Article ID: 2021-0008-IR
Article ID: 2021-0008-IR
Uterus transplantation (UTx) is now a potential option to allow women with uterine factor infertility to give birth. However, UTx is still at an experimental stage, and basic animal studies, including in non-human primates, are needed for the accumulation of data prior to clinical application. Considering that UTx may provide new hope to Japanese women, we launched UTx research in 2009 and have since accumulated a large archive of results in the UTx research field. Furthermore, we have carried out various activities aimed at the implementation of clinical applications of UTx in Japan while clarifying the ethical and social issues involved. Currently, the clinical application of UTx in Japan is just around the corner, and it is expected that UTx research will develop further in the future. Herein, we summarize our basic experiences using non-human primates and our activities with the goal of future clinical applications.
In recent years, uterus transplantation (UTx) has become an option for women with uterine factor infertility (UFI), and clinical trials have already been conducted overseas after the first successful delivery following UTx by a Swedish team (Brännström et al.) in 2014.1 Although UTx is still at the experimental stage, and many medical issues remain unresolved, this new technique in the fields of reproductive and organ transplantation is increasingly being considered worldwide.2
In Japan, approximately 60,000 women of reproductive age with UFI are currently unable to have biological children because gestational surrogacy is forbidden.3,4 Therefore, the clinical application of UTx is expected in Japan to provide an option for women with UFI to have children. With a view to clinical application, we have focused on this new medical technology and have conducted basic experiments over more than a decade using non-human primates that are anatomically and physiologically similar to humans. Following the approach of the Swedish group, we have carried out world-leading basic research on UTx that has resulted in the accumulation of knowledge and of many achievements in the field.5 Moreover, to stimulate social debate on UTx in Japan, we have provided clear, accurate information for dissemination regarding this technology, addressed ethical and social issues, and carried out various activities. Herein, we summarize our background, basic experimental achievements, communications activities, and issues related to UTx research and future perspectives for clinical application in Japan.
The purpose of UTx is to allow the recipient, who has received a uterus transplant from a donor, to have a child. Conventional organ transplantation is performed to save lives, but because the uterus is not a life-sustaining organ, UTx is considered to be an organ transplant to improve the quality of life (QOL). The overall procedure of UTx is as follows: first, fertilized eggs of the couple are cryopreserved in advance. Next, the donor’s uterus is transplanted into the recipient (the ovaries are not transplanted). After engraftment of the transplanted uterus in the recipient, the embryo of the couple is placed in the uterus (embryo transfer). Then, if pregnancy occurs, the baby will be delivered by cesarean section under strict pregnancy control. Because the purpose of UTx is to raise a baby, the transplanted uterus is removed after childbirth (Fig. 1). This allows the recipient to stop taking immunosuppressive drugs; this approach is different from the transplantation of life-supporting organs in that it is a temporary organ transplant.
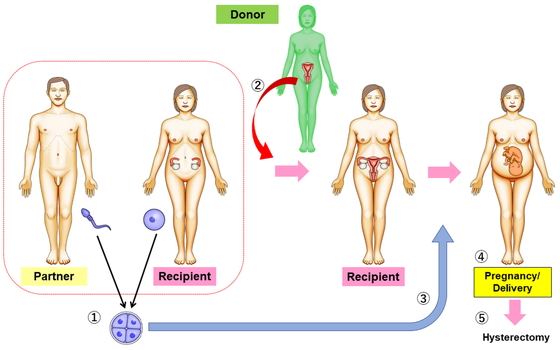
Overview of uterus transplantation.
1, Fertilized eggs of the couple are cryopreserved before uterus transplantation; 2, the donor’s uterus is transplanted into the recipient (the ovaries are not transplanted); 3,after engraftment of the transplanted uterus in the recipient, the embryo of the couple is transferred into the uterus; 4,the aim is pregnancy and a live birth; 5, the transplanted uterus is removed after childbirth.
