2025 Volume 12 Pages 7-13
2025 Volume 12 Pages 7-13
We report a rare case of an elite para-athlete with lumbar disk herniation whose pain generator was difficult to diagnose and treat. A 28-year-old woman with paraplegia below the T10 level felt pain in her low back and left leg during a match. Magnetic resonance imaging revealed a lateral lumbar disk herniation and a high-intensity zone on the left side at the L5-L6 level. Because the pain disappeared following L5 selective nerve block, we performed transforaminal full-endoscopic discectomy alone. Despite the disappearance of leg pain after surgery, her low back pain persisted. We performed thermal annuloplasty because reproducible pain and subsequent temporary pain relief by discography and discoblock after the initial surgery indicated discogenic pain. Her suffering from back pain gradually reduced. She returned to competition 2 months after the second surgery without intensive rehabilitation due to difficulty in performing core exercises for abdominal muscles. During the return match, she experienced a relapse of pain in the low back and left leg, which was caused by a recurrence of disk herniation. We performed a full-endoscopic discectomy with thermal annuloplasty again. Her clinical symptoms were immediately relieved. We enhanced her thoracic spine flexibility to prevent subsequent recurrence. Finally, she returned to international competition 2 months after the third surgery. Close attention to para-athletes is required to achieve an accurate diagnosis of pain generators and prevent recurrence due to their distinctive disorders. Thermal annuloplasty and rehabilitating thoracic movement can be an excellent option for para-athletes with discogenic low back pain.
Low back pain (LBP) in athletes is a serious problem, and many studies have demonstrated a much higher prevalence of LBP in athletes in comparison to non-athletes.1,2) Among top-level athletes, 33%-84% of professional athletes3,4) and 47%-90% of Olympians5) experience one or more episodes of LBP during their lifetime. Lumbar disk herniation (LDH) is one of the most common causes of LBP6) and is more prevalent in athletes compared to the general population due to repetitive overloading on the spine. Generally, typical LDH is not difficult to diagnose. However, there are sometimes cases in which the cause of LBP is difficult to detect. Moreover, it might be more difficult to achieve an accurate diagnosis of the pain generator and an early return to sports in para-athletes, because of paralysis, hypoesthesia, and trunk instability. We herein report a case of an elite para-athlete with LDH whose pain generator was difficult to diagnose and treat.
The patient was a 28-year-old woman and elite para-athlete who experienced low back and left leg pain during a match. She was referred to our hospital because of resistance to ≥6 weeks of conservative treatment, including rest, medication, and selective L5 nerve root block with concordance and temporary disappearance of symptoms. She developed paraplegia and hypoesthesia below the T10 spinal level at 18 years of age. Her neurological function was Frankel grade B (complete loss of motor function and partially preserved sensory function) below the Th10 level. She had no other relevant past medical history. Plain radiography showed lumbarization (Fig. 1A and B). Magnetic resonance imaging (MRI) revealed a left lateral LDH and a high-intensity zone (HIZ) at the L5-L6 level (Fig. 1C-F). Preoperative computed tomography (CT) images after discography with provocation of similar LBP showed leakage of contrast agent via the posterolateral annulus fibrosus on the left side (Fig. 1G and H). On physical examination, she exhibited involuntary movements due to severe spasticity of the lower legs and could not maintain a supine position. Compression of the left L5 nerve root was considered to be the cause of the LBP. Based on this diagnosis, we performed a transforaminal full-endoscopic discectomy (FED) under general anesthesia with intraoperative free-running electromyography to prevent exiting nerve root injury. Since the selective L5 nerve root block eliminated both her low back and leg pain, we decided to proceed with discectomy alone. The lateral disk herniation and osteophytes at the L5-L6 level were resected via the outside of the disk, leading to the decompression of the left L5 nerve root. The operating time was 45 mins and the intraoperative blood loss was minimal. No complications related to surgery were observed.

Preoperative images of radiographs (A, B), MRI (C-F), and CT images after discography (G-H). (A) Posteroanterior radiograph showing lumbarization. (B) Lateral radiograph. (C) Mid-sagittal T2-weighted MRI showing disk degeneration at the L4-L5 and L5-L6 levels. (D) Para-sagittal T2-weighted MRI. (E, F) Axial images of T2-weighted MRI showing lateral lumbar disk herniation (white arrow) (E) and a high-intensity zone (yellow arrow) (F) on the left side of the L5-L6 level. (G) Sagittal CT. (H) Axial CT showing contrast leakage via a posterolateral annulus fibrosus tear on the left side of the L5-L6 level.
