2023 Volume 10 Pages 41-45
2023 Volume 10 Pages 41-45
Several studies have reported the coexistence of chronic subdural hematoma (CSDH) and dural arteriovenous fistula (DAVF); however, the association between these two entities remains unknown. A case of coexisting CSDH and DAVF that was successfully treated with burr hole surgery and middle meningeal artery (MMA) embolization is reported herein. We visualized the positional relationship between CSDH and DAVF by fusion three-dimensional computer graphics images reconstructed from multimodal imaging studies, which revealed that the shunt point of the DAVF was far from the burr hole and was in contact with the CSDH membrane at the center of the CSDH. Additionally, the chronological development of CSDH in the presence of DAVF and the complete disappearance of both DAVF and CSDH after MMA embolization were also demonstrated. This study suggests a possible association between recurrent CSDH and DAVF.
Chronic subdural hematoma (CSDH) is a common disease in neurosurgical practice and is characterized by the collection of blood products in the subdural space, along with the formation of membranes with abnormal neovessels.1,2) Meanwhile, dural arteriovenous fistula (DAVF) is a vascular entity that consists of direct pathologic connections between meningeal arteries and dural venous sinuses or leptomeningeal veins.3-5) Several studies have presented cases of coexisting CSDH and DAVF. However, the association between both entities remains unclear. Herein, we report a case of coexisting CSDH and DAVF. The imaging findings and clinical course indicate that the DAVF contributed to the formation of CSDH, and this study provides insights into the pathogenesis and treatment of both CSDH and DAVF.
An 81-year-old man without a specific history of head trauma was incidentally diagnosed with asymptomatic left CSDH (Fig. 1A) and conservatively observed. However, his CSDH increased in size with mild right hemiparesis one month later, and he underwent burr hole irrigation and drainage for the left CSDH (Fig. 1B). He was discharged without any neurological deficit; however, deep vein thrombosis (DVT) of the lower extremity was detected based on a high D-dimer level during admission for CSDH. Anticoagulant therapy was recommended to prevent pulmonary thromboembolism, but it was postponed due to the risk of CSDH recurrence. However, he experienced mild right hemiparesis again one month after the initial surgery, and computed tomography (CT) revealed recurrence of the left CSDH (Fig. 1C). The patient underwent second burr hole irrigation and drainage procedure (Fig. 1D). Considering the need for systemic anticoagulation for DVT, we scheduled left middle meningeal artery (MMA) embolization the next day to prevent CSDH recurrence.

