2020 Volume 5 Article ID: 20200002
2020 Volume 5 Article ID: 20200002
Background: Descending necrotizing mediastinitis is a potentially fatal polymicrobial infection that often leads to dysphagia after treatment. Such dysphagia is likely the result of fibrosis and scarring from inflammatory changes in the fascial space. A case is presented in which the mechanism of dysphagia was verified using two-dimensional analysis of the muscle lengths of the suprahyoid and infrahyoid muscles. Case: A 57-year-old woman presented with a hyoid and laryngeal movement disorder with pharyngeal residue secondary to descending necrotizing mediastinitis. To treat this disorder, the chin-down maneuver was performed, and it immediately improved hyoid and laryngeal elevation and reduced pharyngeal residue at the epiglottic valleculae and pyriform sinus. Analysis of the mechanism of these improvements revealed that combined head and neck flexion, compared with neck flexion, decreased the distance between the origin and insertion (DOI) of the sternohyoid muscle (SM) and increased the muscle contraction rate and the maximum contraction duration of the geniohyoid muscle (GM) during swallowing. Discussion: In the present case, the patient had restrictions in extension of the SM that applied resistance to GM contraction. Compensation of this condition was achieved by combined head and neck flexion, which decreased the DOI of the SM, thereby improving the contractile function of the GM.
Cervical necrotizing fasciitis, commonly of pharyngeal, tonsillar, or odontogenic origins, is a rare polymicrobial infection. Reports show that in 40–45% of cases, cervical necrotizing fasciitis spreads rapidly to the mediastinum, often becoming fatal.1) Prompt diagnosis and treatment of descending necrotizing mediastinitis (DNM), e.g., securing the airway, administering antibiotics, performing drainage, and providing intensive care for sepsis, can contribute to improved survival. Complications include a compromised airway, jugular vein thrombosis, suppurative jugular thrombophlebitis (Lemierre’s syndrome), carotid artery erosion and rupture, septic shock, empyema, and a bronchocavitary fistula.2)
Dysphagia can persist after DNM treatment. Such dysphagia is thought to be caused by movement disorder of the hypopharyngeal muscle and hyoid/thyroid cartilage that develops as a result of fibrosis and scarring caused by the inflammatory changes in the fascial space.3,4) However, the mechanism remains a matter of speculation. There are very few reports on rehabilitation for this condition,5) probably because of the absence of detailed swallowing evaluations. This report describes the intensive rehabilitation and videofluorographic swallowing study (VFSS) performed after DNM diagnosis. The chin-down procedure was successful in treating dysphagia in the present patient; however, no similar reports have been published to date. Consequently, a two-dimensional analysis of the lengths of the suprahyoid muscles (SHMs) and infrahyoid muscles (IHMs) was conducted to determine whether the chin-down compensation mechanism is consistent with the hyoid and laryngeal movement disorder caused by fibrosis and scarring, as suggested by previous reports.
A 57-year-old woman visited her local physician because of severe throat pain, a swollen neck, and a high fever that had persisted for several days. Ten days before the visit, dried anchovy became lodged in the patient’s throat. The patient did not have a medical history suggestive of a high risk of infection (e.g., diabetes mellitus) or decreased swallowing function (e.g., stroke). Computed tomography showed a deep bilateral neck abscess and inflammation from the neck to the mediastinum, along with gas formation. With the diagnosis of DNM, the patient was transported and admitted to an emergency hospital. On the same day, bilateral cervical drainage and thoracic surgical drainage with video-assisted thoracoscopy from the left thoracic cavity were performed. Postoperatively, antibiotic treatment, sepsis management, and peripheral parenteral nutrition were continued. One week after admission, tracheostomy was performed, and nasogastric tube feeding and physical therapy, including respiratory function training, were started. Four weeks after admission, the inflammatory response, neck abscess, and mediastinitis improved. A jelly diet was started, but the patient developed mild hoarseness (breathy/wet) and showed bilateral vocal cord paresis on laryngoscopy. The patient’s oral intake was level 3 on the Functional Oral Intake Scale (FOIS).6) A VFSS showed poor hyoid and laryngeal elevation. To avoid water aspiration, thickening of the diet was required. With a paste diet, significant pharyngeal residue was present at the epiglottic valleculae and bilateral pyriform sinuses, and several swallows were required to remove the residue. Five weeks after admission, swallowing exercises (i.e., neck range of motion exercise, Shaker exercise, and effortful swallow) were started with a speech-language pathologist. The FOIS improved to level 4, and the patient achieved independent activities of daily living, including gait, and was transferred to our hospital 6 weeks after admission for dysphagia rehabilitation. At the start of swallowing exercises and at the time of hospital transfer, undernutrition was not evident, based on nutrition management screening, such as blood test results.
