Article ID: 2024-0003-OA
Article ID: 2024-0003-OA
Introduction of the robotic stapler has allowed robotic lobectomy to be performed from a surgical console in complete autonomy. The robotic stapler fits a 12-mm port, which is larger than the standard 8-mm port and increases the risk of postoperative pain. However, in many cases, to cover all possible angles of approach, two 12-mm ports are preferably used. However, limiting instrument inventory and simplifying surgical procedures are also desirable to reduce costs. In a multicenter study, we assessed the feasibility of robotic lobectomy with a single type of robotic stapler [SureForm45 Curved-Tip (SF45C); Intuitive Surgical Inc.] inserted through one 12-mm port placed at the anterior tip of the lower intercostal space. We also investigated the potential cost savings of using an additional 60-mm stapler for interlobar division. A total of 135 lobectomy cases were enrolled. In all cases, all stapling procedures were completed using the SF45C inserted from the designated 12-mm port. We found that it was potentially less expensive to use the SureForm60 stapler if more than six SF45C reloads were needed for interlobar division. However, in our series, only 1 case (0.7%) met this requirement. The use of a single type of stapler from one 12-mm port in a robotic lobectomy is technically feasible. This approach may be expected to allow for surgical simplification, minimize the risk of postoperative pain, and reduce inventory costs.
The da Vinci surgical system (Intuitive Surgical Inc., Sunnyvale, CA, USA) has several advantages when compared with conventional thoracoscopic surgical systems, including three-dimensional imaging, a stable camera and operating platform, articulating instruments with seven degrees of freedom, excellent ergonomics, motion scaling, and tremor-free movements.1 However, although stapler division of the hilar pulmonary structures is the most important and potentially dangerous step of the operation, a robotic stapler has not been available for use with the conventional da Vinci Si system. Instead, this task has been delegated to and performed by the bedside assistant.2,3
The introduction of the first robotic stapler [EndoWrist (EW); Intuitive Surgical Inc.] in the da Vinci Xi system made it possible for a Robot-assisted Thoracic Surgery (RATS) lobectomy to be controlled directly by the operating surgeon, who can divide the hilar structures from the robotic console. This development has facilitated the introduction of robotic surgery in the field of general thoracic surgery.2,3
At present, stapling strategies play a significant role in choosing where to place trocars with the da Vinci Xi system. The robotic stapler is a large device and placing the stapling ports as low as possible (i.e., close to the diaphragm) is thought to be advantageous and to allow the greatest degree of maneuverability in the chest cavity. To cover all possible angles, most surgeons place one stapling trocar anteriorly and another posteriorly. Surgeons should also consider that the robotic stapler requires a large 12-mm port even though standard robotic instruments fit through 8-mm ports. Large 12-mm port placement increases the risk of postoperative pain, especially in the narrow posterior intercostal space.4
Despite its utility, the cost of robotic surgery is high. Obviously, there are many stapling options, including the use of both a robotic stapler and a hand-held endoscopic linear stapler (ELS) by a bedside assistant. Limiting the range of instruments, including staplers, and simplification of the surgical procedure are required to reduce the inventory cost and operating times for the sustainable development of robotic surgery.5
The newest robotic stapler [SureForm (SF); Intuitive Surgical Inc.] has a 120-degree cone of articulation, which is much wider than the conventional EW robotic stapler, the articulation of which is elliptical (i.e., 108 degrees left to right and 54 degrees up and down). This improvement may allow surgeons to complete the entire stapling procedure with a single 12-mm stapler port placed in an anterior intercostal space. In addition, given that anterior intercostal spaces are larger than posterior intercostal spaces, this approach may reduce the risk of postoperative pain. Based on the issues described above, we assessed the feasibility of using a single type of stapler (SureForm45 Curved-Tip, SF45C) inserted through one 12-mm port to perform robotic lobectomy in a multicenter setting.
All study procedures were conducted in accordance with the Declaration of Helsinki and its later amendments. This study was approved by the Ethics Review Committee of the Saiseikai Yokohama-shi Tobu Hospital (referral number 20210215), Southern Tohoku General Hospital (referral number 544), Showa University (referral number 2023–193-B), and Shin-Yurigaoka General Hospital (referral number 20230828–2).
