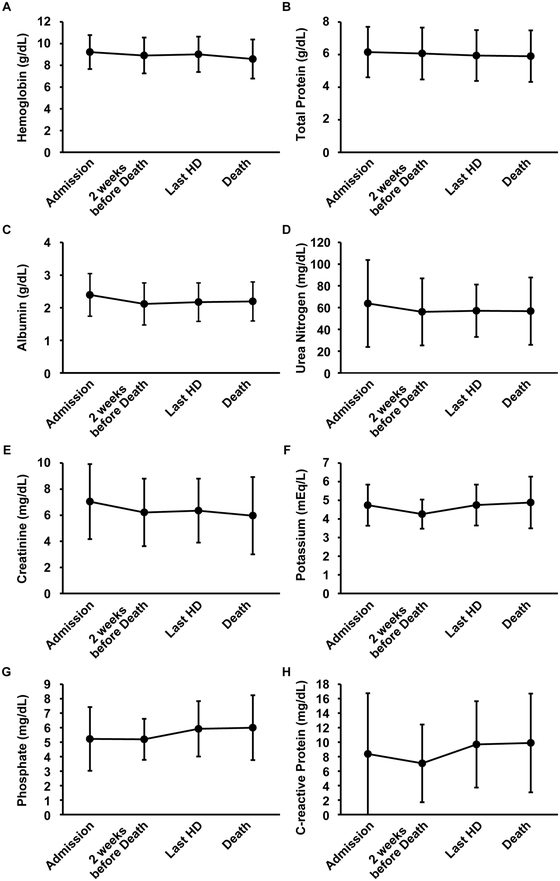
The levels of hemoglobin (A), total protein (B), albumin (C), urea nitrogen (D), creatinine (E), potassium (F), phosphate (G), and C-reactive protein (H) were examined in 47 HD patients at four time points: at admission, 2 weeks before death, before the final HD session, and immediately before death. Differences occurring over time were tested by one-way ANOVA (A and G) or Kruskal-Wallis one-way ANOVA on ranks (B-F, and H). No significant differences over time were found.

Consciousness levels (A), systolic blood pressure (B), diastolic blood pressure (C), and the heart rate (D) were examined in 47 HD patients at four time points. Consciousness levels were evaluated using the Japan Coma Scale (JCS). Differences over time were tested using the χ2 test (A) or one-way ANOVA with a post hoc Fisher’s protected least significant difference test (B-D). *P < 0.05.
Temporal changes in the percentage of patients receiving various medical treatments were examined in the 47 deceased HD patients at four time points during hospitalization: on admission, 2 weeks before death, at the last intermittent HD session, and just before death. The proportion of patients receiving vasopressors or using O2 inhalation or mechanical ventilation significantly increased during admission, whereas the proportion of patients receiving intravenous fluid infusion, red blood cell transfusion, or narcotics was unchanged (Fig. 3). Indeed, only 5 of 47 patients (11%) were being treated with vasopressors at the time of admission, whereas 25 patients (53%) were being administered vasopressors on the day of death (Fig. 3B). The proportion of patients receiving O2 inhalation also increased from 43% at the time of admission to 79% on the day of death (Fig. 3E). The rates of the patients undergoing chemotherapy or radiation therapy were unaltered during admission (data not shown). Changes in the proportion of patients requiring nursing support and ADL were then examined. The need for respiratory care, but not for syringe pump care or wound care, increased gradually and significantly (Fig. 4A–C). The abilities of patients to turn over in bed, change their clothes, eat, and perform oral care deteriorated significantly during the period of hospitalization (Fig. 4D, F–H). The ability of patients to transfer between beds and chairs remained low and did not change significantly (Fig. 4E). These results suggest that the use of specific medical treatments, the required level of nursing support, and ADL are potentially useful to predict the short-term prognosis in HD patients.