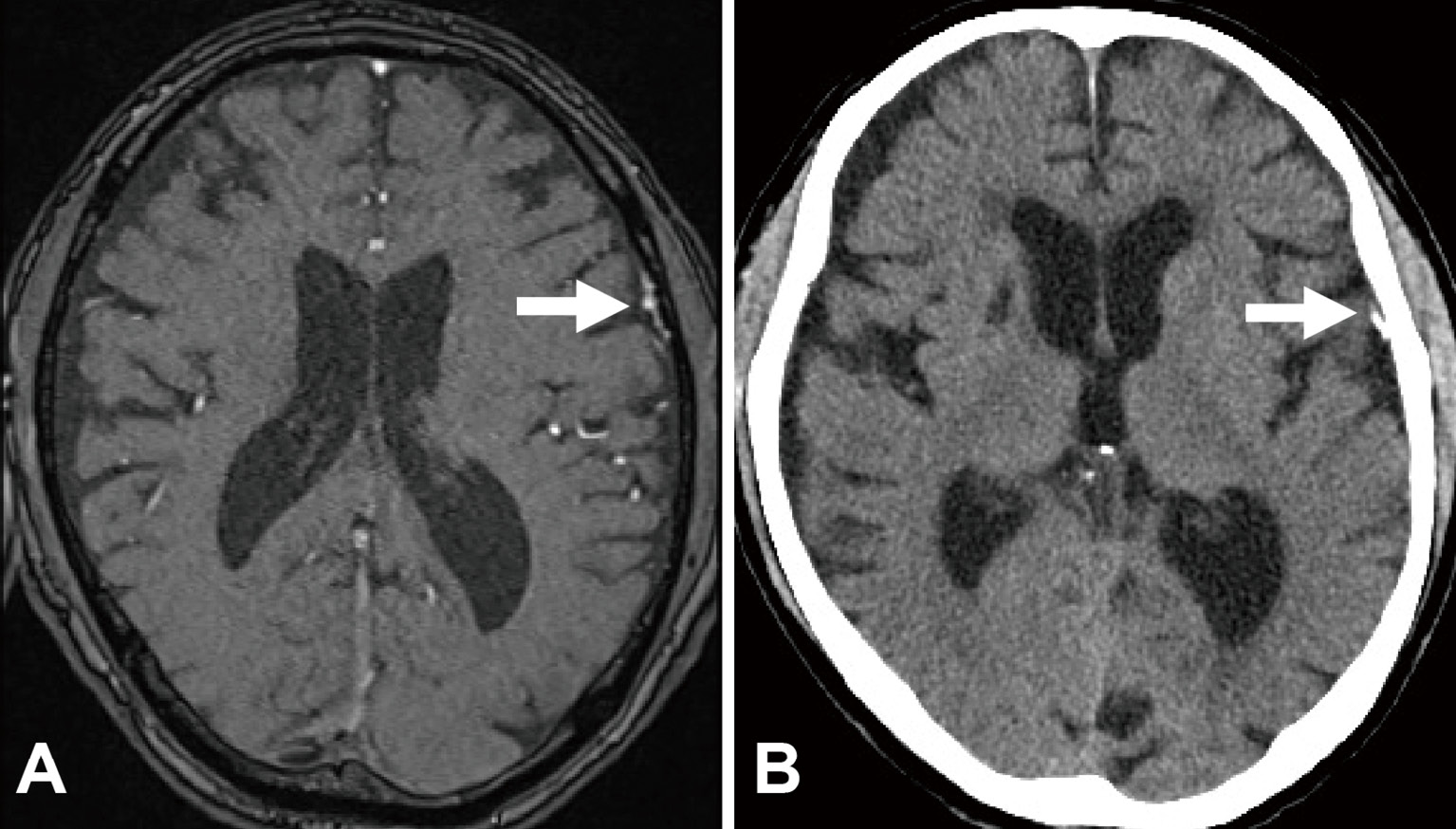
Clinical course of the patient's chronic subdural hematoma.
A. A left chronic subdural hematoma was detected on magnetic resonance imaging during a medical check-up.
B. Computed tomography on postoperative day 1 after the first burr hole surgery for the left chronic subdural hematoma, which was performed one month after the first magnetic resonance imaging examination.
C. Computed tomography revealed the recurrence of the left chronic subdural hematoma one month after the first burr hole surgery.
D. Computed tomography on postoperative day 1 after the second burr hole surgery for the left chronic subdural hematoma.
During MMA embolization, cerebral angiography revealed a left convexity DAVF immediately beside the CSDH cavity. The feeders of the DAVF were the anterior convexity branches of the MMA, and the drainers were the sylvian veins (Fig. 2A). The DAVF was diagnosed as Borden type III and Cognard type III. Furthermore, cerebral angiography revealed faint staining at the shunt point of the DAVF (Fig. 2B). Considering the possibility that the DAVF could increase meningeal blood flow and could therefore cause CSDH recurrence after burr hole surgery, the DAVF was selectively embolized with N-butyl-2-cyanoacrylate. The shunt point of the DAVF was adequately occluded (Fig. 2C, D). The patient's past magnetic resonance imaging findings after embolization was retrospectively reviewed, and DAVF was confirmed in the image obtained five years before the appearance of CSDH (Fig. 3A).

Cerebral angiography and middle meningeal artery embolization.
A. Anteroposterior view of the left external carotid artery angiography revealed a left convexity dural arteriovenous fistula. The feeders were the anterior convexity branches of the middle meningeal artery (white arrow) and drainers were the sylvian veins (white arrowhead).
B. Lateral view of the left external carotid artery angiography showed a faint stain at the shunt point of the dural arteriovenous fistula (black arrow).
C. Lateral view of selective angiography of the left middle meningeal artery during middle meningeal artery embolization.
D. Lateral view of the left external carotid artery angiography demonstrated that the dural arteriovenous fistula was occluded.
Chronological changes in cerebral imaging.
A. The dural arteriovenous fistula (white arrow) was retrospectively confirmed on a magnetic resonance imaging examination performed during a medical check-up five years before the appearance of the chronic subdural hematoma.
B. A follow-up computed tomography at five months post-embolization showed complete disappearance of the chronic subdural hematoma. The embolization material, N-butyl2cyanoacrylate, had well penetrated to the shunt point of the dural arteriovenous fistula (white arrow).