CT: computed tomography; MRI: magnetic resonance imaging
Left leg pain was reduced immediately after the surgery; however, she complained of prolonged intractable LBP. She was not able to sit for more than 20 mins although the brace used to stabilize her trunk improved the LBP a little. Although MRI exhibited sufficient resection of the herniated disk and no recurrence of LDH (Fig. 2), reproducible pain and subsequent temporary pain relief were confirmed by intervertebral discography and discoblock at the L5-L6 level, indicating discogenic pain. We considered that the persistent LBP was due to the ingrowth of nerve fibers into the intervertebral disk via an annular tear at the HIZ area. We performed thermal annuloplasty at the L5-L6 level in the HIZ area under general anesthesia using the outside-in technique. After the removal of red inflammatory granulation tissue (Fig. 3A), radiofrequency cauterization and coagulation of the damaged annulus with redness were performed using a bipolar system (Fig. 3B). The operating time was 55 mins and the intraoperative blood loss was minimal. Hematoxylin and eosin-stained sections of the resected tissue with redness demonstrated granulation tissue with rich angiogenesis (Fig. 3C). After the second surgery, the LBP gradually lessened. Since her palsy was below the T10 level, her abdominal muscles were weak, and it was very difficult to perform core muscle rehabilitation after surgery. She returned to training after 4 weeks, resumed playing after 6 weeks, and returned to international competition 2 months after the second surgery. However, the pain in her low back and left leg relapsed during the return match. MRI revealed a recurrence of left lateral LDH at the same level (Fig. 4). Reproducible pain and subsequent temporary pain relief were also confirmed by selective L5 nerve root block and discoblock at the L5-L6 level before the third surgery. Due to resistance to ≥6 weeks of conservative treatment, we performed a FED with thermal annuloplasty again. The operating time was 54 mins, and the intraoperative blood loss was minimal. Her clinical symptoms were relieved immediately after the surgery. This time, to prevent any further recurrence, we focused on rehabilitating thoracic movement. To reduce physiochemical stresses in the lumbar spine, we enhanced her flexibility in the thoracic spine using pilates, which consisted of 1-hr private sessions 5 days per week. She started conditioning after 2 weeks, returned to training after 4 weeks, and was able to take part in an important competition and achieve excellent results 2 months after the third surgery. At the 3-month follow-up examination after the third surgery, she had no symptoms.

MRI after the initial surgery showing disc degeneration at the L4-L5 and L5-L6 levels without Modic change and the recurrence of disc herniation. (A) Mid-sagittal T2-weighted MRI. (B) Mid-sagittal STIR MRI. (C) Para-sagittal T2-weighted MRI (D, E) Axial images of T2-weighted MRI.
MRI: magnetic resonance imaging; STIR: short-tau inversion recovery
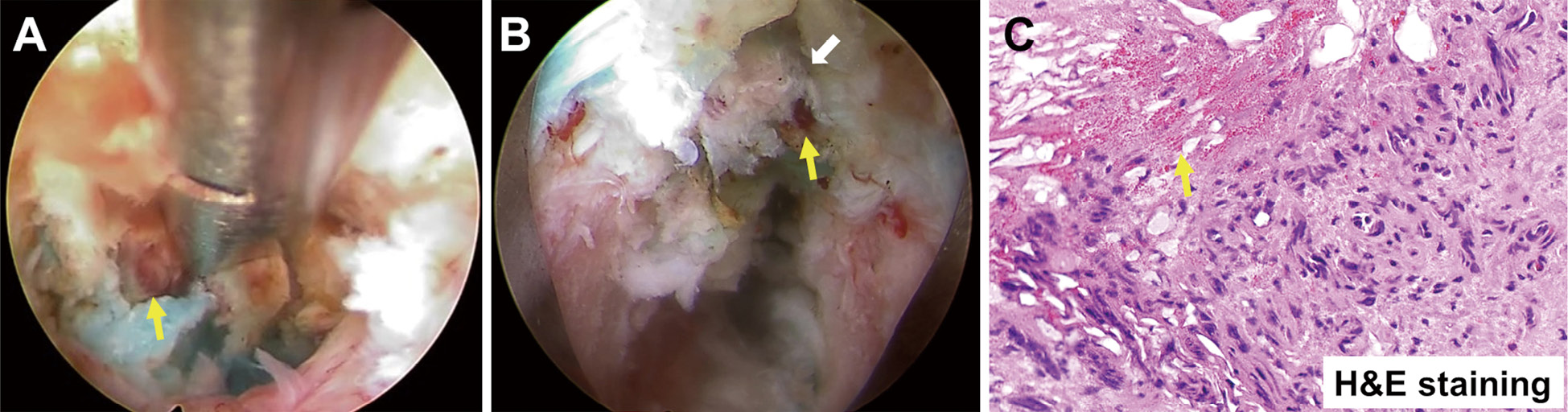
Intraoperative endoscopic views during the second surgery and micrographs of the inflammatory granulation tissue with redness. (A) An intraoperative endoscopic view during resection of the inflammatory granulation tissue with redness (yellow arrow). (B) An intraoperative endoscopic view showing a damaged annulus fibrosus with redness (yellow arrow) at the annular tear (white arrow). (C) Micrograph of a hematoxylin and eosin-stained section showing granulation tissue with rich angiogenesis (yellow arrow) (magnification: ×20).