Similar exercises and the jelly diet established by the previous physician were continued, and the tracheal cannula (button type) was removed 7 weeks after admission. No obvious restrictions in the range of motion of the head and neck were observed. On laryngoscopy, vocal cord atrophy was evident, but vocal cord paralysis had improved. A VFSS done 8 weeks after admission showed that water without thickening could be swallowed without aspiration, and residue in the epiglottic valleculae was reduced with the paste diet. However, poor hyoid and laryngeal elevation was evident, and multiple swallows were required to remove the residue. The FOIS improved to level 5. A VFSS performed 10 weeks after admission also did not show changes in hyoid and laryngeal elevation or residue at the epiglottic valleculae and pyriform sinus. There were no obvious differences in the pharyngeal passage between the left and right sides, and head rotation had no effect.
However, when a reduction in pharyngeal residue was attempted with the chin-down maneuver, immediate improvement was achieved with combined head and neck flexion (CHNF), a finding not observed with neck flexion (NF) alone. In other words, hyoid and laryngeal elevation improved, and the paste diet could be swallowed without residue in the epiglottic valleculae and pyriform sinuses. With such progress, after discharge, the patient was able to transition stepwise from a jelly diet (FOIS: level 4) to a soft diet (FOIS: level 6). Indeed, by discharge, the patient was already dropping her head voluntarily in a chin-down posture when swallowing. Patient information about this case of dysphagia was shared among the transdisciplinary team to determine whether to step up or maintain the food form. However, undernutrition was not evident, and nutritional concerns were not raised by the attending physician’s team.
We postulated that the impairment of IHM extension resulting from fibrosis and scarring caused the dysphagia, compensation for which could be immediately achieved by the chin-down maneuver. In other words, CHNF shortened the distance between the origin and the insertion (DOI) of the IHMs, resulting in a relative relaxation of resting IHMs, thereby immediately compensating for the impaired contraction of the SHMs.
To test this hypothesis, we proposed a measurement method from an integrated perspective to simultaneously analyze the lengths of SHMs and IHMs in two-dimensions and conducted the following validation study using VFSS. Informed consent to publish this case study was obtained from the patient.
Outcome MeasurementsA VFSS was performed 10 weeks after admission. As shown in Fig. 1, the patient sat in a comfortable 60° reclining position to stabilize the chin-down posture. She was asked to swallow 3 ml of barium water or barium paste with NF or CHNF on command. This was repeated six times, and lateral-view images were recorded.
