Abstract
Primary germ cell tumors of the central nervous system (CNS) typically occur in the neurohypophysis, hypothalamus, or pineal gland and rarely in the spinal cord. We report a case of a spinal intramedullary tumor, which was first detected on magnetic resonance imaging (MRI) 41 months after the initial symptoms, with a verified pathological diagnosis of germinoma. The initial symptom was an abnormal sensation in the left plantar region that gradually worsened, resulting in severe sensory disturbance, difficulty in standing, and even bladder rectal disturbance. Repeated MRI after the onset failed to provide an imaging diagnosis. The MRI was performed 41 months after the onset and revealed a previously undiagnosed, contrast-enhancing spinal intramedullary neoplastic lesion at the Th11-12 level. Gross total resection of the tumor was successfully performed, and the pathology confirmed the diagnosis of pure germinoma. Postoperative chemotherapy, followed by local radiation, was successfully administered. Among primary germinomas of the CNS, occult germinoma that lacks imaging findings suggestive of tumors in the early stages of onset and becomes apparent over time is often reported as a primary neurohypophyseal germinoma, particularly in adolescents presenting with diabetes insipidus. In the present case, the lesion appeared to correspond to a primary occult germinoma of the intramedullary spinal cord.
Introduction
Primary germ cell tumors of the spinal cord are extremely rare, and there is no established consensus on their clinical course, diagnosis, and treatment.1) In this report, we describe an extremely rare case in which an intramedullary tumor was first detected by magnetic resonance imaging (MRI) 41 months after onset. Repeated MRI after onset failed to provide diagnosis. As the symptoms worsened, the psychiatrist performed another imaging test and found an abnormality suggestive of a spinal intramedullary tumor. The patient was sent to our institute for surgical verification. Permanent pathological findings confirmed the diagnosis of pure germinoma. Postoperative chemotherapy, followed by local radiation, was administered, and subsequent improvement in the patient's neurological condition was noted. In this case report, the rare pathology of potentially advanced germinoma of the spinal cord is discussed.
Case Report
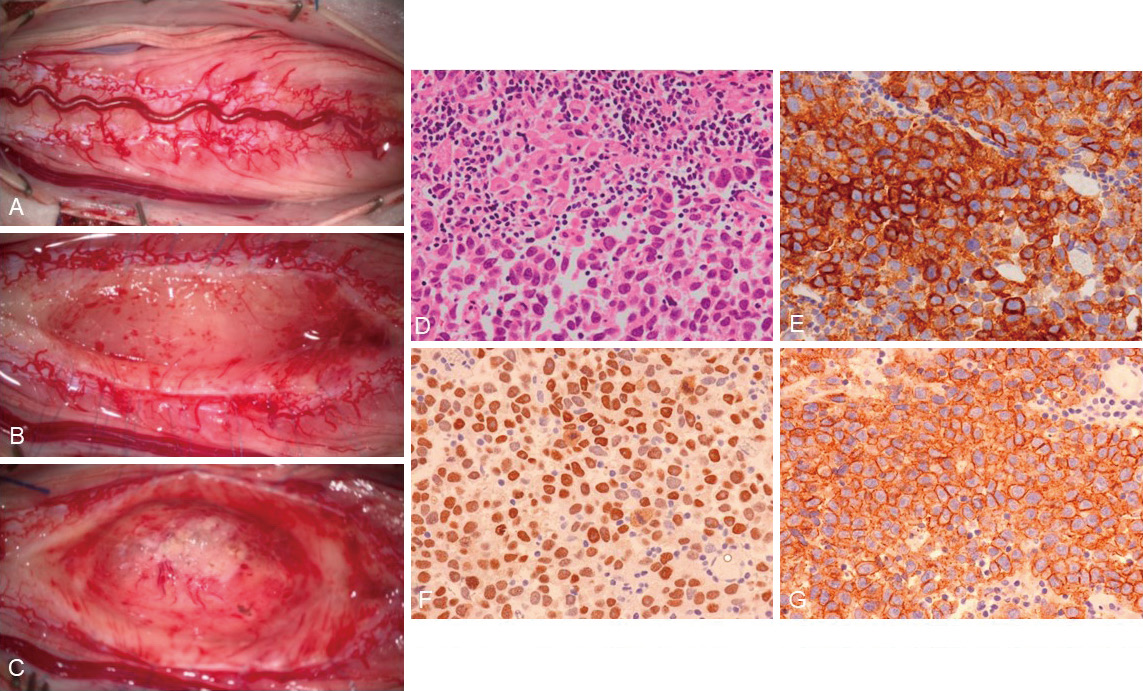
Forty-one months ago, a 45-year-old woman with no underlying medical condition experienced an abnormal sensation in the left plantar area and underwent a thorough examination, including imaging tests, at several medical institutions, including neurosurgical or neurology clinics; however, no definitive diagnosis was established. A lumbar MRI performed 24 months after the onset did not suggest any specific findings around the conus medullaris (Fig. 1A). Additionally, the patient was suspected of having a mental illness and had been receiving psychotherapy. The effect of psychotherapy was poor, and the patient's symptoms further worsened. She developed severe sensory disturbance below the trunk, difficulty in standing, and bladder and rectal dysfunction. The psychiatrist performed another imaging test and found an abnormality suggestive of a spinal intramedullary tumor. The patient was sent to our institute for surgical verification.

