2023 Volume 10 Pages 81-85
2023 Volume 10 Pages 81-85
Middle meningeal arteriovenous fistula (MMAVF) is a shunt between the middle meningeal artery and the vein surrounding the artery. We report an extremely rare case of spontaneous MMAVF; then, we evaluated the effectiveness of trans-arterial embolization for spontaneous MMAVF and the possible cause of spontaneous MMAVF.
A 42-year-old man with tinnitus, a left temporal headache, and pain surrounding the left mandibular joint was diagnosed with MMAVF on digital subtraction angiography. Trans-arterial embolization with detachable coils was conducted, which resulted in a fistula closure and symptoms' diminishment. The cause of MMAVF was thought to be the rupture of the middle meningeal artery aneurysm.
A middle meningeal artery aneurysm can be a cause of spontaneous MMAVF, and trans-arterial embolization might be an optimal treatment.
Middle meningeal arteriovenous fistula (MMAVF) is a shunt between the middle meningeal artery and the venous around the artery.1) The major cause of this disease is a head injury or an iatrogenic injury.1-4) Meanwhile, "spontaneous" MMAVF, defined as MMAVF without such events, is extremely rare. This thesis reports a case of spontaneous MMAVF. This disease was successfully treated with trans-arterial embolization (TAE). Here, a probable cause and prognosis of spontaneous MMAVF was also discussed.
A 42-year-old man came to our hospital for evaluation and treatment of pulsatile tinnitus and left temporal headache for two months. First, he had noticed temporal headache with intermittent pain around his left mandibular joint. A few weeks later, a bull sound was heard on the left side. He then visited a neurologist, and an evaluation with magnetic resonance imaging (MRI) was conducted. An arteriovenous (AV) shunt was suspected on MRI, and he was referred to our hospital for further investigation and treatment. His past medical history included only hypertension, which was treated with telmisartan. He denied any recent history of head trauma or a history of brain surgery. Physical exams show that he was alert and no neurological deficits were observed except the left side tinnitus. No physical signs or test results indicating coagulopathy or connective tissue diseases were observed. MRI shows a relatively dilated middle meningeal artery (MMA) with surrounding dilated veins was admitted, and we suspected an existence of AV shunt (Fig. 1). On digital subtraction angiography (DSA), a single direct AV fistula was seen at a proximal point of the convexity branch of MMA, which directly drained into the middle meningeal vein (MMV). No other feeders were seen on bilateral internal carotid arteriography (ICAG), bilateral external carotid arteriography (ECAG), or bilateral vertebral arteriography (VAG), which was consistent with the diagnosis of MMAVF. The main drainage route started from the MMV, went through an emissary vein of the temporal bone, and ran into the venous plexus around the mandibular joint (Fig. 2). No cortical venous reflux was noted. High-resolution cone-beam CT revealed a single shunt point with an aneurysm-like arterial dilatation at the shunt (Fig. 3). Considering it as a symptomatic MMAVF case, the fistula was embolized.
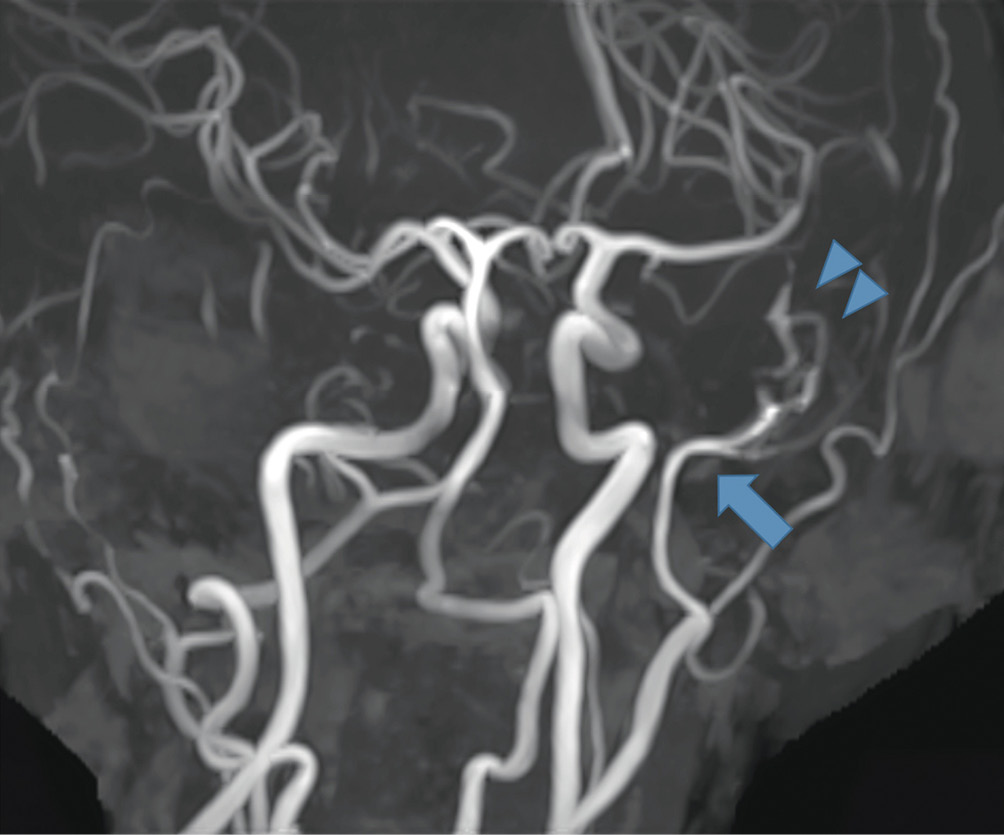
MRA on the admission day.