Given the retrospective nature of the study, the opt-out approach was used to provide consent. Only anonymized data were included in the customized database.
InstitutionFour institutions participated in this study: Saiseikai Yokohama-shi Tobu Hospital, Southern Tohoku General Hospital, Showa University, and Shin-Yurigaoka General Hospital. Robotic lobectomies performed at participating institutions between April 2020 and February 2022 were included and operation data were retrospectively collected and studied. Case selection for robotic lobectomy was left to the individual institutions. During this period, all the participating institutions had introduced robotic lobectomy under the supervision of the corresponding author (M.O.). Each institution used the same port, instruments, and stapler strategy as described below.
Port placementWe utilized the RPL-4 approach (robotic portal lobectomy with four arms) with carbon dioxide insufflation using the da Vinci Xi surgical system (Fig. 1).6 Patients were placed in a lateral decubitus position and were managed with general anesthesia and double lumen intubation. Three 8-mm ports were placed in the same intercostal space. More specifically, they were placed in the sixth intercostal space for upper lobectomies and in the seventh intercostal space for middle and lower lobectomies. A 12-mm stapling port was placed as far anteriorly as possible, usually one interspace below the other three ports. In this study, in principle, all the stapling procedures were performed from this 12-mm port using the SF45C with a white up to a black reload. A 12-mm AirSeal (ConMed, Utica, NY, USA) assist port was inserted in the anterior tenth intercostal space.

Examples of port strategy: right and left upper lobectomies.
Three 8-mm ports are placed in the same intercostal space: specifically, in the sixth intercostal space for upper lobectomies and in the seventh intercostal space for middle and lower lobectomies. A 12-mm port for the robotic stapler is placed as far anteriorly as possible on the bottom of the thoracic cavity, in the seventh or eighth intercostal space. In principle, all staple procedures were performed from this 12-mm port using a SureForm45 Curved-Tip (SF45C).
Lobectomy data were collected using a questionnaire. The questionnaires were sent to the coauthors at each institution. The completed questionnaires were then returned to the lead author (Y.I.) by E-mail.
The complete survey included the following information for each lobectomy:
Investigation of potential cost saving by using additional 60-mm stapler
The thoracic cavity is much narrower than the abdominal cavity. Therefore, from the standpoint of maneuverability and safety, the use of a 45-mm stapler, rather than a 60-mm stapler, is appropriate for division of the hilar structure. However, there is a potential cost advantage to the added use of a 60-mm stapler for obliterated interlobar division instead of using a 45-mm stapler alone. Therefore, we estimated and compared the cost of completing the entire procedure using the SF45C alone and adding the SF60 for interlobar fissure division. The potential advantages of using the SF60 in clinical practice were considered.
The potential cost savings from the added use of the SF60 were assessed as follows: if X and Y represent the respective numbers of SF45C and SF60 stapler reloads required for interlobar division, and the catalog cutline lengths of SF45C and SF60 are 40 mm and 55 mm, respectively, when X reloads of the SF45C are required to cut the interlobar tissue, X−1 reloads of the SF45C are insufficient to cut the tissue. This condition can be expressed in the inequality:
40×(X−1) < Tissue lengthWhen the tissue can be cut with Y reloads of the SF60, the following inequality holds:
Tissue length < 55 × YTherefore, the condition for tissue length is:
40 × (X−1) < Tissue length < 55 × YIf the difference between 40 × (X−1) and 55 × Y is too small, this inequality will almost never be satisfied, making it impractical.