Neurological findings on arrival at our neurosurgical clinic revealed a significant motor weakness of the bilateral lower extremities with a manual muscle test indicating 2/5 weakness, predominantly in the ankle joints. Decreased tactile pressure sensation, hyperalgesia, loss of warm sensation and pain, decreased vibration sensation in the abdomen and bilateral lower extremities, and decreased pressure of urination and fecal incontinence were also observed. Lumbar MRI showed spinal cord enlargement and intramedullary mass lesions at the level of the 11th-12th thoracic spine (Fig. 1B, C).
Surgery and pathological diagnosis
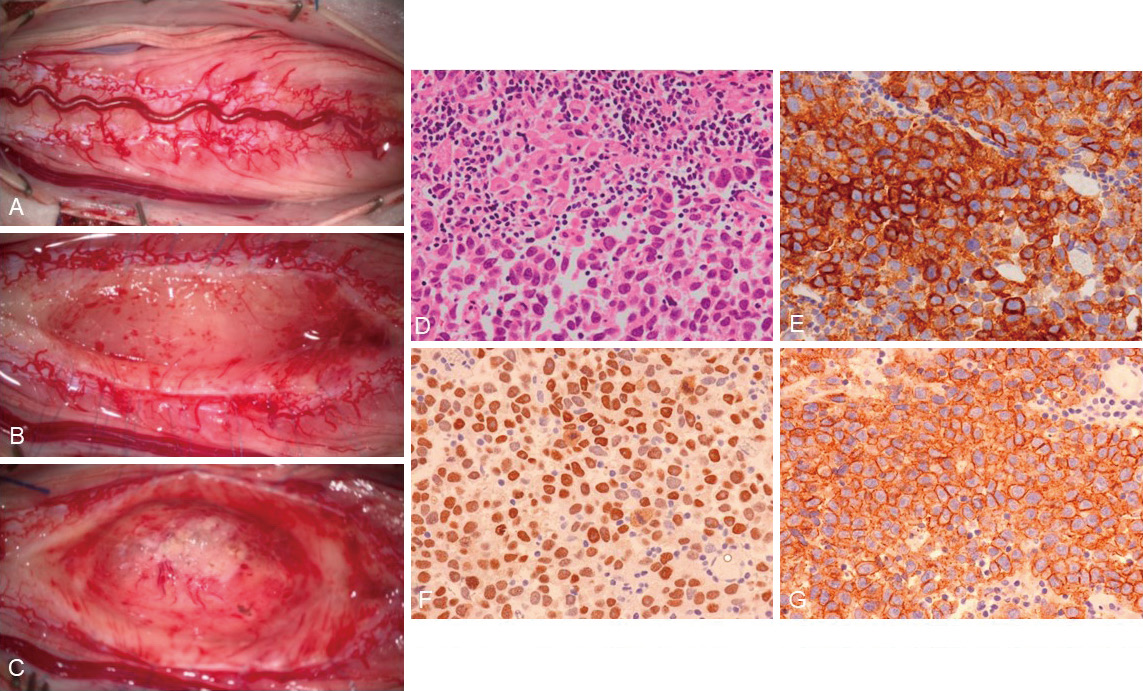
Surgery was performed under general anesthesia in the prone position with intraoperative neuromonitoring. Osteoplastic laminotomy of the 11th-12th thoracic spine was performed to expose the posterior surface of the spinal cord. The spinal cord appeared swollen (Fig. 2A). The posterior median sulcus was identified and separated to reveal an intramedullary tumor (Fig. 2B). The tumor was soft and hemorrhagic, and it showed negative protoporphyrin IX fluorescence. A portion of the tumor was sent to the department of clinical pathology for rapid intraoperative pathological diagnosis, which revealed it to be a high-grade tumor; however, a clear diagnosis was unobtainable. The boundary between the tumor and the normal spinal cord was carefully identified, and the tumor was dissected circumferentially with the help of internal decompression of the tumor. Finally, gross total resection of the tumor was performed (Fig. 2C). Indocyanine green video angiography confirmed maintenance of blood flow in the tumor removal cavity. Postoperative permanent pathology revealed a two-cell pattern consisting of tumor cell proliferation and lymphocytic infiltration. Immunostaining was positive for placental alkaline phosphatase, c-kit, and octamer-binding transcription factor 3/4, suggesting pure germinoma of the spinal cord (Fig. 2D-G).
