2025 Volume 12 Pages 181-188
2025 Volume 12 Pages 181-188
Intracranial solitary fibrous tumor is a rare tumor accounting for 0.4% of intracranial tumors, with a high local recurrence rate and a tendency toward metastasis outside the central nervous system. We experienced a case of distant metastasis to the soft tissues and the kidney without local recurrence after gross total resection of the primary intracranial tumor. A 58-year-old male with cognitive impairment and right hemianopsia had a tumor of 5 cm maximum diameter in the left occipitotemporal convexity. Magnetic resonance imaging examinations showed a tumor with a slightly high signal on T1-weighted images, a low signal on T2-weighted images, and uniform and prominent contrast-enhanced images. Intratumoral flow voids were markedly observed. A head computed tomography performed 3 years earlier showed no mass lesions in the same region. Following tumor embolization, a gross total tumor resection was performed. The pathological diagnosis was grade-1 solitary fibrous tumor according to the 2021 World Health Organization central nervous system 5 criteria. A total of 45 Gy of postoperative local radiation therapy was administered. The patient recovered from his cognitive impairment and his right hemianopsia also improved. Although subsequent imaging studies showed no local recurrence, over 8 years after surgery, distant metastases were found in the subcutaneous soft tissue of the medial right femur and the left kidney, all of which were surgically removed. In a literature review, we identified 213 cases of intracranial solitary fibrous tumor having distant metastases with or without local recurrence from 18 reports and found that ours was the ninth case of distant metastasis despite gross total resection without local recurrence.
Solitary fibrous tumors (SFTs), first described by Stout and Murray in 1942, are mesenchymal tumors that are frequently found in the thoracic cavity and soft tissues, although they can occur anywhere in the body.1) In the central nervous system, SFTs are rare tumors, and when they do occur, they often arise from the dura mater and resemble meningiomas on imaging; they account for 1.9% to 4% of all meningeal tumors and 0.4% of intracranial tumors.2-4) The average age at onset is in patients in their 40s to 50s, with a slightly higher incidence in the male population. SFTs are vascular-rich tumors with high rates of local recurrence and distant metastasis, with recurrent and metastatic events often occurring 10 to 20 years after initial diagnosis. In the 2021 World Health Organization (WHO) classification, SFT is histopathologically classified as a non-meningeal stromal epithelial tumor, with 3 grades: 1, 2, and 3.5) Grade 3 SFTs, formerly known as anaplastic hemangiopericytomas, tend to metastasize extracranially and frequently recur.2-4)
In the present report, we report a case of distant metastasis despite the absence of local recurrence after gross total resection (GTR) and local radiation therapy (RT) of an intracranial SFT, along with a review of the literature.
The patient was a 58-year-old male who presented to our hospital with a chief complaint of cognitive impairment and right homonymous hemianopsia. He had a history of hypertension, hepatitis C, and gastric submucosal tumors. Brain magnetic resonance imaging (MRI) examinations showed a mass lesion with a 5 cm diameter in the left occipitotemporal convexity. On MRI, the tumor showed a slightly high signal on T1-weighted images and a low signal on T2-weighted images with homogeneous and marked contrast-enhanced effects (Fig. 1A-C). Flow voids were clearly observed inside the tumor, suggesting the presence of rich blood vessels, and some areas of necrotic or cystic lesions were also observed. Contrast-enhanced computed tomography (CT) examinations also showed a marked enhancement effect, suggesting a highly vascularized tumor. A head CT scan performed when the patient had a head injury 3 years earlier showed no mass lesion in the same area. Because the patient had undergone surgery for a gastric submucosal tumor 2 years earlier, a contrast CT scan of the body was performed to rule out a metastatic brain tumor. However, no obvious neoplastic lesion was found.
