2023 Volume 10 Pages 87-92
2023 Volume 10 Pages 87-92
Various approaches to lumbar interbody fusion have been described. The usefulness of full-endoscopic trans-Kambin's triangle lumbar interbody fusion has recently been reported. This technique has several advantages in patients with degenerative spondylolisthesis, including the ability to improve symptoms without decompression surgery. Moreover, given that the entire procedure is performed percutaneously, it can be performed without increasing the operation time or surgical invasiveness, even in obese patients. In this article, we discuss these advantages and illustrate them with representative cases.
Various surgical methods for lumbar interbody fusion (LIF) have been reported, including anterior LIF (ALIF), lateral LIF (LLIF), transforaminal LIF (TLIF), and posterior LIF (PLIF). Full-endoscopic surgery has recently been applied in various degenerative diseases, and Sairyo et al. reported a surgical procedure for performing interbody fusion using a full-endoscopic lumbar discectomy system through Kambin's triangle, known as trans-Kambin's triangle LIF (KLIF).1-5)
We believe that KLIF surgery has a number of benefits, one of which is that it can decompress spinal canal stenosis in patients with degenerative spondylolisthesis without the need for open surgery. LLIF can also be performed for indirect decompression. However, in LLIF, the intervertebral cage is inserted before the insertion of the pedicle screws, which can make it difficult to reduce slip using a pedicle screw system and to perform LLIF for Meyerding grade 2 or higher degenerative spondylolisthesis. Conversely, in KLIF surgery, which entails dilating the intervertebral disc space with dedicated tools, reducing the slip with percutaneous pedicle screws, and finally inserting the intervertebral cage, percutaneous pedicle screws can be used for reduction, and patients with Meyerding grade 2 or higher degenerative spondylolisthesis are candidates for KLIF. This report outlines the advantages of KLIF surgery and presents some illustrative cases.
Surgical procedure 1. Harvesting bone for autografting from the ilium or spinous processThe entire surgical procedure is performed with electrophysiological monitoring for safety. The first step is to harvest bone for autografting from the ilium or a spinous process.
2. Percutaneous pedicle screw insertionPercutaneous pedicle screws are inserted under C-arm fluoroscopic guidance (Supplementary Figure 1). In a patient with spondylolisthesis, the rod is fixed to the caudal screw, with the cranial rod floating from the screw, and the cranial screw is used as a reduction screw.
3. Full-endoscopic foraminoplasty and preparation of the endplateAfter discography using indigo carmine, the cannula of a full endoscope (Karl-Storz, Tuttlingen, Germany) is then placed safely in Kambin's triangle (Supplementary Figure 2). The superior articular process is partially removed using a surgical drill until the triangle is large enough for the safe insertion of the box-type dilator to be used in the next step. The aim of osteotomy is to remove the amount of bone required to expose 12 mm or more of the surface of the intervertebral disc. The disc materials are then shaved and curetted via full endoscopy. The endoscopic procedure ends here.
4. Insertion of a retractor to prevent exiting nerve root injurySubsequent procedures are basically performed under fluoroscopy. The insertion of the tools for the next step is performed via the skin incision for endoscopic insertion (surgical procedure 3). The next step is to insert the guidewire into the intervertebral disc (Supplementary Figure 3). Box-type dilators of different lengths and widths can be inserted through the guidewire. The smallest dilator is 8 mm × 10 mm, and the 8-mm side is inserted vertically into the disc and rotated by 90° within the disc. It then becomes possible to open the intervertebral disc by up to 10 mm. If there is still room in the disc space, a dilator measuring 10 mm × 12 mm can be used to further increase the disc height. At this point, the slip can be reduced while maintaining the opened height by fastening the rod and pedicle screw on the cranial side. Subsequently, an open-type retractor is inserted. With these procedures, in addition to completely protecting the nerve root, the disc height is widened, further slip is corrected, and the subsequent step can be performed.
5. Intradiscal procedure, including the preparation of the endplate, bone grafting, and insertion of the intervertebral cageThe disc materials are then shaved and curetted using an open-type retractor (Supplementary Figure 4). The endoscope is reinserted to confirm that the endplate cartilage bleeds after it is scratched. A bone graft is then performed, and the intervertebral cage is inserted. Finally, the screw and rod are bonded.