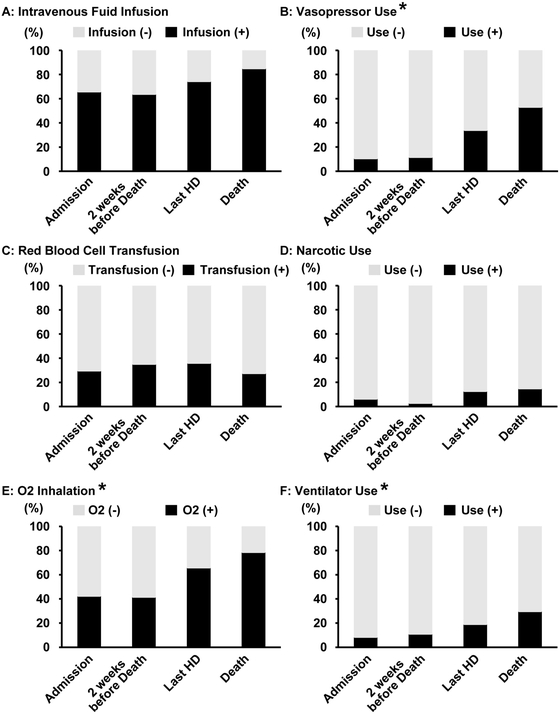
The use of specific medical treatments, namely intravenous fluid infusion (A), vasopressor use (B), red blood cell transfusion (C), narcotic use (D), O2 inhalation (E), and ventilator use (F), was examined in 47 HD patients at four time points. Differences were tested using the χ2 test. *P < 0.05.

Changes in the levels of nursing care required, namely syringe pump care (A), respiratory care (B), and wound care (C), as well as changes in the levels of ADL, including turning over on beds (D), transfer between beds and chairs (E), changing clothes (F), eating (G), and oral care (H) were examined in 47 HD patients at four time points. Differences were tested using the χ2 test. *P < 0.05. NPO, nil by mouth.
We investigated the rates of explanation, agreement, and execution of forgoing HD (Table 2). Among the 47 cases, DNAR was explained to 5 patients (11%) and 45 families/relatives (96%) in advance, and it was executed in 43 cases (91%). Forgoing HD was explained to 2 patients (4%) and 26 families/relatives (55%), and agreement to forgo HD was obtained from 1 patient (2%) and 21 families/relatives (45%). HD was actually foregone in 18 cases (38%). The reasons for forgoing HD were multiple and complex (Table 3). In one case, a family member wanted HD to be resumed after it had been forgone, but HD was not performed because of the deterioration of the patient’s physical condition. Among the 47 deceased patients, none had had an advance directive.
| Yes | No | ||
|---|---|---|---|
| Explanation of DNAR | To patient | 11% | 89% |
| To family/relatives | 96% | 4% | |
| Execution of DNAR | 91% | 9% | |
| Explanation of forgoing HD | To patient | 4% | 96% |
| To family/relatives | 55% | 45% | |
| Agreement to forgo HD | By patient | 2% | 98% |
| By family/relatives | 45% | 55% | |
| Execution of forgoing HD | 38% | 62% | |
| Advanced directive | By patient | 0% | 100% |
| Case number | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reason | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
| Progression of malignancy | Y | Y | Y | Y | Y | Y | Y | Y | ||||||||||
| Deterioration of cardiovascular disease | Y | Y | Y | Y | Y | Y | Y | |||||||||||
| Deterioration of gastroenterological disease | Y | Y | ||||||||||||||||
| Low blood pressure | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||
| Disturbed consciousness | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Severe infection | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||||||||
| Troubles in vascular access | Y | Y | ||||||||||||||||
Forgoing HD was executed in 18 cases. Y, yes.
Finally, we compared multiple factors, including biochemical markers, physical parameters, nursing support levels, use of medical treatments, and the levels of ADL between the patients whose HD sessions were forgone (n =18) versus those who continued (n =29). At the last HD session, most of the parameters examined were not different between the patients who discontinued HD versus those who continued HD (data not shown). However, the explanation of forgoing HD given by medical doctors to the family/relatives, as well as the agreement to forgo HD given by the family/relatives were significantly related to the forgoing of HD being carried out. There were also no differences in the etiology of CKD, the reason for admission, and the cause of death between the groups (data not shown). These results suggest that HD was forgone in our hospital when the condition of the patients was too poor to perform HD safely. In other words, the results suggest that the forgoing of HD was executed at the very last moment in our hospital.