Brain and pelvic MRIs revealed no obvious neoplastic lesions. The patient was diagnosed with primary pure germinoma of the intramedullary spinal cord. Lumbar MRI on postoperative day 7 showed no obvious residual tumor, suggesting gross total resection of the tumor (Fig. 3A, B). Postoperative blood tests showed no significant elevation in alpha-fetoprotein or human chorionic gonadotropin levels. After careful deliberation by the cancer board, chemotherapy using cisplatin and etoposide combined with local radiation was administered postoperatively. Lumbar MRI after chemotherapy and radiation showed no apparent recurrence (Fig. 3C, D). Postoperative rehabilitation enabled the patient to walk using a walker and regain bladder control.
Discussion
Germ cell tumors arising from the central nervous system (CNS) are rare, accounting for approximately 1.9% of all CNS tumors in Japan.2) In this classification, intracranial primary tumors, such as those arising from the neurohypophysis, hypothalamus, or pineal gland, comprise the majority, whereas spinal cord tumors comprise the minority. Primary spinal germ cell tumors have been reported previously. The age of onset for spinal germ cell tumors ranges from adolescence to young adulthood, consistent with that for intracranial germ cell tumors.1) Primordial germ cells appear in the yolk sac of the embryo during the third to fourth week of gestation. The normal destination is the ovaries or testes, but some germ cells migrate elsewhere in the developing embryo for unknown reasons. These cells become trapped mainly in midline sites, such as the mediastinum, retroperitoneum, and third ventricle.3) Many pineal germ cell tumors are thought to result from the midline location of the pineal gland near the third ventricle.4) Although it is difficult to find a definitive reason for the development of spinal cord tumors in adults, such as in the present case, it is possible that the same mechanism may be involved in the development of germ cell tumors of the spinal cord located in the midline.
Among primary intracranial germinomas, those that lack imaging findings suggestive of tumors in the early stage of onset and become apparent over time are called "occult germinomas." 5) A typical example is a case of the onset of diabetes insipidus in school children or adolescents, with no obvious lesions on brain imaging in the early stages of the disease; however, months or years later, a brain MRI revealed an enlarged pituitary stalk and mass lesions in the hypothalamus, pituitary stalk, or posterior pituitary gland, leading to the possible diagnosis of a germinoma.5) There are still some cases that lack characteristic imaging findings in the early stage of disease, and neurohypophyseal germinoma is diagnosed later than other brain tumors.6) Clinical features reported as occult germinomas are now being recognized as imaging findings characteristic of and as exhibiting the clinical course of neurohypophyseal germinoma,7,8) which is now widely recognized as a differential diagnosis for diabetes insipidus in adolescents and young adults, particularly if the cause is unknown. Primary CNS germinomas that exhibit the characteristic course of occult germinoma have been reported along with neurohypophysis, for example, occult cerebellar germinoma with ataxia and cranial nerve palsy.9,10) In the current case, the patient's symptoms began with sensory disturbance in the lower limbs, which was exacerbated by paralysis and bladder and rectal disturbances. Despite repeated examinations at several medical institutions, no clear diagnosis was made. A lumbar MRI performed 24 months after onset showed no obvious neoplastic lesions, and the patient's symptoms had already advanced. The delay between the onset of symptoms and a clear radiological appearance was consistent with the characteristics of occult germinomas. Among the previous reports of primary spinal cord germinoma, we summarized cases that required >1 year from the onset of symptoms for an accurate diagnosis (Table 1).11-19) The tumor is commonly located at the thoracic level, and patients usually develop lower-extremity symptoms. Two case reports (Cases 3 and 8) showed no abnormal findings on the initial MRI after onset, but there were abnormal findings on the follow-up MRI.13,18) However, there were no reports of abnormal findings on MRI 24 months after onset, as in the present case. It is difficult to explain why the appearance of abnormal findings on images was significantly delayed in this case compared to other cases; however, in CNS germ cell tumors, diagnostic radiation, use of corticosteroids, and some kind of immunologic response are considered to influence tumor regression, and the imaging examination and treatment before definitive diagnosis may have influenced the delay in the appearance of abnormal findings on images.20) The imaging findings are also variable, with no consistent findings, suggesting that follow-up examinations, including repeat imaging studies, are desirable for diagnostic confirmation of primary spinal cord germinoma.