6. SuturesThe fascia and skin are closed using absorbable sutures (Supplementary Figure 5).
The consent for publication of these cases was obtained from all patients.
Case 1: Meyerding grade 1 spondylolisthesisThe patient was a 57-year-old man with a 2-year history of low back pain and right leg pain and intermittent claudication at a distance of more than 200 m (Fig. 1). He was referred to our hospital when conservative management failed to improve his symptoms.
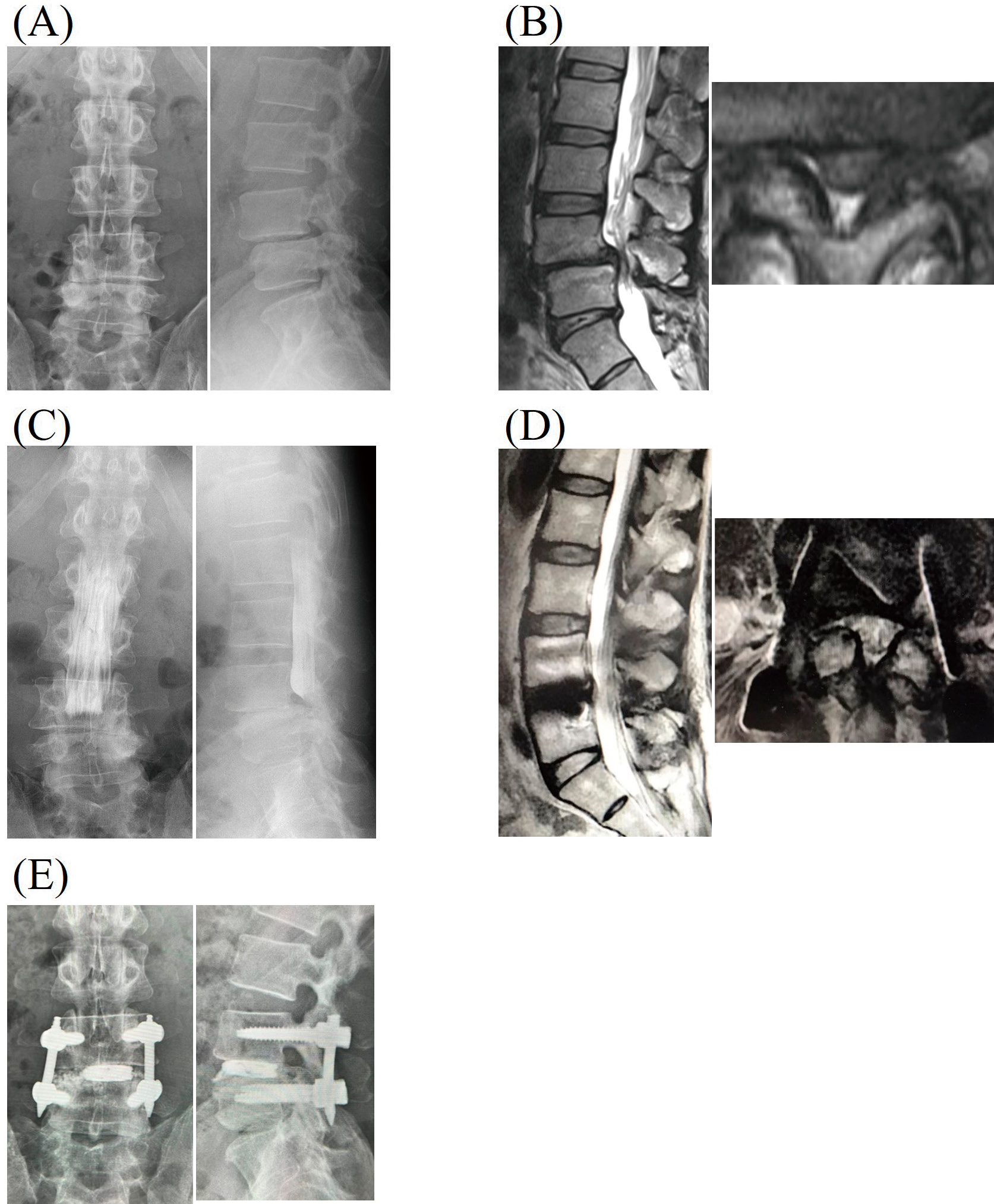
(A) Plain radiograph showing Meyerding grade 1 spondylolisthesis at L4. (B) T2-weighted magnetic resonance image (MRI) revealing spinal canal stenosis at L4/5. (C) Preoperative myelography. (D) Postoperative T2-weighted MRI confirming the expansion of the spinal canal at L4/5. (E) Postoperative radiograph showing the reduction of the slippage at L4/5.
