2023 Volume 10 Pages 279-283
2023 Volume 10 Pages 279-283
Endovascular treatment is a standard procedure for subclavian artery stenosis or obstruction. However, great care should be taken to avoid embolic complications to the vertebral artery, and several methods have previously been reported. Hence, as surgical procedures become increasingly complicated, unintended issues may arise during treatment. Here, the authors report a case where the filter-type protection device was caught in the stent because the patient moved during treatment, leading to open surgery to recover the filter-type protection device.
A 78-year-old female suffering from a left subclavian steal syndrome underwent stenting due to subclavian artery stenosis. The stenotic lesion was approached via the transfemoral route, and a filter-type protection device was advanced to the vertebral artery via the transbrachial route to prevent embolic complications. As the procedure was performed under local anesthesia, the patient moved during stent deployment proximally to the left vertebral artery origin, and the stent unintentionally advanced distally, covering the vertebral artery and obstructing the retrieval catheter for the filter-type protection device to advance. Failed attempts in recovering the filter-type protection device required open surgery for retrieval. Fortunately, there was no postoperative neurological and radiographic complication, ameliorating her chief complaint.
The retriever catheter for the protection device should be advanced beyond the vertebral artery orifice just proximal to the protection device before stenting to avoid such complications while also thoroughly considering the type of anesthesia during treatment.
The primary presenting symptoms of subclavian artery stenosis or obstruction are arm claudication, paresthesias, weakness, and sequelae of distal embolism.1) Furthermore, subclavian artery stenosis or obstruction can lead to subclavian steal syndrome caused by the reversal flow of the vertebral artery ipsilateral to the stenosis or occlusion. Subclavian steal syndrome includes vertigo, syncope, and even transient quadriparesis.2) While most endovascular interventions to the lesion are performed via a transfemoral approach, transradial access becomes an alternative approach. There is a 1%-5% risk of stroke during the treatment,3-5) and distal embolization through the ipsilateral vertebral artery to the posterior circulation is one of the major concerns. Distal artery protection during subclavian artery stenting has recently been advocated to counteract the concern. However, the authors show a case where the protection device caused a serious issue during endovascular surgery and propose the safest procedural protocol for subclavian artery stenting using a protection device.
A 78-year-old female suffered vertigo attacks and left arm claudication when moving her left arm. The left subclavian artery was near occluded on computed tomography angiography. Thus, her symptoms were likely a subclavian steal syndrome. The patient was scheduled for a subclavian artery stenting. Since the patient tolerated diagnostic angiography well, the stenting procedure was performed under local anesthesia via a combined transfemoral and transbrachial approach. A sheathless 6 fr guiding catheter (Fubuki, Asahi-intecc, Tokyo, Japan) was placed from the femoral artery to the origin of the left subclavian artery. Another sheathless 4 fr guiding catheter (Fubuki, Asahi-intecc, Tokyo, Japan) was advanced from the left brachial artery to the distal left vertebral artery, followed by introducing a filter-type protection device (Spider FX 6.0 mm, Medtronic, Minnesota, USA) into the left vertebral artery. This procedure prevented embolic complications to the left vertebral artery during stenting (Fig. 1). First, prestenting angioplasty was performed with a percutaneous transluminal angioplasty (PTA) balloon catheter (Shiden 5 × 20 mm, Kaneka, Tokyo, Japan). Then, the guiding catheter was advanced distally, crossing the stenosis, followed by an attempt to deploy a 6 × 20 mm SMART stent (Cordis, Miami, USA) proximally to the left vertebral artery origin. However, during deployment, the patient suddenly moved, and the stent unintentionally advanced distally, covering the vertebral artery and obstructing the retrieval catheter for the filter-type protection device to advance (Fig. 2). Although several procedures were tried, including an attempt to recover the protection device using a Goose Neck Sneer catheter (Medtronic, Minnesota, USA) via contralateral vertebral artery approach, the vertebrobasilar artery was strongly pulled downward, causing pain to the patient and forcing us to abandon the procedure, fearing secondary complication. After consulting cardiovascular surgery, the procedure was switched to general anesthesia, and a supraclavicular incision exposed the vertebral artery to retrieve the protection device directly. The left vertebral artery was occluded during surgery, as the endothelium was damaged when retrieving the protection device (Fig. 3). Fortunately, there was no postoperative neurological and radiographic complication with amelioration of her chief complaint.

The arrow indicates the stenosed segment of the subclavian artery (a). The diagram shows the presurgical plan of the procedure (b). The stent was planned to be placed far enough from the vertebral artery orifice so that the protection filter could be easily retrieved.