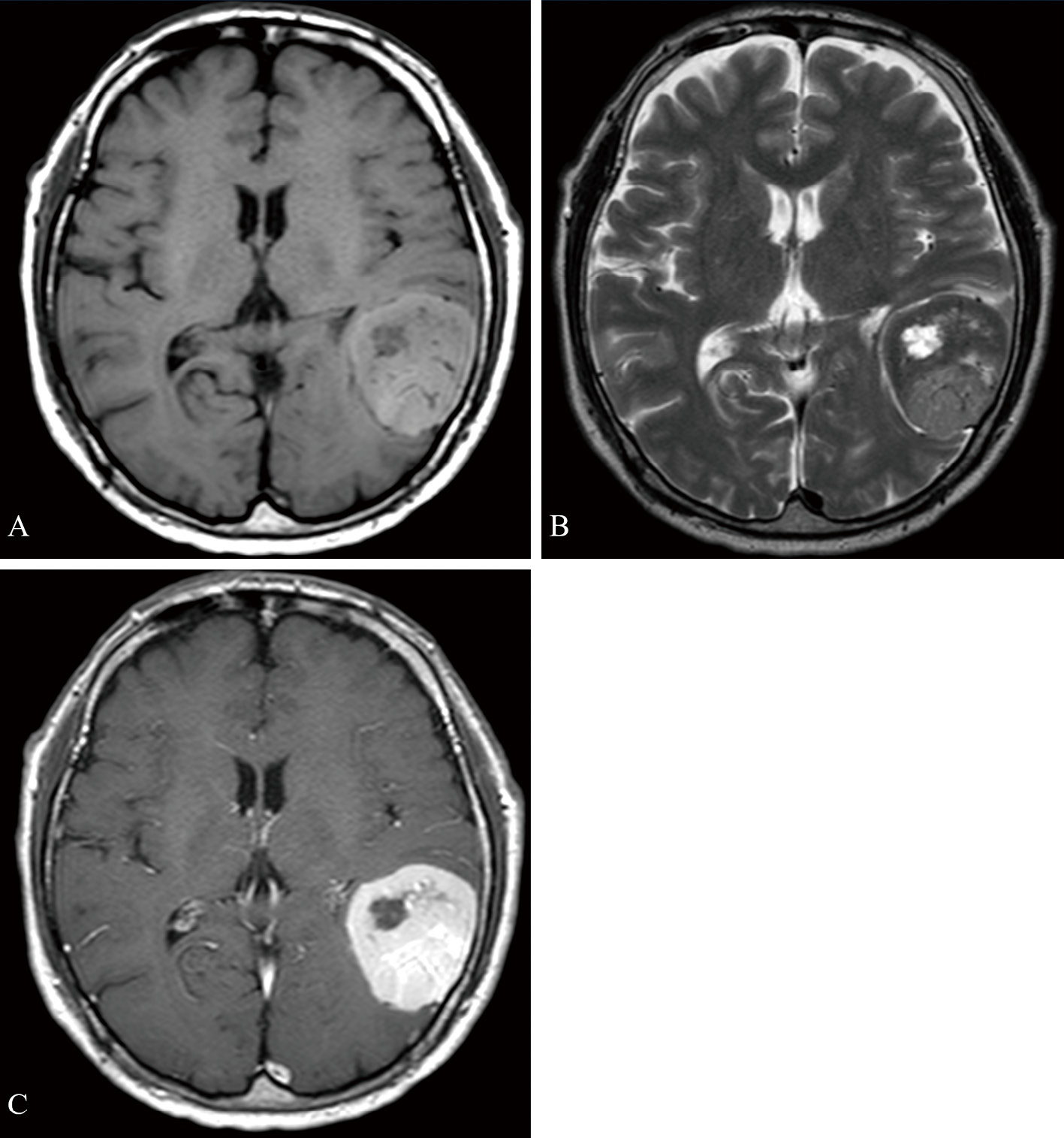
Preoperative magnetic resonance imaging (MRI) findings of the brain tumor.
A. The axial T1-weighted view showed a mass lesion with a diameter of 5 cm in the left occipitotemporal convexity with slightly high signal and internal low signal areas.
B. The axial T2-weighted view showed a tumor with low to equal signal and internal high signal areas. Flow voids were clearly observed inside the tumor.