Left MMA was dilated (arrow) and meningeal veins (arrowhead) around it were seen on MRA.
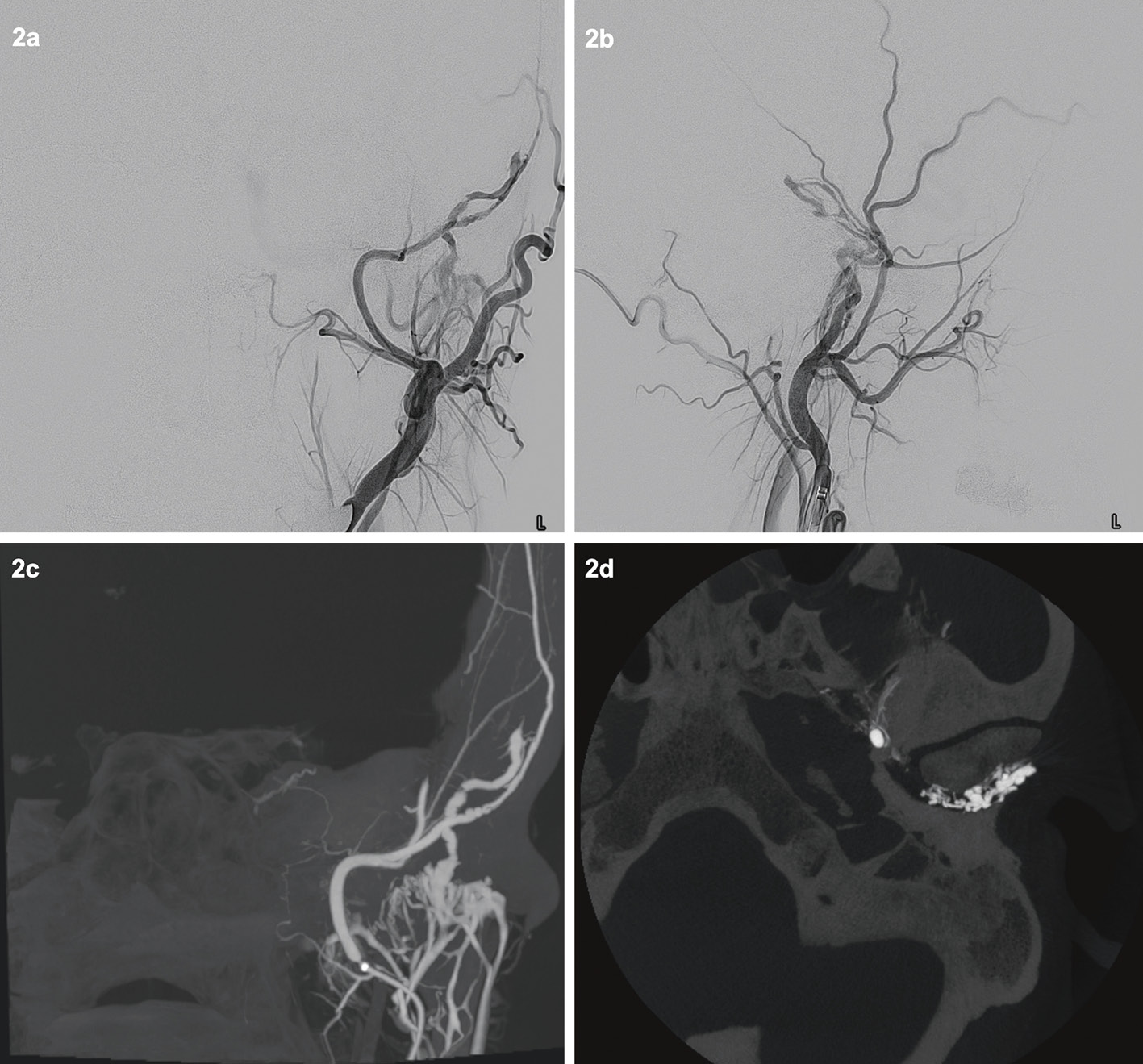
DSA.