Therefore, assuming that the difference in staple length (safety margin) between X−1 reloads of the SF45C and Y reloads of the SF60 is at least 10 mm (Fig. 2), the relationship between X and Y is:
40 × (X−1) < 55 × Y+10 (1)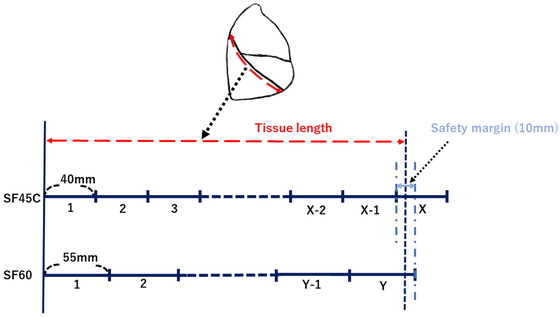
The conditions under which a 60-mm stapler (SF60) was used instead of a 45-mm stapler (SF45C).
For example, an SF60 was used for an oblique fissure division during a right lower lobectomy. X and Y represent the respective number of SF45C and SF60 stapler reloads required for interlobar division, and the cutline lengths of SF45C and SF60 are 40 mm and 55 mm, respectively. We set a safety margin of 10 mm for the cutline length between X−1 reloads of the SF45C and Y reloads of the SF60.
The SF45C and SF60 stapler shafts each cost 35,000 yen (US 233.30 at an exchange rate of 150 yen to the dollar). Stapler reloads cost 31,000 yen for SF45C and 34,000 yen for SF60 (206.70 and 226.70, respectively).
If using SF45C and SF60 together is cheaper than using SF45C alone, the following inequality holds:
31,000 × X > 35,000 + 34,000 × Y (2)We investigated the potential cost saving by the use of an additional 60-mm stapler by identifying the proportion of cases that may satisfy these simultaneous inequalities.
Exclusion criteriaThe following cases were excluded from this study: those in which surgery was performed by other robotic port approaches; cases in which staplers other than the SF45C were used for non-technical reasons; and cases that required conversion to another approach [i.e., conventional video-assisted thoracic surgery (VATS) and/or open thoracotomy].
Of the 163 cases collected, 28 were excluded because staplers other than SF45C were used for non-technical reasons (out of stock or because of inventory clearance). All stapling procedures in these 28 cases were completed by using a robotic stapler inserted through the designated anterior inferior 12-mm port. A hand-held ELS was not used.
No operations were performed by other robotic port approaches. No cases were converted to VATS or open thoracotomy. Consequently, a total of 135 cases of robotic lobectomy were enrolled (Shin-Yurigaoka General Hospital, 35; Saiseikai Yokohama-shi Tobu Hospital, 45; Southern Tohoku General Hospital, 37; Showa University Hospital, 18).
All stapling procedures were completed using the SF45C inserted through the designated anterior inferior 12-mm port. The 135 surgical procedures included 44 right upper lobectomies, 18 right middle lobectomies, 33 right lower lobectomies, 20 left upper lobectomies, and 20 left lower lobectomies. The numbers of reloads required for each surgical step (vessel division, bronchial division, and interlobar division) and for the overall operation according to type of lobectomy are listed in Table 1.
| Lobectomy type | Hilar vessel division | Bronchial division | Interlobar division | Overall procedure |
|---|---|---|---|---|
| Right upper (n=44) | 3 [1–5] | 1 [1–2] | 3 [0–6] | 7 [4–11] |
| Right middle (n=18) | 2.5 [1–5] | 1 [1] | 3 [1–5] | 6.5 [4–10] |
| Right lower (n=33) | 2 [1–4] | 1 [1] | 2 [0–5] | 5.5 [3–9] |
| Left upper (n=20) | 4 [2–6] | 1 [1–2] | 1.5 [0–5] | 7 [4–11] |
| Left lower (n=20) | 3 [2–4] | 1 [1] | 2 [0–5] | 6 [3–9] |
| Overall (n=135) | 3 [1–6] | 1 [1–2] | 2 [0–6] | 6 [3–11] |
Data are shown as median [range].
For hilar vessel division, the number of stapler reloads (median [range]) required per case was 3 [1–5] during right upper lobectomy, 2.5 [1–5] during right middle lobectomy, 2 [1–4] during right lower lobectomy, 4 [2–6] during left upper lobectomy, and 3 [2–4] during left lower lobectomy. Considering all lobectomies, 3 [1–6] stapler reloads were required for hilar vessel division.