C. The contrast-enhanced T1-weighted view indicated uniform and marked enhancement.
Cerebral angiography showed abundant tumor shadows fed from the left occipital artery (OA), the middle meningeal artery (MMA), the meningohypophyseal trunk, and the right posterior cerebral artery (PCA), so tumor embolization was performed using 20% n-butyl-2-cyanoacrylate (NBCA) on feeders of the left OA and MMA. The day after the embolization, the patient underwent craniotomy in the right lateral recumbent position under a surgical navigation system. The tumor was reddish brown and hemorrhagic. A partial incision made for rapid collection of intraoperative specimens resulted in significant hemorrhage, suggesting that internal decompression at this point would be difficult. Because several feeding arteries were observed mainly on the posterior surface of the tumor and were thought to be branches from the PCA, detachment from the normal brain was started from this posterior surface. Because the tumor turned white after detachment of its upper, anterior, and inferior surfaces, internal decompression was performed using a Sonopet Ultrasound Aspirator (Stryker, Kalamazoo, MI, USA), followed by detachment of the medial surface from the normal brain, and then total removal of the remainder of the tumor. Because the tumor was tightly attached to the dura mater of the convexity area, the dura mater of this area was resected and replaced with periosteum. Because the tumor was also attached to the transverse venous sinus, electrocoagulation was performed in this region, leading to a GTR of Simpson's grade 2. The operative time was 5 hours and 41 minutes, with a blood loss of 460 mL.
Histologically, the tumor was an SFT, grade 1 according to the 2021 WHO central nervous system 5 (CNS5) criteria and grade II according to the 2016 WHO CNS4 criteria, with pale acidophilic cytoplasm and short spindle-shaped cells proliferating with a delicate vascular network, with no significant nuclear atypia or fission (Fig. 2A and B). Immunohistochemical examinations indicated that the tumor was diffusely positive for Cluster of Differentiation 99 (CD99) and positive for signal transducer and activator of transcription 6 (STAT 6) with no significant positive images for Epithelial Membrane Antigen (EMA), Progesterone Receptor (PgR), S-100, Cluster of Differentiation 34 (CD34), or c-kit, and the Ki-67 labeling rate was about 10% (Fig. 2C-E). A total of 45 Gy of local RT was given postoperatively. The patient recovered from his cognitive impairment in the early postoperative period, with no new neurological abnormalities appearing. His right hemianopsia also improved.

Pathological findings of the brain tumor.
A and B. The tumor was an SFT, grade 1 according to the 2021 WHO CNS5 criteria and grade II according to the 2016 WHO CNS4 criteria, with pale acidophilic cytoplasm and short spindle-shaped cells proliferating with a delicate vascular network, with no significant nuclear atypia or fission (hematoxylin and eosin staining; A: original magnification ×100; B: original magnification ×400).
C, D, and E. Immunohistochemical examinations indicated that the tumor was diffusely positive for CD99 (C: original magnification ×400) and STAT6 (D: original magnification ×400), and the Ki-67 labeling rate was about 10% (E: original magnification ×400).
WHO CNS5: World Health Organization central nervous system 5
Thereafter, the patient underwent annual outpatient follow-up with contrast-enhanced MRI until after the 7-year postoperative examination, when he stopped visiting our neurosurgery department; no local recurrence was apparent in these imaging studies. In addition, because of a previous surgical history of gastric mucinous tumor, a contrast CT examination of the trunk was performed once a year until the patient stopped visiting our gastrointestinal surgery department in the fourth postoperative year; these examinations revealed no neoplastic lesion in either the kidneys or femur. Nine years after brain surgery, the patient was admitted to our hospital due to ascites effusion resulting from cirrhosis; a contrast-enhanced CT examination was performed and revealed a mass lesion with a maximum diameter of 1.3 cm in the left kidney. Because the lesion did not respond to contrast, a renal cyst was suspected and the patient was followed up with imaging examinations. In addition, at 10 years after the brain surgery, the patient visited the orthopedic surgery department of another hospital due to a mass in his right femur, which had been gradually increasing since he first noticed it 2 years earlier. A contrast-enhanced MRI examination showed an 8 cm-long subcutaneous soft tissue mass on the medial side of the right femur (Fig. 3A), although a contrast-enhanced MRI scan of the head showed no obvious recurrence of the primary tumor (Fig. 3B). Finally, upon contrast-enhanced CT examination of the lesion in the femur, the known left renal lesion was found to have increased to a maximum diameter of 2.8 cm, with contrast enhancement, and another lesion with a maximum diameter of 1.4 cm had also appeared (Fig. 3C).