2 (a, b); Left ECAG revealed MMAVF.
2 (c, d); The drainer of the shunt ran into the venous plexus around the mandibular joint, which we thought caused mandibular joint pain.
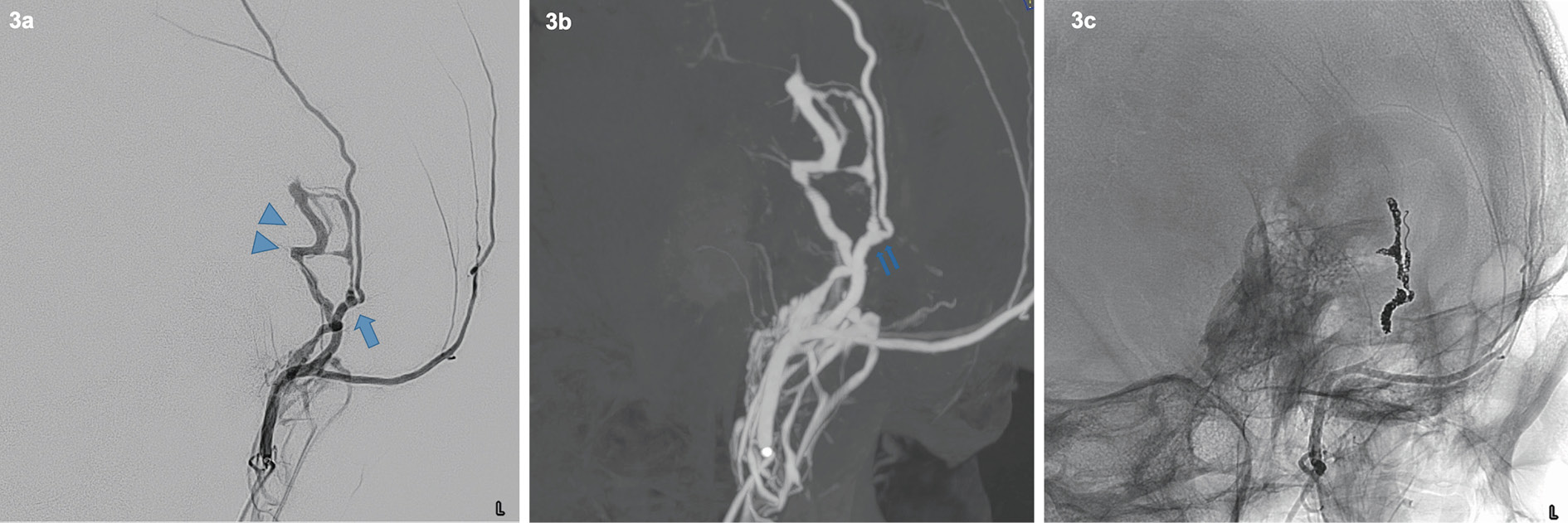
Working angle.
3 (a); MMA had an AV shunt at a proximal point of the convexity branch (arrow). Meningeal veins (arrowhead) made a hairpin curve, and they were directed into an emissary vein and venous plexus around the mandibular joint.
3 (b); At the shunt point, there was an aneurysmal dilatation of MMA (double arrow).
3 (c); i-ED coils were placed on the shunt point, a part of MMA, and meningeal veins.