The subjects for UTx are patients with UFI, who are roughly divided into those with congenital and acquired UFI. Congenital UFI includes Mayer-Rokitansky-Küster-Hauser syndrome (MRKHS), in which the uterus and vagina are absent; uterine hypoplasia; and uterine malformation. Acquired UFI includes patients who undergo hysterectomy to remove malignant uterine tumors, benign diseases (e.g., uterine fibroids and adenomyosis), massive postpartum bleeding, or patients who lost fertility due to severe uterine synechiae, as in Asherman syndrome. Recently, the number of young patients with uterine cancer has been increasing, and it is estimated that more than 1500 women of reproductive age (20–39 years) with uterine cancer annually undergo hysterectomy in Japan, according to the registrations in the Japan Society of Obstetrics and Gynecology cancer registry program.6 Taking immunosuppressive drugs is essential for organ transplantation, and it is debatable whether patients who have had treatment for malignant uterine tumors are eligible as recipients because of concerns about cancer recurrence caused by immunosuppressive drugs.7,8
Donors can be categorized as living or deceased donors (brain-death/cardiac arrest). The organ should ideally be donated from a deceased donor, which clearly has the greatest advantage over a living donor in terms of the elimination of surgical stress.9 Moreover, with a deceased donor, resection of extended vascular pedicles of greater length than those from living donors can be achieved. However, in Japan, organ donation from deceased donors is very limited compared to other countries.10,11 Furthermore, the organs that can be transplanted from deceased donors under the current Act on Organ Transplantation are limited to the heart, lung, liver, kidney, pancreas, small intestine, and eye, so that amendment of the act would be required to permit uterus donation by a deceased donor in Japan. However, it should be noted that there are fewer reports of live births after UTx from deceased donors than from living donors12; indeed, there are several disadvantages to uterine donations from deceased donors, such as difficulty in planning surgery and thorough preoperative screening, longer ischemic time of the donated uterus, the negative effect on the uterus due to vascular insufficiency and systemic inflammatory changes in the agonal stage, and the need for vascular fine treatment (ligation) before reperfusion in back-table preparation.13
The reason that we started UTx research was that, in 2009, a young woman in her twenties had a trachelectomy for cervical cancer. Unfortunately, the uterus could not be preserved due to the progression of cancer, so conversion to radical hysterectomy was performed. During the operation, the question occurred to I.K. (first author): “If this patient received a uterus donation from someone, could she become pregnant and give birth?” This was the beginning of our research on UTx. At that time, no gynecologists knew about UTx in Japan. After a comprehensive literature search, it was noted that the first human UTx had already been attempted in Saudi Arabia in 2000, although the grafted uterus was removed 3 months after surgery because of uterine necrosis and vascular thrombosis.14 Moreover, a Swedish group had performed many basic animal studies using mice, rats, pigs, and sheep.15
Initially, because of the ease of management, we started UTx research using rats. However, we had no experience with microscopic surgery for dissection and anastomoses of small blood vessels, and it was difficult to advance the research. Furthermore, because rats have a bicornuate uterus, even if we succeeded in achieving UTx in rats, that procedure was likely too remote from clinical application in humans. Around that time, the International Federation of Obstetrics and Gynecology (FIGO) guidelines indicated that UTx should only be performed after significant and adequate research in large animal models, including primates.16 Therefore, we selected a non-human primate, the cynomolgus macaque, because the species complied with the guidelines and there were few reports of experiments on non-human primates overseas.
Non-human primate models, including macaques, are frequently used in clinical and non-clinical testing because of the great anatomic and physiologic similarity to humans of their reproductive organs.5 The close correlation of macaque and human immune and reproductive systems has been a significant advantage in terms of their pertinence for extrapolation to humans in the fields of organ transplantation and reproductive medicine,17 although the weight of female macaques is approximately 3–4 kg, which is very small compared to humans, and fine surgical techniques are required. Further, there are specific problems such as difficulties in postoperative medication management and testing, measures that take animal welfare into consideration, and the limitations associated with them.18,19
Because pregnancy and delivery after allogeneic UTx in animal studies had been reported only in rats and sheep,20,21 our tentative goal in basic research was a successful delivery after allogeneic UTx using cynomolgus macaques. The history of initial UTx research is shown in Fig. 2. To date, we have conducted a broad range of experiments on UTx research using approximately 100 cynomolgus macaques; the verification of basic experiments in non-human primates has greatly increased our preparation for the clinical application of UTx. Our research using cynomolgus macaques was performed in strict accordance with the recommendations of the Guide for the Care and Use of Laboratory Animals of the National Research Council and was approved by the Committee of the Animal Research Center, which is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International. A brief summary of our achievements is shown in Table 1.