Magnetic resonance imaging (MRI) and computed tomography (CT) findings at the time of metastasis more than 10 years after the initial surgery.
A. MRI of the lower extremity showed an 8 cm long subcutaneous soft tissue mass on the medial side of the right femur. The mass was clearly bordered by the surrounding area, with heterogeneous internal contrast and a flow void.
B. Brain MRI contrast-enhanced T1-weighted images showed no obvious recurrence of the primary tumor.
C. Contrast-enhanced CT of the trunk showed two tumors with maximum diameters of 2.8 cm and 1.4 cm and a uniform contrast effect in the left kidney (white arrows).
These postsurgical lesions were treated as follows. First, the femoral lesion underwent total resection at another hospital 10 years after brain surgery. The pathology was diagnosed as SFT, and immunohistochemistry showed that the tumor was STAT6-positive, indicating that it was likely a distant metastasis of the brain SFT. Then, 11 years after the brain tumor surgery, total resection of the kidney lesions was performed at the urology department of this hospital, because they were suspicious for renal cell carcinoma. These pathological findings also indicated SFTs and the immunohistochemistry was positive for STAT6, again indicating a likely distant metastasis from the brain SFT. Eleven years after the primary brain surgery, the patient is stable and leading a normal daily life, and is undergoing regular imaging follow-up with whole-body MRI from the head to the peripheral lower extremities.
Two major reviews of intracranial SFTs have been reported.3,4) Ratneswaren et al.4) reviewed reports on intracranial SFTs from 1980 to 2018, to identify common sites of metastases, and the timing of onset, of 347 metastases of 213 patients from 71 reports. Giordan et al.3) reviewed all reports on intracranial SFT from 2000 to 2020 and examined predictors of recurrence, metastasis, and death in 368 cases of intracranial SFT in 29 reports. According to their reviews, distant metastases of intracranial SFT are often observed, with an incidence of 17.5% to 28% of patients with intracranial SFT. Metastases can occur in any age group, the location of metastases varies, and metastases are often diagnosed after symptoms appear. In a review by Giordan et al.,3) the lungs were reported as the most common site of metastasis (32.1%), followed by bone, while Ratneswaren et al.4) found that the most common site was bone (19.6%), followed in order by lung and pleura (18.4%), liver (17.6%), and spine (14.1%).
We searched the literature for reports of intracranial SFT with distant metastases with or without local recurrence that included information on the method of initial removal of the primary tumor (GTR or subtotal resection [STR]) and identified 213 cases from 18 reports (Table 1).6-23) Of the 213 cases reviewed, 125 had GTR, 104 had primary recurrence, and 44 had distant metastasis. Excluding reports that considered only recurrent cases, the primary recurrence rate was 39% (71/180 cases) and the distant metastasis rate was 18% (33/180 cases). Cases of distant metastasis without local recurrence after GTR are quite rare. Indeed, to the best of our knowledge, only 8 such patients have been reported to date,12) making our present case the ninth. We summarize the details of these 9 cases of distant metastasis without local recurrence after GTR in Table 2. The average age of the cases was 43.3 years old (range: 23 to 67 years). The follow-up period was about 10 years, and bone and lungs accounted for about half of the metastatic sites. Although a previous review reported that there have been no patients with recurrence or systemic metastasis after GTR of hemangiopericytomas grade II,14) our present case was grade II. The present patient had distant metastasis to the soft tissues and kidneys. The kidneys are a relatively rare metastatic site in intracranial SFT, based on a report by Ratneswaren et al.4) in which only 14 cases of metastasis to the kidneys were observed among 347 cases of intracranial SFT with distant metastases.