Physical examination did not reveal any muscle weakness, and his reflexes and sensory examination were normal. A radiograph showed Meyerding grade 1 degenerative spondylolisthesis at L4/5 and spinal canal stenosis at L4/5. Myelography showed complete block at L4-5. Thus, we diagnosed his symptoms as right L5 radicular pain due to lateral recess stenosis at L4/5. KLIF was performed at L4/5 without spinal decompression using the surgical procedure described above. Operation time was 2 h 18 min with blood loss of 55 mL. Reduction of the slip at L4/5 relieved the complete block at this level.
His symptoms disappeared immediately after surgery. Postoperative radiographs confirmed that the slip at L4 was reduced completely, and magnetic resonance image (MRI) showed resolution of the spinal canal stenosis. He was asymptomatic at the final follow-up visit 1 year postoperatively. The Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) scores preoperatively and at the final follow-up were 43, 42, 86, 43, and 57 and 100, 100, 100, 100, and 96 for Low back pain, Lumbar function, Walking ability, Social life function, and Mental health, respectively.
Case 2: Meyerding grade 2 spondylolisthesisAn 81-year-old woman with a 3-year history of low back pain and right leg pain was referred to our hospital when conservative management resulted in no improvement (Fig. 2).

(A) Preoperative plain radiograph showing Meyerding grade 2 spondylolisthesis at L4. (B) T2-weighted MRI revealing spinal canal stenosis at L4/5. (C) Postoperative plain radiograph showing a change in spondylolisthesis from Meyerding grade 2 to grade 1.
There was no muscle weakness on physical examination, and her reflexes and sensation were normal. Radiography showed Meyerding grade 2 degenerative spondylolisthesis at L4, and MRI showed spinal canal stenosis at L4/5. Thus, we diagnosed her symptoms as right L5 radicular pain due to lateral recess stenosis at L4/5.
KLIF was performed at L4/5 without spinal decompression using the surgical procedure described above. The operation time was 2 h 23 min with blood loss of 43 mL. The patient's postoperative course was good, and her symptoms disappeared immediately after surgery. Postoperative radiographs showed that the slip at L4 was reduced from grade 2 to grade 1 spondylolisthesis. Her symptoms improved at the final follow-up visit 6 months postoperatively. The JOABPEQ scores evaluated preoperatively and at the final follow-up were 43, 42, 29, 38, and 21 and 71, 83, 49, 65, and 49 for Low back pain, Lumbar function, Walking ability, Social life function, and Mental health, respectively.
Case 3: A severely obese patientThe patient was a 50-year-old woman who complained of a 6-month history of low back pain and left thigh pain (Fig. 3). Her body weight was 90 kg and her height was 154 cm, giving a body mass index (BMI) of 38.0. She was referred to us after failure of conservative management.

(A) Preoperative plain radiograph showing Meyerding grade 1 spondylolisthesis at L3. (B) T2-weighted MRI revealing left foraminal stenosis at L3/4 (arrow) with thick subcutaneous fat (double arrow). (C) Postoperative dynamic plain radiograph showing the reduction of the slippage at L3/4. (D) Postoperative T2-weighted MRI revealing the enlargement of the foramen at L3/4, and fat tissue around the L3 exiting nerve root was observed (arrow).
On physical examination, there was no muscle weakness, and reflexes and sensation were normal. Radiography showed Meyerding grade 1 degenerative spondylolisthesis at L3, and MRI revealed left foraminal stenosis at L3/4 with lumbar disc herniation. Thus, we diagnosed the leg pain as left L3 radicular pain due to foraminal stenosis at L3/4 and the low back pain as being due to the instability at L3/4.