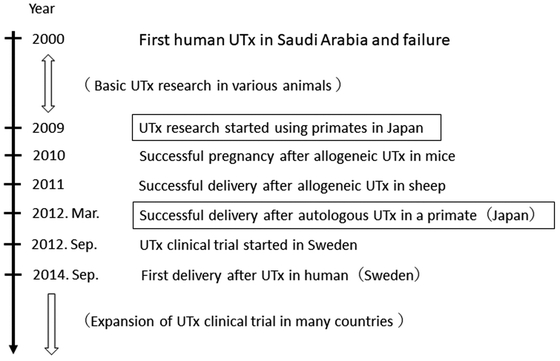
The history of early uterus transplantation research and its transition.
| Subject | Main outcomes | References |
|---|---|---|
| Uterine blood flow | ― Uterine vessels were significantly related to uterine perfusion, whereas ovarian vessels did not have a significant relationship. ― Pregnancy and delivery were supported by a unilateral uterine artery and vein alone. | (19,20) |
| Uterine warm ischemia/ reperfusion injury | ― Warm ischemia in the uterus was tolerated for up to 4 h. ― Uterine ischemia/reperfusion injury did not cause morphological or biological change. | (21,22) |
| Autologous UTx | ― First pregnancy and delivery after autologous UTx in a primate was achieved. | (23,24,25) |
| Living donor minimally invasive surgery | ― Usage of ovarian veins instead of uterine veins resulted in less invasive donor surgery. | (27) |
| Organ perfusion | ― The technique with perfusion via the femoral or external iliac artery could be useful for UTx assuming the procurement of a uterus from a brain-dead donor. | (28) |
| Allogeneic UTx | ― First pregnancy and delivery after allogeneic UTx in a non-human primate was achieved. | (29-31) |
| Rejection | ― Severe cellular and humoral rejections were observed in the transplanted uterus. ― Rejection diagnostic criteria of the uterus in cynomolgus macaques were established. ― Irreversible rejection of the uterus did not lead to fatal outcomes. | (32,33) |
Uterine blood flow is an important factor in maintaining uterine function, including pregnancy and delivery, and it is not clear which blood vessels are essential for maintaining uterine function. In UTx, the vagina of the donor uterus is cut, and uterine perfusion is performed only by the uterine and ovarian vessels (Fig. 3). We mimicked the blood flow dynamics during UTx by separating the uterus of a cynomolgus macaque from the vagina, leaving the uterus and ovarian vessels in place for uterine perfusion; we then clamped the vessels in various combinations. The uterine vessels responsible for uterine blood flow were examined using indocyanine green (ICG) fluorescence imaging.22 The results suggested that the uterine vessels were significantly related to uterine perfusion, whereas ovarian vessels were not significantly involved. As a limitation of this study, deep uterine veins were not evaluated, which made it difficult to determine exactly which veins (ovarian vessels, uterine vessels, and deep uterine veins) are the main contributors to uterine drainage.
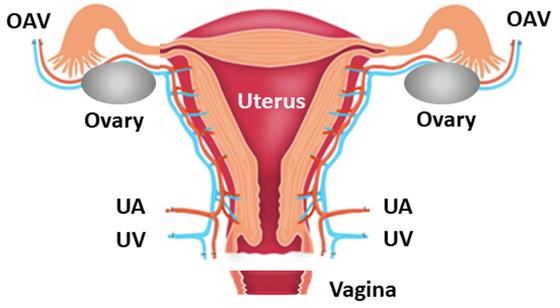
Anatomical characteristics of the blood vessels associated with the uterus. OAV, ovarian artery and vein; UA, uterine artery; UV, uterine vein.
Furthermore, to verify whether pregnancy and childbirth are possible with only the uterine arteries and veins, we exploratively operated on a cynomolgus macaque so that the uterus was perfused with only one side of the uterine arteries and veins, and the fertility of the uterus was examined.23 As a result, menstruation recovered 2 months after the operation, and pregnancy occurred 4 months after the operation. Fetal growth and right uterine arterial blood flow during gestation were normal. Full-term delivery was achieved with nutrition from unilateral uterine vessels, but collateral vessels from the left side were detected by ICG imaging during cesarean section. Our results showed that pregnancy and delivery are supported by a unilateral uterine artery and vein alone with collateral circulation in cynomolgus macaques, with the major limitation of this experiment having been performed only once.