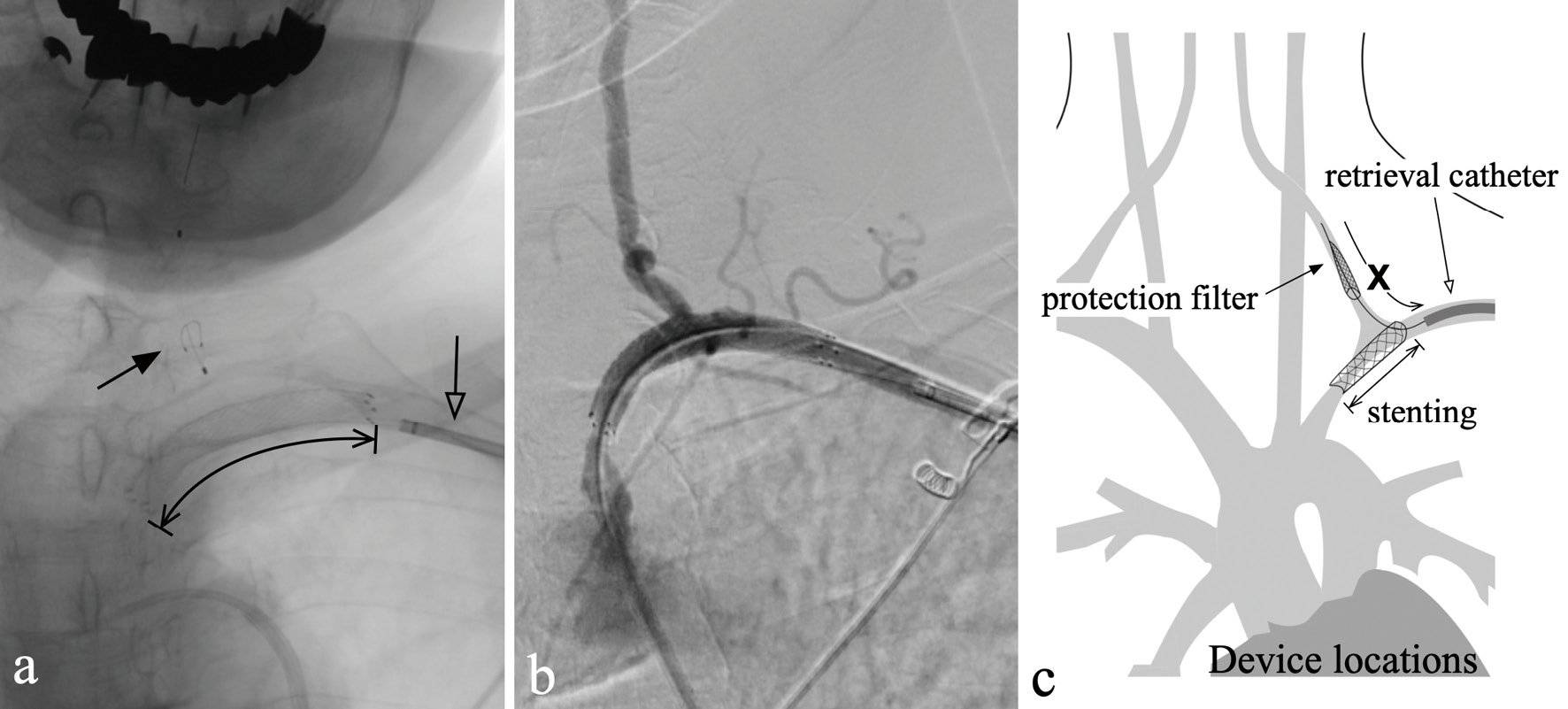
The black and white arrows indicate the locations of the protection filter and the retrieval catheter, respectively. The arrow indicator indicates the location of the stent (a). The stent was completely covering the vertebral artery orifice (b). The diagram shows how the stent interfered with retrieving the protection filter (c).

Photographs during open surgery for recovering the protection filter (a) and the recovered filter (b) are shown.
Endovascular therapy for subclavian artery stenosis is widely performed, and symptomatic stenosis or occlusion of the subclavian artery, acute ischemia threatening the extremities, asymptomatic stenosis or occlusion in patients with subclavian steal phenomenon are indications for PTA according to the European Society of Cardiology (ESC) 2017 Guidelines.6) However, the present case's treatment failed to fulfill its primary objective, ending with a serious complication, such as occluding one of the vertebral arteries.