For bronchial division, 1 [1–2] stapler reload was required during right upper lobectomy or left upper lobectomy and 1 [1] was required during right middle lobectomy, right lower lobectomy, or left lower lobectomy. Considering all lobectomies, 1 [1–2] stapler reload was required for bronchial division.
For interlobar division, 3 [0–6] stapler reloads were required during right upper lobectomy, 3 [1–5] during right middle lobectomy, 2 [0–5] during right lower lobectomy or left lower lobectomy, and 1.5 [0–5] during left upper lobectomy. Considering all lobectomies, 2 [0–6] stapler reloads were required for interlobar division.
Based on all procedures, 7 [4–11] stapler reloads were required during right or left upper lobectomy, 6.5 [4–10] during right middle lobectomy, 5.5 [3–9] during right lower lobectomy, and 6 [3–9] during left lower lobectomy. Overall, 6 [3–11] stapler reloads were required during all lobectomies.
In examining the potential cost savings of using an additional 60-mm stapler, Figure 3 shows the range for which the simultaneous inequalities (1) and (2) are valid. If the SF45C requires more than six reloads to divide the interlobular fissure, it may be more economical to switch to the SF60. In our series, only one case (0.7%) met this requirement. This particular case was a right upper lobectomy that required six stapler reloads for interlobar division. However, replacing the SF45C with the SF60 in such situations would reduce costs by only 15,000 yen per case ($100).

The area in which inequalities (1) and (2) hold, where X and Y are both positive integers.
The positive integers that satisfy these inequalities are indicated by the highlighted dots.
The development of the first robotic stapler, which was only available on the da Vinci Xi robotic system, was a major technological leap and facilitated the introduction of robot-assisted technology in thoracic surgery.2 Before the development of the robotic stapler, inexperienced assistants who had to staple vessels using a hand-held ELS were a potential risk factor for intraoperative catastrophic bleeding during major lung resection.2 Therefore, many thoracic surgeons were reluctant to adopt robots in clinical practice. However, the introduction of the robotic stapler made it possible to perform a complete robotic lung resection without entrusting hilar structure division to inexperienced assistants.
Robotic staplers fit 12-mm robotic ports and are larger than standard robotic instruments that fit 8-mm ports; therefore, their use may increase the risk of postoperative pain. Nevertheless, many surgeons prefer to place two 12-mm ports (one anterior and one posterior) to accommodate virtually all stapler angles for the division of any structure.4 This trend may be partly attributed to the fact that the traditional robotic stapler (EW) is not sophisticated in terms of operability. In comparison, the latest robotic stapler (SF) has a wider range of motion and improved operability. Therefore, the use of two 12-mm ports might not always be necessary.5 However, among the many stapler options, including use of the hand-held ELS, inventory management could be simplified by exclusive use of the SF45C, which has superior maneuverability. These issues motivated us to investigate the feasibility of using a single type of stapler (SF45C) from a single 12-mm port for robotic lobectomy. The following results were obtained:
In conclusion, using a single type of stapler (SF45C) inserted through a single 12-mm port is a technically feasible means of performing robotic lobectomies, and it is more cost effective than added use of the SF60 for interlobar fissure in most cases. This approach may be expected to provide surgical simplification, minimize the risk of postoperative pain, and reduce inventory costs.
This study had some limitations. It was a retrospective single-arm study, and only an initial small number of cases were enrolled after the introduction of robotic surgery. Case selection was delegated to each institution. Consequently, cases with a complete fissure and were technically easy tended to be selected. However, an additional 60-mm stapler (SF60) may be less expensive in cases of a largely fused fissure, which would seldom have been selected in our series. Further research will be needed to determine the appropriate use of the SF60.
In terms of postoperative pain, we assume that our single 12-mm port strategy is superior to a multiple 12-mm port strategy. However, there is no evidence as to whether the number or location of intercostal 12-mm ports is related to postoperative pain. A detailed comparative study using a large sample size will be needed to determine whether postoperative pain is related to the number and location of intercostal ports.
Makoto Oda has delivered lectures on behalf of Intuitive Surgical Inc. (Sunnyvale, CA, USA). The remaining authors declare no conflict of interest.