Uterine warm ischemia/reperfusion injuryThe allowable time for warm ischemia of an organ varies depending on the organ and is an important factor affecting the vascular anastomosis time in the recipient, the order of organ removal from a deceased donor, and transfer of the organ; however, the allowable time was unknown for the uterus. Therefore, we investigated the allowable warm ischemic time and morphological and biochemical changes in uterine ischemia/reperfusion injury in cynomolgus macaques.24,25 The uterus was kept connected with ovarian and uterine vessels only, and these were subsequently clamped for 0.5, 1, 2, 4, and 8 h, and then released. Histopathological changes and biochemical parameters were evaluated after each blockage time and after reperfusion. Myometrial biopsy of the uterine body showed mild degeneration after warm ischemia for 4 h, and zonal and atrophic degeneration of smooth muscles after warm ischemia for 8 h. There were no significant changes in biochemical parameters, including lactic acid, anion gap, base excess, and potassium, between before and after reperfusion for 5, 15, and 30 min in each group. In all animals that underwent warm ischemia for up to 4 h, periodic menstruation resumed within 3 months after surgery, but regular menstruation did not recover in the animals that underwent warm ischemia for 8 h. As a result, it was suggested that warm ischemia in the uterus of cynomolgus macaques is tolerated for up to 4 h, and that uterine ischemia/reperfusion injury did not cause morphological or biological changes.
Autologous UTxWhen we started the experiment, there were no reports of pregnancy after autologous UTx in non-human primates. Therefore, our first attempt focused on establishing surgical procedures using autologous orthotopic UTx in cynomolgus macaques, with the goal of first delivery in primates. Since cynomolgus monkeys are very small individuals, delicate surgical procedures and vascular anastomosis were required along with anesthesia management;5 consequently, we experienced many deaths during and after surgery resulting from hemorrhage and inadequate anesthetic management.26,27 In the sixth macaque, menstruation resumed 1 month after surgery, and natural pregnancy was achieved 4 months after surgery. There were no abnormalities in fetal growth or uterine arterial blood flow during pregnancy. Although placental abruption was observed, the first delivery in a primate worldwide was achieved.28 This result led to many advances in UTx research and provided useful data for clinical application.
Living donor minimally invasive surgery of UTxIn UTx from a living donor, the deep uterine vein is mainly used as a drainage vein,29 but because this is a complicated surgical procedure, the burden on the donor, including the operative time and the amount of bleeding, is an important issue to be resolved9; consequently, the development of minimally invasive donor surgery was required. To reduce the risk and with the aim of developing a minimally invasive surgical technique, we verified the usefulness of the ovarian veins instead of the deep uterine veins in the donor surgical procedure in cynomolgus macaques.30 In surgery in cynomolgus macaques that imitated that of a living donor, the surgery time was significantly shorter in the group using the ovarian vein as the vascular pedicles than in the uterine vein group. The amount of intraoperative bleeding was small in all macaques, and no complications such as injury to other organs or blood vessels were observed. It has been suggested that in living donor surgery in cynomolgus macaques, it is possible to provide less invasive surgery by using the ovarian veins rather than the uterine veins and by practicing surgical techniques.
Organ perfusion procedure in brain-dead donorsWhen removing abdominal organs from a brain-dead donor, the current method of perfusing an organ with protective solution is to clamp the aorta and place a perfusion catheter in the lower aorta to perfuse the abdominal organs. However, in UTx, the uterus, located in the pelvis, also needs to be perfused, so the existing procedure had to be revised. We placed a perfusion catheter in the femoral artery or the external iliac artery and examined macroscopically and pathologically whether organ perfusion from these vessels perfused not only the uterus but also the entire abdominal organ.31 With this new organ perfusion procedure, perfusion of the abdominal organs and uterus was macroscopically sufficient. Furthermore, histopathologically, it was confirmed that the blood cell components in the tissues of each abdominal organ, such as the small intestine, liver, pancreas, and kidney, were barely observed, and that the tissues were sufficiently perfused. The technique with perfusion via the femoral or external iliac artery could be useful for UTx, assuming that the uterus was to be procured from a brain-dead donor.