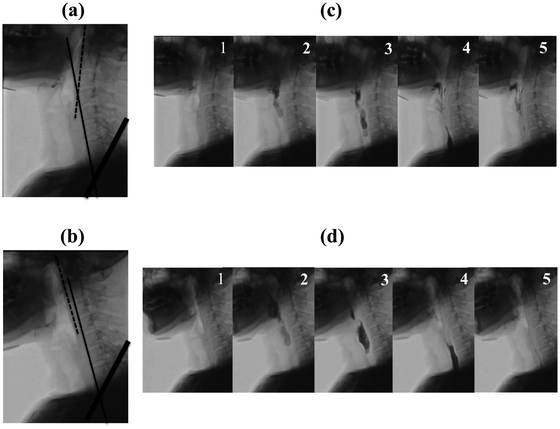
Parts (a) and (b) depict the chin-down posture. (a) NF: The thin black line connecting the upper margins of the C5 and C6 anterior vertebral bodies forms a 40° neck flexion (NF) from the bold black line showing a 60° reclining posture. The dashed black line connecting the lower margins of the C1 and C2 anterior vertebral bodies creates a 15° extension (physiological cervical lordosis) from the thin black line. (b) CHNF: The thin black line depicts a 45° NF from the bold black line. The dashed black line is parallel (straight neck) in reference to the thin black line due to a 15° HF. Parts (c) and (d) show the VFSS results. Chronological changes in swallowing (3 ml barium paste) are shown from 1 to 5. (c) NF: Residue at the epiglottic valleculae and pyriform sinuses. (d) CHNF: No residue at the epiglottic valleculae and pyriform sinuses.
Recorded frame-by-frame images (30 frames per second) of the following four endpoints were evaluated using two-dimensional motion analysis software (DIPP-Motion PRO 2D, DITECT Corporation, Tokyo, Japan).
1) DOI of the Sternohyoid MuscleBecause the origin and insertion of both the right and left sternohyoid muscles (SMs) run parallel to the midline of the anterior neck, we postulated that the outcome measure would be similar to the actual muscle length even when measured as a virtual muscle length on the VFSS lateral view. The DOI of the SM (DOI-SM) was measured as the distance between the upper end of the manubrium of the sternum and the central portion of the hyoid bone [Fig. 2(a)].

(a) Distance between the origin and insertion of the SM, and (b) and (c) distance between the origin and insertion of the GM. (b) Hyoid in the anterior displacement start position, and (c) hyoid in the anterior displacement end position.
In the lateral view of the VFSS, the hyoid bone during oropharyngeal swallowing typically moves in the superior direction from the resting position, followed by displacement in the anterior direction and a subsequent return to the resting position. It has been reported that, of the SHMs, the mylohyoid muscle has the greatest potential to displace the hyoid bone in the superior direction, and the GM has the greatest potential to displace the hyoid bone in the anterior direction.7)
Because the origin and insertion of both the right and left GMs run parallel to the midline of the lower jaw, we postulated that the outcome measure would be similar to the actual muscle length, even when measured as a virtual muscle length on the VFSS lateral view. This distance was measured with the hyoid in the anterior displacement start position (b) and the anterior displacement end position (c) [Fig. 2(b), (c)].
3) Muscle Contraction Rate of the GMThe DOI-GM was converted to the muscle contraction rate (MCR). The MCR of the DOI-GM was calculated as: MCR={[(b) minus (c)] divided by (b)}×100.
4) Maximum Contraction Duration of the GMUsing the first frame at the hyoid anterior displacement end position as a reference (zero), stationary frames of the hyoid at that position over time were counted and added: the maximum contraction duration (MCD) of the GM (s)=Total number of frames × 1/30
Data AnalysisAll statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM, Armonk, NY, USA), with P values <0.05 indicating significance. Normality was confirmed for the data of all groups using the Shapiro-Wilk test. The t-test was used to compare each parameter before and after the chin-down posture.
ResultsTable 1 shows the DOI, MCR, and MCD values for NF and CHNF.