MRI before the second surgery and the third surgery showing recurrent lateral disc herniation on the left side of the L5-L6 level. (A) Para-sagittal T2-weighted MRI before the second surgery. (B) Para-sagittal T2-weighted MRI before the third surgery showing a decrease in the T2-high area on the caudal side of the left L5 nerve root, indicating left L5 nerve root compression. (C) Axial T2-weighted MRI before the second surgery. (D) Axial image of T2-weighted MRI before the third surgery showing recurrent lateral disk herniation on the left side of the L5-L6 level.
MRI: magnetic resonance imaging
This case report raises alarms regarding the management of LDH in elite para-athletes. First, for an early return to sports, especially in an elite athlete, close attention is warranted to accurately identify and treat pain generators in patients with LDH and HIZ. Second, surgeons should take into account the distinctive disorders of individuals in the comprehensive management of para-athletes that may affect the postoperative course.
Diagnosis of discogenic LBP with HIZIn the present case, there was a pitfall in the diagnosis of LBP. In fact, it is not easy to achieve an accurate diagnosis of the pain generator in athletes with LBP.6) Disk-related LBP is the most common cause of LBP in adult elite athletes.6) Provocative discography has been the gold standard for the diagnosis and management of discogenic LBP,7) despite its invasiveness and associated complications, such as infection, neurological injury, and contrast medium reaction.8) Although disk pin puncture itself can potentially cause and accelerate lumbar disk degeneration, we performed the discography and subsequent discoblock to identify the pain generator. The HIZ, first reported by Aprill et al.9) in 1992, is a confined intensity signal zone on T2-weighted MR images that is located at the posterior or posterolateral annulus fibrosus. They demonstrated the significance of a HIZ as a sign of painful disk rupture. After that, many studies,7,10,11) including several meta-analyses demonstrated the association of HIZ with discogenic LBP, although some studies12) reported a limited role of HIZ in the diagnosis of LBP because of low sensitivity and high prevalence in asymptomatic patients. Regarding the pathomechanism, growing evidence suggests that an HIZ reflects inflammation-induced fluid accumulation at the tearing of annulus fibrosus with neovascular granulation tissue.13) This inflammatory granulation with angiogenesis implies the co-existence of ingrowth of nerve fibers into the intervertebral disk causing discogenic LBP, which is not observed in non-degenerated discs.14,15) In the present case, we confirmed the temporary disappearance of radicular pain as well as LBP after L5 nerve root block. This is why we initially diagnosed radicular LBP as the main pain generator. However, discography and discoblock at the L5-L6 level rather than L5 nerve root radiculography and block after the initial surgery showed superior performance in terms of concordance and pain reduction of persistent LBP, respectively. Additionally, histological findings suggested inflammatory granulation tissue with angiogenesis at the site of a tear at the annulus fibrosus that was detected as an HIZ on MRI and contrast leakage on CT discography. Based on these facts and the successful outcome of thermal annuloplasty, discogenic pain with inflammatory substances, angiogenesis, and nerve ingrowth at the area of HIZ may have been the main pain generator. Despite continuous administration of non-steroidal anti-inflammatory drugs and amelioration in the signal intensity of HIZ after the first surgery, she had intractable LBP even 4 weeks after the first surgery. Therefore, the major LBP generator was considered to be nerve ingrowth with symptomatic HIZ before the first surgery rather than inflammatory aggravation after the first surgery. Even if LBP improves after selective nerve root block, we cannot rule out the possibility of concomitant discogenic LBP. This finding represents the difficulty in the detection of pain generators. Additionally, the patient had sensory disturbance below the T10 spinal level, which might hamper the accurate diagnosis of pain generators. Although a case report demonstrated the effectiveness of epidural opioid therapy in a patient with incomplete tetraplegia and disk herniation during pregnancy,16) no reports described the effectiveness of selective nerve root block and discoblock in patients with plegia. Although more careful interpretation is required in patients with sensory disturbance, our case would suggest the diagnostic value of discography and discoblock even in a patient with partial sensory disturbance.