Allogeneic UTxAllogeneic UTx models in non-human primates are very important for preclinical study to investigate medical issues, including suitable immunosuppressants, diagnosis of rejection, uterine antigenicity, and teratogenicity induced by immunosuppressants. There had been no reports of menstrual recovery or pregnancy after allogeneic UTx in non-human primates until we embarked on an allogeneic UTx experiment in macaques. We progressed to allogeneic UTx in cynomolgus macaques after the achievement of the first delivery in an autologous UTx model. In a preliminary study, we interchanged uteri between two animals and performed an orthotopic transplant under different immunosuppressive protocols.32 In one animal, first menstruation after allogeneic UTx in non-human primates was observed, but in the other, uterine atrophy occurred. Thereafter, we decided to perform allogeneic UTx by assuming a brain-dead donor for the purpose of creating a stable model. Longer and thicker vessels, including the common iliac vessels or abdominal aorta/inferior vena cava, were removed from the donors. In recipient surgery, end-to-side anastomosis with the recipient and donor common iliac vessels or abdominal aorta/inferior vena cava was performed. By performing vascular anastomosis with major blood vessels, a stable surgical procedure for allogeneic UTx in cynomolgus macaque was established.33 After menstruation recovered post-surgery, transtubal embryo transfer (ET) through laparoscopy was performed because transvaginal ET was restricted due to cervical canal bending; this prevented the insertion of a catheter into the uterine cavity in cynomolgus macaques. Subsequently, we succeeded in the world’s first pregnancy and delivery after allogeneic UTx in a non-human primate (Fig. 4).34

The first offspring after allogeneic uterus transplantation in a cynomolgus macaque.
We have experienced various severe cases of cellular and humoral rejections induced by donor-specific antibody production in allogeneic UTx models in cynomolgus macaques.34,35,36 Based on this experience, we established our diagnostic rejection criteria for the uterus in a cynomolgus macaque,34 which partially referred to the grading system proposed by a Swedish group for monitoring rejection.37 We believe that rejection of cellular and humoral components is more likely to develop in cynomolgus macaques, whose uteri may exhibit high levels of antigenicity compared with those of humans.34,35 Another concern regarding UTx is whether a uterus with irreversible rejection should be removed. In our experimental series of allogeneic UTx in cynomolgus macaques that were unresponsive to treatment with immunosuppressants, irreversible rejection occurred but the general condition remained good; however, temporary swelling of the uterus was observed by ultrasonography and temporary increases in white blood cells, lactate dehydrogenase, and C-reactive protein were evident. Histopathological findings in the removed uteri showed hyalinized fibrosis, endometrial deficit, lymphocytic infiltration, and vasculitis. These findings suggest that irreversible rejection of the uterus is not fatal, in contrast to the rejection of life-supporting organs.36
To date, 65 UTx procedures have been reported in publications from 12 institutions, with 31 healthy babies born after these procedures.37,38 Thus, UTx research is circulating worldwide and is starting to be recognized as a feasible medical treatment for patients with UFI. However, UTx is not a commonly known medical technique in Japan. We have been providing accurate information to Japanese society and academia through various social and academic activities so that the new technology of UTx might be correctly recognized by Japanese society and conform with the needs of society. As a result, UTx has attracted attention in Japan, and the expectation of clinical application has increased. The activities carried out to explore the possibility of clinical application of UTx in Japan and the social and academic movements resulting from them are described below.
Information disclosure to the public through the homepage of Keio uterus transplantationBefore discussing whether UTx could become an accepted technology for Japanese society, it is necessary to fully recognize the implications of UTx and the medical, social, and ethical issues it faces. With the aim of deepening the public’s awareness of UTx, we continue to disseminate information on our homepage (http://keio-utx.org/, in Japanese) about our UTx research activities, recent reports from around the world, explanations of UTx, and the associated issues. So far, we have received about 200 inquiries from parties who wish to have a UTx or to donate a uterus, and it is hoped that a UTx will be carried out in Japan.
Japan Society for Uterus Transplantation (JSUTx)JSUTx was established by experts involved in UTx research in 2014. The purpose of JSUTx is to deepen exchanges in various fields such as gynecology, obstetrics, reproductive medicine, and transplantation medicine for basic and clinical research on UTx; to improve applicable knowledge about UTx; and to clarify medical, social, and ethical issues. Furthermore, by holding regular academic meetings and public lectures, not only for medical professionals but also for the general public, we will provide a place for understanding and discussing UTx and contribute to the development of new medical technology.