A 5F FUBUKI guiding sheath (ASAHI Intecc, Aichi, Japan) was placed in the right femoral artery and was navigated to the left external carotid artery. Excelsior SL-10 micro-catheter (Stryker Neurovascular, Fremont, California) over 0.014 Synchro (Stryker Neurovascular, Fremont, California) was navigated to the shunt point using 3.2F TACTICS (Technocrat Corporation, Aichi, Japan) as a distal access catheter. It was easy to access to both dilated veins and distal MMA, and we embolized the shunt point along with aneurysm-like dilatation, a part of MMA, and drainer route with the i-ED coil (Kaneka Medical Products, Kanagawa, Japan). The blood flow through the shunt point vanished, and we finished the treatment (Fig. 4). MRI on post-operative day 1 revealed no signs of remained MMAVF, and his symptoms of tinnitus and headache disappeared after the operation. Follow-up MRI after six months showed no recurrence of MMAVF.
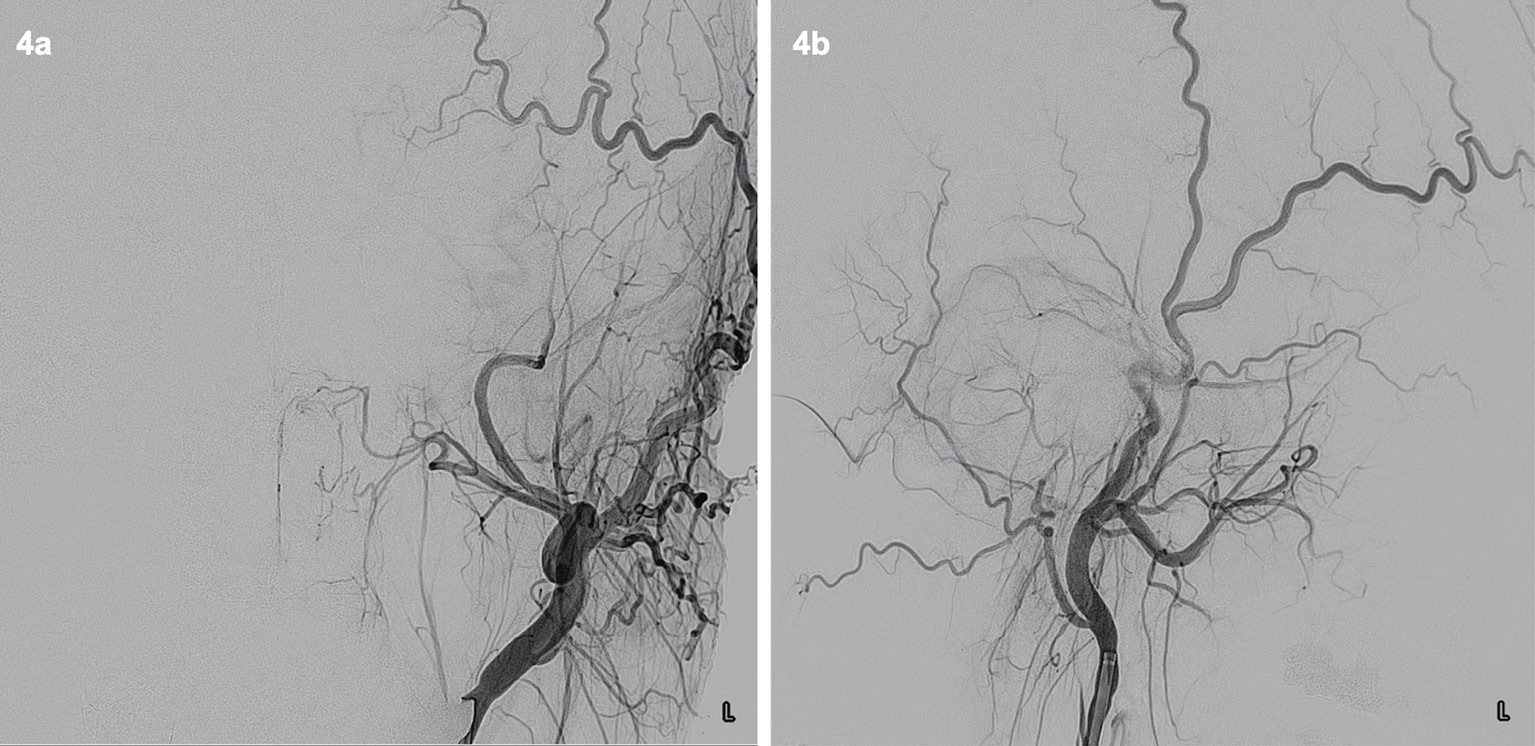
DSA after coiling.