In the present study, we examined temporal changes in multiple clinical parameters, including biochemical data, physical data, the use of specific medical treatments, nursing support levels, and ADL levels in 47 ESRD patients who had undergone intermittent maintenance HD and who had died in our hospital. Whereas the biochemical parameters were unaltered, some physical parameters, namely consciousness levels and blood pressure, the use of specific medical treatments (vasopressor use, O2 inhalation, and ventilator use), nursing support levels, and ADL levels, gradually and significantly changed across the four time points analyzed during the course of hospitalization. The physical parameters deteriorated, whereas the use of specific medical treatments increased. The need for nursing care increased, and the levels of ADL decreased toward the time of death. We also clarified that, among the 47 deceased patients, medical doctors gave information about forgoing HD to the patients and/or their family/relatives in 55% of cases; agreement to forgo HD was obtained for 45% of patients, and forgoing HD was executed in 38% of patients. We also found that most clinical parameters were not significantly different between patients whose HD sessions were forgone and those whose HD sessions were continued, suggesting that, in our hospital, forgoing HD was executed as a result of the severely deteriorated medical conditions of the patients.
The aim of the present study was to explore possible indicators suitable for estimating short-term prognosis in the final stages of life in HD patients. However, the biochemical markers currently examined, including albumin and C-reactive protein, remained unaltered in the final stages of life in HD patients, despite these markers having proven useful for estimating long-term prognosis in ESRD patients.4,5,6,7 To establish a novel scoring system to predict short-term prognosis in ESRD patients, it may be useful to combine several clinical parameters that were shown to change in the present study. Indeed, to evaluate short-term prognosis in terminally ill cancer patients, multiple scoring systems use a combination of several indicators. For example, the Palliative Prognostic Score includes the following variables: clinical prediction of survival, Karnofsky performance status, anorexia, dyspnea, total white blood cell count, and lymphocyte percentage.8,9 Although simple, this scoring system based on clinical and biochemical variables permits quite accurate estimation of expected survival. Using the present study as a first step, it is hoped to establish a novel scoring system to predict short-term prognosis in the final stages of ESRD. To establish such a scoring system in the future, the system will need to be tested not only in deceased patients but also in healthy HD patients.
In the present study, we analyzed data from 47 ESRD patients who died in our hospital between January 1st, 2014, and September 30th, 2017. Although the proposal for the shared decision-making process regarding initiation and continuation of maintenance HD was published in Japanese by the Japanese Society for Dialysis Therapy in 2014 and in English in 2015,3 the advance directive had not been prepared in any cases. This means that the advance directive has not been generally recognized as a tool to express the willingness of patients to have more control over their death. Withholding or withdrawing life-supporting treatment is one of the most important ethical issues for medicine in the 21st century. Measures need to be taken to inform the general public of the existence of the advance directive in the future.
In addition, the proposal for a shared decision-making process has described the importance of a care plan after the forgoing of HD.3 The present study clarified that the median duration from the last HD session to the time of death was 2.0 (IQR: 1.0–3.5) days. Despite this median duration being only 2 days, the medical team, together with the patient’s family, should formulate a care plan. Indeed, among the 47 patients, 2 patients survived more than 20 days after their last HD session. Effective palliative care should be provided to patients whose HD sessions have been forgone.
There are several limitations to the present study. First, all of the 47 cases analyzed died in our university hospital. Although the causes of death and the ages of the patients were similar to those for the entire population of HD patients in Japan,11 it is possible that the cases we analyzed were unique and are therefore not generalizable. For example, HD patients who undergo aggressive treatment tend to stay in our hospital until the final stages, whereas those who decline such treatment tend to move to other hospitals before death. Consequently, the mortality rate of HD patients in our hospital (4.4%) was extremely low. Therefore, it is possible that the HD patients we analyzed represent a biased sample. To ensure generalizability, it would be necessary to obtain data regarding deceased HD patients from various types of clinics, hospitals, and hospices. Moreover, the retrospective nature of the analysis and the small number of patients are also limitations of the study. However, it is quite difficult to perform a study of this nature in a prospective manner. Nevertheless, further studies are warranted to confirm and extend our findings.
In conclusion, the results of the present study suggest that physical parameters, the use of specific medical treatments, and the levels of nursing care and ADL are potentially useful indicators for forgoing HD in the final stages of ESRD. Further studies are required to establish a novel scoring system to evaluate the short-term prognosis for such patients.
The authors declare that no conflicts of interest exist.