Aside from technical issues that will be discussed, we must critically reflect on the chosen treatment setup. The primary trigger of the complication was the patient's unexpected motion during a critical moment of the procedure, which could have been avoided if the procedure was taken place under general anesthesia or at least under deep sedation. While we chose local anesthesia as a treatment setup based on the patient's tolerance during angiography, the authors retrospectively feel that the treatment should have been done with great care, foreseeing the patient becoming intolerant during the intervention. While general anesthesia could prevent any unintended patient-derived motions, it could put patients at new risks, such as stroke or myocardial ischemia due to hypotension for patients complicated by vascular diseases. For example, in the case of carotid artery stenting, whether one should choose local or general anesthesia is still under debate, with local anesthesia being favored.7) However, our tragic experience suggests that patients must be placed under general anesthesia, especially those with low tolerance to anxiety and pain.
From a technical point of view, distal vertebral artery embolism is the primary complication of endovascular treatment of subclavian artery stenosis. Previous literature shows a 1%-5% risk of stroke during subclavian artery stenosis stenting.3-5) Ipsilateral vertebral artery protection techniques have been reported to deal with this risk, such as using a filter-type protection device, a balloon microcatheter, a balloon-guiding catheter, and dual-balloon protection.3,4,8-11) The balloon protection technique places a balloon-guiding catheter at the proximal segment of the vertebral artery or at the orifice of it within the subclavian artery to prevent posterior circulation embolization caused by debris generated during subclavian artery stenting. However, aspirating the debris proximal to the protection balloon is difficult once the stent has been deployed. Meanwhile, the filter-type protection device technique preserves the anterograde vertebral artery flow throughout the procedure and allows a much easier aspiration of the debris.8,12) However, it should be noted that the placed stent could interfere with the protection filter, as demonstrated in the present case. From our experience, we recommend placing the retrieval catheter distal to the vertebral artery orifice before stenting, standing by to retrieve the protection filter (Fig. 4). The same could be applied to the balloon protection technique by guiding the aspiration catheter just proximal to the protection balloon before stent deployment.
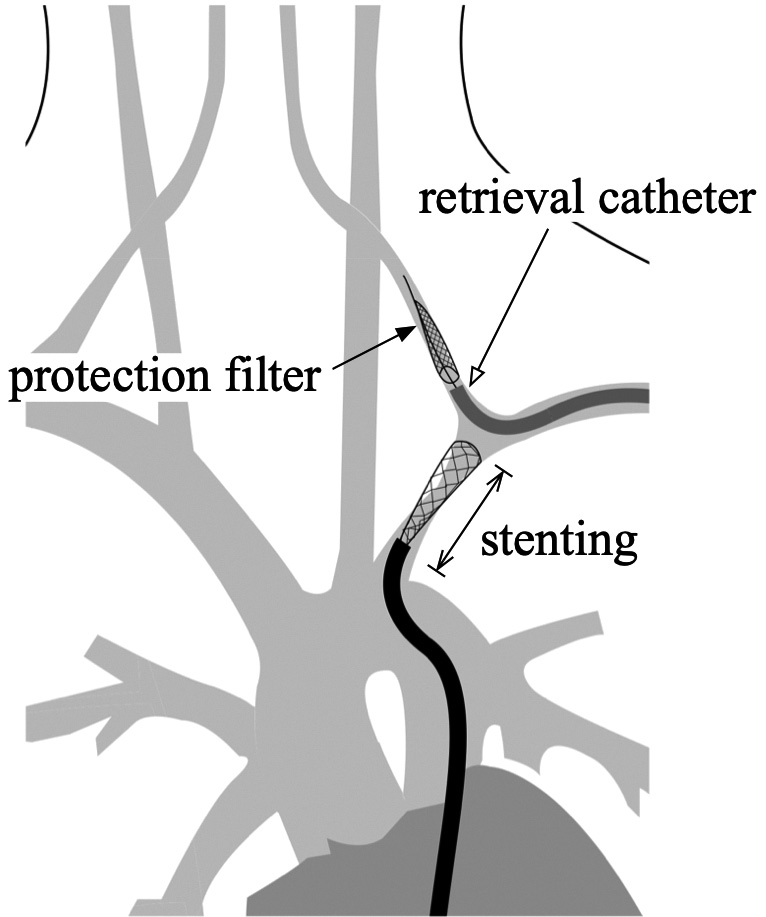
The proposed "safe" procedure for subclavian artery stenting is presented. The retrieval catheter for the proception filter should be advanced into the vertebral artery before stenting.
The authors reported a procedure-related serious complication regarding the filter-type protection device during subclavian artery stenting. We strongly advise having the retrieval catheter advanced just proximal to the protection device before stenting to avoid such complications. Our case also highlights the importance of choosing the appropriate anesthesia setup for individual patients.
The patient provided consent to submitting this case report to the journal.
There are no conflicts of interest.