KLIF was performed at L3/4 without spinal decompression using the same surgical procedure described above. The operation time was 2 h 20 min with blood loss of 60 mL. The patient's postoperative course was good, and her symptoms disappeared immediately after surgery. Postoperative radiography confirmed that the slip at L3 was reduced completely and that the foramen at L3/4 was expanded. She was asymptomatic at the final follow-up visit 1 year later. The JOABPEQ scores evaluated preoperatively and at the final follow-up were 0, 8, 29, 38, and 45 and 100, 75, 100, 100, and 69 for Low back pain, Lumbar function, Walking ability, Social life function, and Mental health, respectively.
Full-endoscopic discectomy, which was initially developed by Yeung and Tsou for lumbar disc herniation,6) is a minimally invasive procedure that is now used to treat foraminal stenosis and lateral recess stenosis.1,7-9) Lumbar interbody fixation can now be performed by full-endoscopic discectomy using the procedure named KLIF by Sairyo et al.2)
Various types of LIF have been reported, including ALIF, LLIF, TLIF, and PLIF. There has been a recent report describing the use of LLIF to treat adult spinal deformity because of its indirect decompressive effect, less surgical invasiveness and blood loss, and strong corrective force.10) Indirect decompression in spinal surgery refers to the decompression of spinal nerve tissues, namely, the spinal cord and nerves, without the resection of the tissue causing the compression, such as a hypertrophic ligamentum flavum or intervertebral disc.11,12) This is achieved by reducing the bulging of the intervertebral disc and debulking the ligamentum flavum and posterior longitudinal ligaments by the enlargement of the disc height and reduction of the slip. Whether or not decompression has been successful can be confirmed by checking whether the contrast medium had passed through the stenosed site into the area of the defect on intraoperative myelography.13) However, the disadvantage of indirect decompression using LLIF is that a large intervertebral cage must be inserted before screw fixation. Therefore, it is difficult to reduce the slip using a pedicle screw system, and it is difficult to insert the intervertebral cage if the patient has Meyerding grade 2 degenerative spondylolisthesis.
We consider that KLIF compensates for the disadvantages of the indirect decompression of LLIF in that the slip can be reduced by a pedicle screw after shaving and curetting the disc material via full endoscopy. It is then possible to insert the intervertebral cage after the reduction of the slip using the pedicle screw system. In other words, it is easier to reduce the slippage to the original anatomical state by KLIF than by LLIF. We refer to this surgical effect as "in anatomical situ decompression." KLIF has the further advantage of allowing the insertion of the intervertebral cage after reducing the slip, which makes it possible to operate on degenerative slip disease exceeding grade 2, which cannot be treated by LLIF.
KLIF is also beneficial in obese patients. So far, we have performed KLIF in two obese patients with BMIs of 38 and 37. The size of the skin incision required for an obese patient is the same as that for a nonobese patient because all procedures are performed percutaneously. In conventional open surgery, the heavier the patient is, the larger is the skin incision needed and the more difficult is the surgery to perform. Reviewing the 40 KLIF operations that we have performed to date (data not shown), the operation time was 2 h 15 min in 10 patients with BMI 20-25 and 2 h 20 min in 2 patients with BMI ≥ 35, with blood loss of 46 and 54 mL, respectively. Therefore, in obese cases, KLIF has advantages for not only the patient but also the operator.
Furthermore, LLIF is associated with an increased risk of potentially lethal damage to major organs and blood vessels.14) KLIF may be preferable to LLIF in patients with degenerative spondylolisthesis affecting a single level.
Finally, because the entire KLIF procedure can be performed percutaneously, there may be less risk of infection. The infection rate associated with pedicle screw fixation is lower with a percutaneous approach than with an open approach.15,16) At this time, approximately 200 KLIF surgeries have been performed at our affiliated institutions, and there have been no cases of infection thus far.
However, there are some cases in which other intervertebral fusion techniques are preferable to KLIF. First, in patients with degenerative spondylolisthesis at L5/S1, the pelvis is often an obstacle and it may be difficult to insert the cage in the correct place. Second, in view of the operation time and corrective force required, LLIF may be preferable to KLIF when correction of multilevel vertebral deformity is required. Finally, in cases requiring posterior decompression, PLIF or TLIF would be preferable. Examples include cases with ossification of ligamentum flavum and cases with significant thickening of ligamentum flavum that makes it difficult to achieve symptomatic improvement with indirect decompression.
In conclusion, KLIF can be effective in patients with degenerative spondylolisthesis when decompression surgery is not required.
None declared.