| NF | CHNF | |||||
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | P | ||
| DOI of the SM (mm) | ||||||
| 3 ml liquid | 77.9 (0.9) | 77.0–78.9 | 68.1 (1.2) | 66.8–69.3 | 0.000* | |
| 3 ml paste | 77.5 (0.6) | 76.9–78.2 | 67.0 (1.2) | 65.7–68.2 | 0.000* | |
| DOI of the GM (mm) | ||||||
| 3 ml liquid | A | 35.3 (0.4) | 34.9–35.7 | 35.6 (0.3) | 35.1–36.0 | 0.274 |
| B | 26.5 (0.3) | 26.2–26.8 | 25.3 (0.3) | 24.9–25.7 | 0.000* | |
| 3 ml paste | A | 35.5 (0.6) | 34.9–36.1 | 35.1 (0.5) | 34.6–35.7 | 0.226 |
| B | 27.1 (0.6) | 26.5–27.7 | 24.3 (0.4) | 23.9–24.7 | 0.000* | |
| MCR of the GM (%) | ||||||
| 3 ml liquid | 24.9 (0.9) | 24.0–25.8 | 28.8 (1.3) | 27.4–30.1 | 0.000* | |
| 3 ml paste | 23.6 (0.9) | 22.6–24.6 | 31.1 (1.3) | 29.7–32.5 | 0.000* | |
| MCD of the GM (s) | ||||||
| 3 ml liquid | 0.78 (0.17) | 0.60–0.96 | 1.34 (0.31) | 1.02–1.66 | 0.001* | |
| 3 ml paste | 0.89 (0.17) | 0.71–1.07 | 1.67 (0.30) | 1.35–1.98 | 0.005* | |
CHNF: combined head and neck flexion, DOI: distance between the origin and insertion, GM: geniohyoid muscle, MCD: maximum contraction duration, MCR: muscle contraction rate, NF: neck flexion, SM: sternohyoid muscle, A: hyoid in the anterior displacement start position, B: hyoid in the anterior displacement end position.
P calculated by the t-test; *P <0.05.
Compared with NF, CHNF resulted in a significantly lower DOI-SM for both liquid (77.9 mm vs. 68.1 mm) and paste (77.5 mm vs. 67.0 mm).
2) DOI of the Geniohyoid MuscleCompared with NF, CHNF had a similar DOI-GM at the hyoid anterior displacement start position, but significantly lower DOI-GM at the hyoid anterior displacement end position for both liquid (26.5 mm vs. 25.3 mm) and paste (27.1 mm vs. 24.3 mm).
3) MCR of the Geniohyoid MuscleCompared with NF, CHNF resulted in a significantly higher MCR-GM for both liquid (24.9% vs. 28.8%) and paste (23.6% vs. 31.1%).
4) MCD of the Geniohyoid MuscleCompared with NF, CHNF resulted in a significantly longer MCD-GM for both liquid (0.78 s vs. 1.34 s) and paste (0.89 s vs. 1.67 s).
The chin-down maneuver is a postural technique widely used in dysphagia treatment. According to Logemann,8) one of the primary effects of the chin-down posture is the proximity of the tongue base and epiglottis to the posterior pharyngeal wall. This was corroborated in the present case, and a reduction in residue at the epiglottic valleculae with the chin-down posture was confirmed on VFSS.
Recently, Okada et al. reported that head flexion (HF), NF, and CHNF produce different effects on the anteroposterior dimensions of the valleculae and the pharyngeal lumen.9) Specifically, they showed that the changes in the relationship between the food pathway and the airway caused by the difference in the position of the head and neck explain the multifaceted effects of the chin-down posture.
Nevertheless, there is only one report, by Matsubara et al., that verified the swallowing pressure with three types of chin-down maneuvers (HF, NF, and CHNF).10) According to this report, NF was the position that lowered the upper esophageal sphincter swallowing pressure to the greatest and longest extent in healthy individuals. However, in the present study, NF, which was anticipated to reduce hypopharyngeal residue, was not effective. The addition of HF (CHNF) showed immediate improvement, indicating that swallowing pressure alone may not be appropriate to explain this effect.
To the best of our knowledge, there are no previous reports describing hyoid and laryngeal movement that classifies the chin-down maneuver into HF, NF, and CHNF categories. Leigh et al. reasoned that the horizontal hyoid movement of healthy subjects was suppressed by a chin-tuck because the submental muscles were compressed by the mandible, and the submental muscle was shorter than it was in a neutral position.11) However, the chin-down maneuver did not significantly affect hyoid movement. In other words, a comfortable chin-down position that does not change the length of resting SHMs does not affect the hyoid movement in healthy individuals. In the present study, both NF and CHNF were comfortable, and the length of the GM before contraction was not significantly different between the two positions.