Reports of intracranial solitary fibrous tumor with distant metastases
| Ref no. | Case no. | Extent of surgery | Grade | RT | Rec | Meta | Meta w GTR wo Rec | Location of metastasis |
|---|---|---|---|---|---|---|---|---|
| Details of the included reports: number of patients with local recurrence and distant metastases, extent of resection and CNS4 WHO grade of the primary tumor in these patients. *The malignancy grade in reference 9 was described as grade 3 according to the WHO CNS5 criteria, but based on the histopathologic description, it was determined to be grade III also according to the WHO CNS4 criteria. CNS: central nervous system; GII: CNS4 WHO grade II; GIII: CNS4 WHO grade III; GTR: gross total resection; Meta w GTR wo Rec: cases of distant metastasis without local recurrence after gross total resection; Meta: distant metastasis; NI: no information; Rec: local recurrence; Ref no.: reference number; RT: radiation therapy; STR: subtotal resection; WHO: World Health Organization |
||||||||
| 6 | 1 | GTR 1 | NI | 0 | 1 | 1 | 0 | bone |
| 7 | 14 | GTR 7, STR 7 | NI | NI | 6 | 7 | 0 | bone, liver, peritoneum, intestine |
| 8 | 1 | GTR 1 | GII | 0 | 1 | 1 | 0 | bone, liver |
| 9 | 1 | GTR 1 | GIII* | 1 | 0 | 1 | 1 (RT) | bone, lung |
| 10 | 19 | GTR 9, STR 1 | NI | 8 | 3 | 10 | 3 (RT 2) | lung, bone, liver |
| 11 | 2 | STR 2 | NI | 0 | 2 | 2 | 0 | bone |
| 12 | 15 | GTR 15 | GII 10, GIII 5 | 3 | 3 | 0 | 0 | |
| 13 | 13 | GTR 9, STR 4 | GII 6, GIII 7 | 11 | 6 | 0 | 0 | |
| 14 | 10 | GTR 6, STR 4 | GII 4, GIII 6 | 1 | 2 | 2 | 1 (RT) | hip, bone |
| 15 | 10 | GTR 7, STR 3 | NI | 0 | 3 | 0 | 0 | |
| 16 | 15 | GTR 13, STR 2 | NI | 6 | 12 | 1 | 0 | bone |
| 17 | 11 | GTR 10, STR 1 | NI | 10 | 3 | 4 | 1 | lung, liver, bone |
| 18 | 12 | GTR 10, STR 2 | NI | 5 | 4 | 0 | 0 | |
| 19 | 12 | GTR 5, STR 7 | NI | 1 | 7 | 1 | 0 | lung, liver |
| 20 | 15 | GTR 8, STR 7 | NI | 15 | 15 | 4 | 0 | lung, lymph node |
| 21 | 17 | GTR 13, STR 4 | NI | 10 | 10 | 3 | 1 (RT) | bone, thyroid, lung |
| 22 | 14 | GTR 5, STR 9 | NI | 10 | 14 | 3 | 0 | lung, liver, skin |
| 23 | 31 | GTR 29, STR 2 | NI | 17 | 12 | 4 | 1 (RT) | liver, lung, bone |
| Total no. | 213 | GTR 125, STR 88 | 98 | 104 | 44 | 8 | ||
Details of cases of distant metastasis with gross total resection without local recurrence
| Ref no. | Grade | RT | Age of first diagnosis | Sex | Follow-up period | Location of metastasis |
|---|---|---|---|---|---|---|
| The nine cases of distant metastasis with gross total resection without local recurrence, including CNS4 WHO grade, radiation therapy, age of first diagnosis, sex, follow-up period (years), location of metastasis. *The malignancy grade in reference 9 was described as grade 3 according to the WHO CNS5 criteria, but based on the histopathologic description, it was determined to be grade III also according to the WHO CNS4 criteria. CNS: central nervous system; F: female; GII: CNS4 WHO grade II; GIII: CNS4 WHO grade III; Grade: CNS4 WHO grade; M: male; NI: no information; Ref no.: reference number; RT: radiation therapy; WHO: World Health Organization |
||||||
| 9 | GIII* | y | 65 | M | 4 | bone, lung |
| 10 | NI | y | 26 | F | 11 | bone, lung |
| 10 | NI | n | 29 | F | 22 | lung |
| 10 | NI | y | 43 | F | 10 | lung, liver |
| 14 | GIII | y | NI | NI | 5 | hip, bone |
| 17 | NI | n | 67 | M | 4 | bone |
| 21 | NI | y | 35 | F | 15 | bone, thyroid, lung |
| 23 | NI | y | 23 | F | 10 | femur |
| present case | GII | y | 58 | M | 10 | femur, kidney |