Awareness survey of attitudes toward UTx in reproductive-aged Japanese womenTo clarify the views on UTx for UFI of Japanese women of reproductive age, we conducted a survey through an Internet research company in December 2014 as a cross-sectional study of 3892 randomly chosen women aged 25 to 39 years old.3 In choosing candidates for UTx based on the highest priority, deceased persons (33.8%) and mothers (19.0%) were favored as donors, and women with congenital absence of the uterus (54.4%) and hysterectomy due to a malignant uterine tumor (20.0%) were favored as recipients. Of the respondents, 62.1%, 34.7%, and 18.1% favored adoption, UTx, and gestational surrogacy, respectively. Regarding societal acceptance of UTx, the response rates were 15.7% for “UTx should be permitted,” 77.6% for “UTx should be permitted with discussion,” and 6.7% for “UTx should not be permitted, even with discussion.” Regarding personal opinions on UTx, 44.2% were in favor, 47.5% had no opinion, and 8.3% were against. From these results, it is clear that there are many people who view UTx as socially and personally acceptable, and it is expected that it can become an accepted technology in Japan. A questionnaire survey conducted by a group at Tokyo University in 2017 showed similar results.39 However, it cannot be said that the technology of UTx is fully known to Japanese society, and it is necessary for medical personnel to provide accurate information, including the advantages and disadvantages of UTx, to Japanese society. Further investigations to establish the societal need for UTx in Japan should be carried out.
UTx Working Group at Keio University Hospital and preparation for clinical trialUTx is, in essence, an organ transplant, and transplantation medicine is unfamiliar to obstetricians and gynecologists; consequently, the support of experts in other fields centered on transplant surgery is indispensable for clinical application. Furthermore, not only is organ transplantation a surgical procedure, but postoperative management, including immunosuppressive drugs, is very important. Indeed, fatal outcomes may ensue due to infections caused by immunosuppressive drugs; therefore, careful post-surgery management and the establishment of a clinical research system are required. As a result, in 2016, we established the UTx Working Group at Keio University Hospital consisting of multidisciplinary specialists such as physicians, nurses, pharmacists, and administrators at Keio University Hospital (Fig. 5). The purpose of UTx is to obtain a healthy child, but there are various steps in the process, and careful measures must be taken at each step (Fig. 6). We are aiming for the first clinical trial of UTx in Japan from a multifaceted perspective, with the utmost effort to provide physical, mental, and psychosocial support for donors, recipients, their families, and the children born.
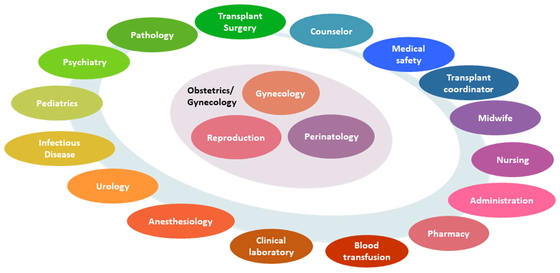
The Working Group at Keio University Hospital.
This group consists of multidisciplinary experts, such as physicians, nurses, pharmacists, and administrative staff.
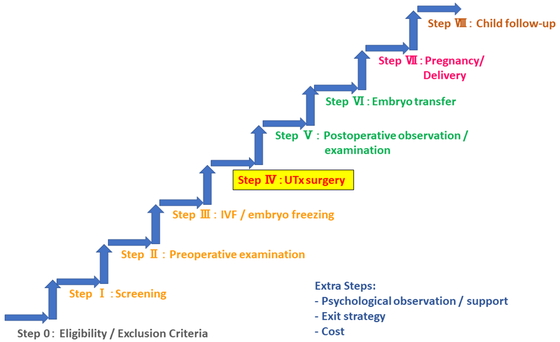
Various steps in the process of producing a healthy child by uterus transplantation.