Treatment of discogenic LBP with HIZVarious treatment modalities have been described based on the consideration of an HIZ as a potential source of discogenic LBP. Interbody fixation is the most common surgery for discogenic pain.17) However, we cannot overlook the damage to the back muscles and the decrease in mobility of segments in athletes. Intradiscal electrothermal therapy is another option that can preserve segmental mobility.18) However, intradiscal electrothermal therapy could induce severe disk degeneration compared to thermal annuloplasty under full-endoscopy. Although the effectiveness of thermal annuloplasty without endoscopy is still controversial,19) recent studies of thermal annuloplasty with FED can provide direct visualization of the vascularized granulation tissue that correlates with the location of the HIZ, leading to excellent clinical outcomes with safer and more accurate radiofrequency coagulation.20,21) Although this procedure requires additional discectomy via the inside of the disk, which may lead to future disk degeneration, in order to secure a space for radiofrequency coagulation, it might have been better to perform thermal annuloplasty in the initial surgery for an early return to sports in the present case. In contrast, discectomy alone could improve her pain at the third surgery. However, she strongly hoped to take part in an important competition 2 months after the third surgery. We could not deny the possibility of nerve re-ingrowth because of temporary pain relief by discoblock before the third surgery. Because her LBP improved after the second surgery, we selected discectomy and thermal annuloplasty to surely achieve return to play within 2 months.
Special consideration for para-athletesPara-athletes may have different health issues compared to non-disabled athletes due to their disabilities and/or mobility aids, such as a wheelchair or prosthetic devices. This increases the complexity of strategies designed to reduce injury risk.22) Therefore, it is indispensable to develop a treatment plan with individualized approaches based on the specifics of the sport and the competition level. However, there is little evidence regarding the management of sports injuries in para-athletes. The shoulder is the most common region of sports injuries in non-ambulatory para-athletes.23,24) Accordingly, few authors have reported the management of LBP and LDH in para-athletes. In the present case, the onset and recurrence of LDH may have been due to the patient's poor trunk function, which was the pitfall in the management. Risk factors related to the recurrence of disk herniation include obesity, smoking, and the presence of comorbidities such as diabetes.25) Non-ambulatory para-athletes may be at increased risk for LDH when participating in sports. Additionally, poor trunk function itself would likely cause discogenic LBP due to insufficient support of spinal motion. In fact, the patient's LBP was relieved by bracing. We should have more carefully considered the postoperative rehabilitation program and the timing of returning to sports based on her disorder. The importance of the core for stabilization of the spine and production of a high force in most sports and everyday physical activities has been largely recognized. In para-sports, performance ability in wheelchair basketball was associated with trunk stability.26) Additionally, Bjerkefors et al.27) demonstrated that postural stability in patients with thoracic spinal cord injury could be improved by kayak ergometer training. Therefore, trunk rehabilitation would be important for patients with paraplegia. However, little evidence regarding trunk rehabilitation in patients with paraplegia and para-athletes exists. This might be because of difficulty in improving the strength of core muscles in most patients with paraplegia. In fact, the patient was not able to do core muscle training. Therefore, we aimed to rehabilitate thoracic spine movement to reduce mechanical stress in the affected segment after the third surgery, which may contribute to preventing recurrence after the third surgery. The timing of returning to sports might have needed more careful consideration, as the patient was unable to perform sufficient core muscle training.
In conclusion, we reported the case of an elite para-athlete with LDH and HIZ in which LBP was difficult to diagnose and treat. Adequate attention is required to accurately diagnose and develop an individualized treatment plan with specific approaches for para-athletes with LDH and HIZ based on the specifics of the sport modality and their impairments. Discography and discoblock would be useful even in a patient with partial sensory disturbance. FED with thermal annuloplasty and rehabilitating thoracic movement can be an excellent option for para-athletes with paraplegia and intractable discogenic LBP.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Informed consent was obtained from the patient for the publication of this case report and the accompanying images.
There are no conflicts of interest to declare.