It has been reported that the NGFI-A binding protein 2 (NAB2)-signal transducer and activator of transcription 6 (STAT6) fusion gene is the driver mutation of SFT,24) and the fusion of STAT6 and NAB2 causes cytoplasmic STAT6 to migrate to the nucleus, which can be detected by immunostaining with anti-STAT6 antibody, making this antibody useful for the diagnosis of SFT.25) The fact that the femoral and renal lesions in the present case were STAT6-positive, as were the brain SFTs, indicated that these lesions were likely metastases of the primary intracranial SFT.
A significantly higher risk of recurrence has been reported in STR with CNS4 WHO Grade III SFT,3) and surgical resection followed by RT may serve to reduce the risk of local recurrence but not metastasis.21) RT combined with STR leads to improved survival compared to STR alone.3) GTR and adjuvant RT were reported to significantly improve survival as compared with STR and no RT, respectively.2) We believe that long-term follow-up is necessary, bearing in mind that distant metastasis may occur even in the absence of local recurrence, as in the present case. When adjusted for studies with more than 10 years of follow-up, 1 in 1.4 to 8.6 patients with primary intracranial SFT have been reported to develop extracranial metastases.4) The median time after primary lesion was 3.25 years (0.5-12.3 years).3) However, there has been a report of extracranial metastases 31 years after the initial diagnosis.26) Therefore, patients with intracranial SFT require regular and long-term clinical and imaging follow-up for recurrence as well as extracranial metastases.3) It has been pointed out that follow-up with whole-body positron emission tomography/CT scans is not suitable because it exposes patients to a relatively significant dose of radiation, which increases the lifetime risk of carcinogenesis.27) We therefore perform imaging follow-up with whole-body MRI for patients with distant metastasis, as in this case. For patients with distant metastatic risk, such as recurrence of the primary tumor, high histologic grade, or STR, we believe that annual follow-up with a whole-body CT or MRI examination that can cover the lungs, bones, soft tissues, liver, and spine, all of which are favorable sites for distant metastasis, is advisable for 10 years, with continued follow-up thereafter at a rate appropriate for the individual case. Even for patients who do not have these metastatic risks, it may be desirable to follow up with CT or MRI examinations for 5 years after surgery, when metastasis is considered to be more common. However, it should be noted that some cases, including the present case and the others summarized in Table 2, may develop distant metastases more than 5 years after surgery, even though they do not have these metastatic risks. In cases where imaging of the entire body is not feasible, options such as limiting imaging to the lungs, liver, and spine, which are the predominant sites of metastasis, could be considered.
In conclusion, although intracranial SFT is a rare tumor accounting for 0.4% of intracranial tumors, with a high local recurrence rate and a tendency toward extracranial metastases, we experienced a case of distant metastasis to the soft tissues and kidneys without local recurrence over 8 years after GTR. A review of the literature indicated that, among 213 cases of intracranial SFT with distant metastasis with or without local recurrence from 18 reports, our case was only the ninth case of distant metastasis without local recurrence after GTR.
There are no conflicts of interest.