Table 1
Summary of previously reported cases of primary occult germinoma of the spinal cord
| No. |
Authors |
Age/Sex |
Initial symptoms |
Duration from onset to diagnosis |
Spinal level |
Location |
Surgery |
Chemotherapy |
Radiation |
| M: male; F: female; T: thoracic; IM: intramedullary, EM: extramedullary; GTR: gross total resection; STR: subtotal resection; LS: local spine; OSA: other spinal area; WS: whole spine; WB: whole brain; ND: not determined |
| 1 |
Hanafusa et al., 1993 (11) |
34/F |
Numbness of the lower extremities |
42 months |
T10-T11 |
IM |
GTR |
― |
LS + OSA |
| 2 |
Kiyuna et al., 1999 (12) |
20/F |
Back pain |
24 months |
T11-L3 |
EM |
GTR |
― |
LS + OSA |
| 3 |
Chute et al., 2003 (13) |
18/M |
Ankle weakness |
24 months |
T6-T8 |
IM |
Biopsy |
― |
LS |
| 4 |
Watanabe et al., 2005 (14) |
33/F |
Numbness of the lower extremities |
45 months |
T1-T3 |
IM |
Partial |
Carboplatin + Etoposide |
LS |
| 5 |
Nakata et al., 2006 (15) |
35/M |
Weakness of lower extremity |
54 months |
T6-T7 |
IM |
GTR |
Carboplatin + Etoposide |
WS |
| 6 |
Yamagata et al., 2009 (16) |
33/M |
Gait disturbance |
24 months |
T9-T11 |
IM |
Partial |
Carboplatin + Etoposide |
WB + WS |
| 7 |
Kinoshita et al., 2010 (17) |
21/F |
Back pain, constipation, and urinary urgency |
12 months |
T9-T11, L2-L3 |
IM + EM |
STR |
Carboplatin + Etoposide |
WS |
| 8 |
Madhukar et al., 2013 (18) |
11/F |
Weakness of the lower extremity |
20 months |
T6-T7 |
IM |
Biopsy |
1st: Carboplatin + Etoposide; 2nd: Cyclophosphamide; 3rd: Thiotepa + Etoposide |
LS, followed by WB + LB |
| 9 |
Hu et al., 2017 (19) |
24/M |
Back pain |
12 months |
L2-L3 |
EM |
GTR |
ND |
ND |
| 10 |
Present case |
45/F |
Abnormal sensation of left lower extremity |
41 months |
T11-T12 |
IM |
GTR |
Cisplatin + Etoposide |
LS |
Primary germ cell tumors of the spinal cord are rare, and there is no established treatment strategy that includes postoperative chemotherapy and radiation. In previous studies, radiation was the postoperative treatment of choice in most cases. There have been many cases in which patients were treated with radiation alone without recurrence. When chemotherapy is selected, a combination of a platinum anticancer drug and etoposide is often chosen.2) There is a method for determining postoperative chemotherapy and radiation according to prognostic classification based on the histology of the tumor, consistent with the treatment strategy for primary germ cell tumors of the CNS in Japan.16,21) When a case is classified into the good prognosis group with pure germinoma, chemotherapy using cisplatin and etoposide and local radiation are recommended as postoperative adjuvant therapy.
Conclusion
Among germinomas that originate from the CNS, there is a rare category of occult germinoma with few suspicious tumor findings in the early stage of onset, with the lesions becoming clearer over time. In particular, it is often reported as a germinoma of neurohypophysis in adolescents, which develops with diabetes insipidus. In the present case, the lesion appeared to correspond to an occult germinoma of the spinal cord. Surgical verification should be performed to confirm the diagnosis. Postoperative adjuvant therapy has not been standardized but it should be planned according to the germinoma in the neurohypophysis, hypothalamus, or pineal gland.
Acknowledgments
The authors thank Dr. Masahiro Goto (Cancer Chemotherapy Center) and Dr. Keiji Nihei (Department of Radiation Oncology) for their dedicated therapeutic support.