Systemic anticoagulation with apixaban for DVT was initiated on postoperative day 1. The patient recovered well and was discharged without complications. A follow-up CT examination at five months post-embolization showed complete disappearance of both the DAVF and CSDH, and the patient remained symptom-free (Fig. 3B). To intricately investigate the spatial relationship between the DAVF and CSDH, fusion three-dimensional computer graphics (3DCG) images were reconstructed using GRID 1.1 software (Kompath Inc., Tokyo, Japan). This application provides automatic image registration for multiple imaging studies using normalized mutual information.6) The 3DCG examinations revealed that the shunt point of the DAVF was far from the burr hole (Fig. 4A); moreover, it was in contact with the outer membrane of CSDH (Fig. 4B). The DAVF was almost at the center of the CSDH; however, there was no hematoma at the shunt point.

Fusion three-dimensional computer graphics integrating magnetic resonance imaging and three-dimensional rotational angiography.
A. Fusion three-dimensional computer graphics image showing that the shunt point of the dural arteriovenous fistula (red arrow) was far from the burr hole (red arrowhead).
B. Fusion three-dimensional computer graphics image showing that the shunt point of the dural arteriovenous fistula was in contact with the outer membrane of chronic subdural hematoma membrane (red arrow).
Fusion three-dimensional computer graphics images were reconstructed using GRID 1.1 software (Kompath Inc., Tokyo, Japan).
A case of coexisting CSDH and DAVF successfully treated with MMA embolization after burr hole surgery and providing unique imaging findings was reported. The cause and significance of these unique imaging findings are discussed with respect to the clinical course. Through analysis of the fusion 3DCG images, we infer the putative association between CSDH and DAVF.
The CSDH pathogenesis is based on the formation of membranes with abnormal vessel networks promotes a positive feedback cycle of continued hemorrhage, inflammation, and angiogenesis, which results in subdural collection of blood.7,8) The pathogenesis of DAVF remains unclear, but it has been suspected to involve progressive dural venous sinus stenosis or thrombosis with secondary angiogenesis.9) The pathogenesis of both entities involves angiogenesis, but the association between CSDH and DAVF remains uncertain. Several cases of coexisting CSDH and DAVF have been reported, and these have been described as idiopathic or iatrogenic secondary to burr hole surgery.10-15) Tabibian et al. reported that a DAVF was found incidentally in 3 of 30 cases of MMA embolization for CSDH.15) Currently, no study has indicated that a DAVF can contribute to the formation of CSDH.
The mechanism of CSDH enlargement is considered to be repeated bleeding from abnormal vessels in the outer membrane of CSDH. MMA embolization for CSDH could prevent the enlargement and recurrence of CSDH by decreasing the blood supply to abnormal vessels in the CSDH membrane.16,17) Sam et al. reported that MMA embolization also leads to a reduction in the hematoma volume of residual CSDH after burr hole surgery.18) Additionally, the faint staining of abnormal vessels (called cotton wool-like staining) is observed along the CSDH membrane on selective MMA angiography.19-22)
Notably, cerebral angiography and fusion 3DCG in our case revealed that the shunt point of the DAVF was in contact with the outer membrane of CSDH without cotton wool-like staining along the CSDH membrane. Therefore, DAVF may provide abundant feeding to the CSDH membrane. These unique imaging findings suggest that DAVF may be associated with the formation of CSDH. Theoretically, embolization of this abnormal vessel network in the CSDH membrane, including the DAVF, could prevent the enlargement or recurrence of CSDH. Moreover, the CSDH disappeared completely after MMA embolization despite induction of anticoagulant therapy, which was a risk factor for the recurrence of CSDH.23,24) These findings and the clinical course indicated that MMA embolization for DAVF was also potentially effective for CSDH in this case.
In our case, the detailed architecture of DAVF that was in contact with the outer membrane of CSDH could be clearly visualized using fusion 3DCG, which indicated that DAVF may contribute to the recurrence of CSDH. Vascular malformations should be considered in patients with refractory CSDH. Nevertheless, our study was limited by the lack of case series data. Further research is needed to elucidate the association between DAVF and CSDH.
In conclusion, we encountered a case of coexisting CSDH and DAVF, which presented unique imaging findings and clinical course. This case implies that increased meningeal blood flow due to DAVF can contribute to CSDH development and that DAVF embolization may be effective in preventing CSDH recurrence.
3DCG image, three-dimensional computer graphics image; CSDH, chronic subdural hematoma; CT, computed tomography; DAVF, dural arteriovenous fistula; DVT, deep vein thrombosis; MMA, middle meningeal artery
SK certifies that all authors have participated and have been involved in the case presented and/or in the elaboration of the present manuscript. All authors contributed to the article and approved the submitted version.
The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.