4 (a, b); Left ECAG showed vanishment of the MMAVF.
The occurrence rate of MMAVF was 1.8% in severe head injuries,3) and most cases were accompanied with a cranial fracture.3,5) The typical symptoms of MMAVF are tinnitus and headache, but this can cause more severe conditions, such as subarachnoid haemorrhage, subdural/epidural hematoma, and venous infarction because of venous reflux.1,6,7) In this case, his symptoms started with a left temporal headache and pain in the left mandibular joints. We suspected that the pain of the mandibular joints was caused by the highly dilated plexus-like-veins in the joint due to high shunt flow (Fig. 2). Pulsatile tinnitus often happens when the shunt involves meningeal veins or sinuses around a petrous bone,8) which was also observed in this case. All symptoms disappeared after the operation, supporting their relationship with MMAVF.
Spontaneous MMAVF and its treatmentThis case is rare and peculiar in the meaning of "spontaneous" MMAVF. Although there are many reports of traumatic or iatrogenic MMAVF cases, only nine spontaneous cases reported in English translation have been found (Term; "middle meningeal arteriovenous fistula" or "middle meningeal artery fistula" ).1,2,9-11) We summarize those characteristics in Supplementary Table 1, 2.
As for treatment, TAE or open surgery was mostly selected as a first line treatment for traumatic/idiopathic MMAVF,2,6) which often resulted in the good closure of shunts. Contrary, some cases reported the spontaneous closure of MMAVF.2,5)
In spontaneous MMAVF, same as traumatic/idiopathic MMAVF, TAE was done in most cases (9 in 10 cases), and all of which achieved good obliteration of the fistulas. MMAVF without intracranial haemorrhage resulted in good outcome, but intracranial haemorrhage can easily happen and deteriorate patient's neurological outcome in spontaneous MMAVF (7 in 10 cases). We should note that there might be a selection bias wherein symptomatic cases are easily found and reported; but still, we should notice the importance to diagnose spontaneous MMAVF before causing severe complications.
Pathogenesis of the MMAVF is aneurysm ruptureAs the most likely cause of MAVF in the present case, we suspect a rupture of the MMA aneurysm into the meningeal vein. Firstly, his symptoms started without any triggers, which led us to suspect an underlying abnormal lesion. Secondly, the dural arteriovenous fistula usually has plenty of small meningeal feeders, but this case has only a single hole fistula without meningeal feeders, also suggesting some underlying causes. However, he denied any traumatic/idiopathic history, and there were no signs or test results indicating coagulopathy or connective tissue diseases.
Finally, even though the proximal MMA were dilated due to the shunt flow, the shunt point had an aneurysm-like dilation of the artery, which is demarked from other parts of MMA by its narrow neck on DSA (Fig. 3). All three points suggested the MMA aneurysm as the cause of this disease.
True MMA aneurysm is rare but some have been reported.12) Hassler et al.13) reported that the commonly seen structure of MMA distal to the foramen spinosum is same as the other intracranial arteries and medial defects, which is the key for the formation of intracranial saccular aneurysms. Even hypertension, shown in our case, can be a cause true MMA aneurysm.14)
True MMA aneurysm often ruptures. Kobata et al.14) summarized true MMA aneurysm cases, and 7 out of 16 cases presented intracranial haemorrhage, including subdural/intracerebral/subarachnoid haemorrhage. Anatomically, MMA and paired veins runs alongside and are tightly adherent to the outer surface of the dura matter. Hence, when the aneurysm heads into the surrounding veins, it's rupture could cause MMAVF that is similar to aneurysmal rupture, a well-known cause of direct carotid-cavernous fistula.
We experienced a rare spontaneous MMAVF case treated with trans-arterial embolization. The rupture of an aneurysm can be a cause of MMAVF. Trans-arterial embolization for spontaneous MMAVF often leads to good obliteration, but intracranial haemorrhage can cause a poor neurological outcome.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
AV, arteriovenous; DSA, digital subtraction angiography; ECAG, external carotid arteriography; ICAG, internal carotid arteriography; MMA, middle meningeal artery; MMAVF, middle meningeal arteriovenous fistula; MMV, middle meningeal vein; MR, magnetic resonance; TAE, trans-arterial embolization; VAG, vertebral arteriography.
The authors certify that appropriate patient consent for the publication of patient information and images was received.
The authors report there are no conflicts of interests to declare. All authors have registered online self-reported COI Disclosure Statement Forms.