Because UTx involves various ethical and social issues, discussion and cooperation not only with the implementation facility but also with related medical societies and the Ministry of Health, Labour and Welfare are considered essential for the clinical application of UTx in Japan. Therefore, in 2018, we submitted a draft plan for a clinical trial and a request to the Japan Society of Obstetrics and Gynecology and to the Japan Society for Transplantation for their views on conducting clinical research on UTx in Japan. While societies have sought to develop positions on the ethical and social aspects of UTx, the issue encompasses a wide range of facets for discussion. Therefore, the Japanese Association of Medical Sciences, which presides over all domestic medical societies in Japan, has taken up the role of examining this issue. In April 2018, the Japanese Association of Medical Sciences began investigating the advantages and disadvantages of allowing UTx in the country to pave the way for women without a uterus to become pregnant and give birth. The Association set up a 13-member panel, which included experts in reproductive medicine, medical transplantations, bioethics, sociology, and criminal law. The panel debated the ethical and safety issues associated with UTx for more than 2 years. Finally, the Association published a report in July 2021 concluding that it would approve clinical studies of UTx in Japan. Therefore, our team is currently preparing to apply for permission from the Institutional Review Board at Keio University Hospital and to conduct the first clinical trial of UTx in Japan.
Understanding of the position of MRKHS patientsAlthough the clinical application of UTx has not yet been realized in Japan, MRKHS patients, who are candidates for UTx, have become widely recognized by society. As the situation and circumstances of MRKHS patients have become more deeply understood, gynecologists have been encouraged by the advances of UTx research.40 Previously, MRKHS was not widely recognized, and the required care and counselling for these patients were not familiar to gynecologists; as a result, patients lost the opportunity for hospital consultations because of insufficient support. After MRKHS became more widely recognized in Japan, triggered by UTx research, MRKHS patients have been able to arrange hospital visits for accurate diagnosis and counseling on their relationship with their body. Moreover, several patient groups have been established for communication purposes. Overall, it has become clear that physical and psychological care interventions for these patients are essential, and gynecologists need to become more aware of the condition and more supportive of the patients. In the wake of UTx research, the increased awareness of the situation of patients with MRKHS by the public and gynecologists alike is of great significance to the patients.
Because each country has different medical, ethical, social, and religious backgrounds, thorough discussions are essential prior to UTx trials. As previously reported, the major ethical and social concerns related to UTx in Japan are the risks for donors, comparisons with surrogacy, and opposition to non-vital organ transplantation.41
There are no risks associated with deceased donors, which is clearly an advantage compared to living donors.9,13 However, in Japan, organ transplantations from living donors greatly outnumber those from deceased donors.10,42 There are potential risks associated with a living donor, including complications of the surgery itself, hysterectomy, and the removal of vascular pedicles. Moreover, in cases where ovarian veins are used, oophorectomy is required, resulting in ovarian dysfunction. Therefore, decreased QOL in terms of sexual activity and mental burden should be considered.
Surrogacy is forbidden in Japan because of the many ethical issues.4 However, there is no legal framework for surrogacy. UTx is a very different process from that of surrogacy, although comparisons between the two methods have been debated. Ethically, UTx is more likely to be acceptable than surrogacy in Japan because children born to a surrogate mother may not experience maternal behavior that fully respects the child’s welfare.41
Organ transplantation is an essential means of saving lives, whereas UTx is a procedure to improve the QOL of UFI patients rather than to provide a chance for survival. Therefore, some opposing opinions exist; for example, the notion that organ transplantation should not be conducted solely for the improvement of QOL because complications occasionally lead to death. Specifically, questions regarding the ethics of allowing transplantation therapy to fulfill a woman’s desire for childbirth have been debated.
The new reproductive and organ transplantation technology of UTx for patients with UFI is rapidly proliferating, and in view of the trend of worldwide clinical development, its implementation must be deliberated in Japan as elsewhere. The following are mandatory for the clinical application of UTx: sufficient acquisition and experience of the technology through basic experiments, comprehensive understanding of this technology, thorough discussions and careful organizational systems at implementation facilities and related academic societies, and the formation of social consensus. Furthermore, to evaluate the efficacy and safety of UTx, the procedure should be conducted as a rigorously controlled clinical trial with sufficient deliberation considering ethical, legal, and social issues. This new technology will bring great benefit to uterine infertile women, and it is expected that it will be clinically deployed in Japan in the near future.
The authors declare that no conflicts of interest exist.