Conflicts of Interest Disclosure
The authors declare no conflicts of interest.
References
- 1) Nikitović M, Grujičić D, Skender Gazibara M, Stanić D, Bokun J, Sarić M: Intramedullary spinal cord germinoma: a case report and review of literature. World Neurosurg 95: 392-398, 2016
- 2)
Brain tumor registry of Japan (2005-2008). Neurol Med Chir (Tokyo) 57: 9-102, 2017
- 3) Fetcko K, Dey M: Primary central nervous system germ cell tumors: a review and update. Med Res Arch 6: 1719, 2018
- 4) Villano JL, Propp JM, Porter KR, et al.: Malignant pineal germ-cell tumors: an analysis of cases from three tumor registries. Neuro Oncol 10: 121-130, 2008
- 5) Kato T, Sawamura Y, Tada M, et al.: Occult neurohypophyseal germinomas in patients presenting with central diabetes insipidus. Neurosurg Focus 5: e6, 1998
- 6) Sethi RV, Marino R, Niemierko A, Tarbell NJ, Yock TI, MacDonald SM: Delayed diagnosis in children with intracranial germ cell tumors. J Pediatr 163: 1448-1453, 2013
- 7) Di Iorgi N, Napoli F, Allegri AE, et al.: Diabetes insipidus - diagnosis and management. Horm Res Paediatr 77: 69-84, 2012
- 8) Cerbone M, Visser J, Bulwer C, et al.: Management of children and young people with idiopathic pituitary stalk thickening, central diabetes insipidus, or both: a national clinical practice consensus guideline. Lancet Child Adolesc Health 5: 662-676, 2021
- 9) Minami N, Tanaka K, Kimura H, et al.: Radiographic occult cerebellar germinoma presenting with progressive ataxia and cranial nerve palsy. BMC Neurol 16: 4, 2016
- 10) Evanson EJ, Lewis PD, Colquhoun IR: Primary germinoma of the posterior cranial fossa: a case report. Neuroradiology 39: 716-718, 1997
- 11) Hanafusa K, Shibuya H, Abe M, Yamaura K, Suzuki S: Intramedullary spinal cord germinoma. Case report and review of the literature. Rofo 159: 203-204, 1993
- 12) Kiyuna M, Toda T, Sadi AM, Toyoda Z, Nakashima Y: A rare case of extramedullary spinal cord germinoma. Pathol Int 49: 633-637, 1999
- 13) Chute DJ, Burton EC, Klement IA, Frazee JG, Vinters HV: Primary intramedullary spinal cord germinoma: case report. J Neurooncol 63: 69-73, 2003
- 14) Watanabe A, Horikoshi T, Naganuma H, Satoh E, Nukui H: Intramedullary spinal cord germinoma expresses the protooncogene c-kit. Acta Neurochir (Wien) 147: 303-308; discussion 308, 2005
- 15) Nakata Y, Yagishita A, Arai N: Two patients with intraspinal germinoma associated with Klinefelter syndrome: case report and review of the literature. AJNR Am J Neuroradiol 27: 1204-1210, 2006
- 16) Yamagata T, Takami T, Tsuyuguchi N, Goto T, Wakasa K, Ohata K: Primary intramedullary spinal cord germinoma: diagnostic challenge and treatment strategy. Neurol Med Chir (Tokyo) 49: 128-133, 2009
- 17) Kinoshita Y, Akatsuka K, Ohtake M, Kamitani H, Watanabe T: Primary intramedullary spinal cord germinoma. Neurol Med Chir (Tokyo) 50: 592-594, 2010
- 18) Madhukar M, Maller VG, Choudhary AK, Iantosca MR, Specht CS, Dias MS: Primary intramedullary spinal cord germinoma. J Neurosurg Pediatr 11: 605-609, 2013
- 19) Hu Q, Yu W, Du Q, Zhu Q, Che Z: Primary extramedullary spinal germinoma: case report and review of the literature. Neurosurg Rev 40: 171-176, 2017
- 20) Schipmann S, Keurhorst D, Köchling M, et al.: Regression of pineal lesions: spontaneous or iatrogenic? A case report and systematic literature review. World Neurosurg 108: 939-947, 2017
- 21) Matsutani M, Ushio Y, Abe H, et al.: Combined chemotherapy and radiation therapy for central nervous system germ cell tumors: preliminary results of a phase II study of the Japanese Pediatric Brain Tumor Study Group. Neurosurg Focus 5: e7, 1998