Based on these findings, we postulated that the impaired extension of IHMs as a result of fibrosis and scarring was the cause of dysphagia, compensation for which could be immediately achieved in the present case by the chin-down maneuver. In other words, we hypothesized that CHNF shortens the DOIs of IHMs, resulting in a relative relaxation of resting IHMs, thereby immediately compensating for the contraction impairment of SHMs.
Mepani et al. used VF images of the thyrohyoid muscle,12) and Shimizu et al. used echo images of the GM13) for the two-dimensional analysis of muscle lengths. However, to the best of our knowledge, there are no studies in which simultaneous two-dimensional analysis of the lengths of SHMs and IHMs was performed from an integrated perspective. The measurement method in the present study was a two-dimensional analysis of the muscle length of SHMs and IHMs using lateral VF images; however, extensive use of this method will require additional studies to determine its reliability.
For CHNF compared with NF, we found that the DOI before the start of anterior hyoid displacement was similar for the GM but smaller for the SM. Furthermore, MCR and MCD of GM was higher for CHNF than for NF when swallowing liquid and paste.
In other words, fibrosis and scarring restrict the extension of the SM, which resists GM contraction. Compensation for this could be achieved by CHNF, which decreases DOI-SM, thereby improving the contractile function of the GM during swallowing. Although surgical invasion from cervical drainage and tracheostomy may have contributed to the fibrosis and scarring, it is likely that the above compensatory mechanism led to appropriate cricopharyngeal muscle opening and maintenance, thereby reducing residue at the pyriform sinus.
As described here, a movement disorder of the SHMs during swallowing can develop after DNM treatment because of extension impairment of the IHMs. The present report is the first to verify the mechanism by which compensation of this condition can be achieved by CHNF.
The way in which the DOI of IHMs is affected by flexion should be studied for all positions (HF, NF, and CHNF). We postulate, however, that the compensatory effect may work better in the chin-down posture with a deeper flexion than with a shallow flexion. The patient in the present case swallowed meals with CHNF, achieved by voluntarily dropping her head. In addition, we surmised that the patient swallowed in a head-dropped position without using the muscles around the neck to avoid contractions of the IHMs during the chin-down posture and simultaneous contractions of SHMs and IHMs during swallowing, especially since contraction of the IHMs plays a role in neck flexion.
However, in the present case, the high compensatory effect of CHNF may have been achieved because of the absence of obvious functional problems such as fibrosis and scarring of the SHMs. In the future, it will be necessary to examine the effects in a broader range of conditions, not limited to DNM, such as in inflammatory diseases or surgical procedures that may result in fibrosis, scarring, or shortening of the IHMs, as well as hypertonia of these muscles.
Dysphagia after DNM was successfully treated in this case with the chin-down procedure. The lengths of the SHMs and IHMs were analyzed in two dimensions using VFSS images to assess whether the compensation achieved by the chin-down maneuver is consistent with the previously-suggested hyoid and laryngeal movement disorder being caused by fibrosis and scarring. The present patient may have developed restrictions in extension of the SM, which applies resistance to GM contraction, and compensation for this condition was achieved by CHNF through the decreased DOI of the SM, thereby improving the contractile function of the GM.
The authors would like to thank Mr. Yukio Morohoshi, Radiological Technologist of Tokai University Oiso Hospital, for providing comments on our data. Furthermore, the authors would like to thank Ms. Emi Tada, Speech Language Pathologist of Tokai University Hospital, for providing detailed patient information.
No conflicts of interest have been reported by the authors or by any individuals in control of the content of this study.
Level 1: Nothing by mouth.
Level 2: Tube dependent with minimal attempts at food or liquid.
Level 3: Tube dependent with consistent oral intake of food or liquid.
Level 4: Total oral diet of a single consistency.
Level 5: Total oral diet with multiple consistencies, but requiring special preparation or compensations.
Level 6: Total oral diet with multiple consistencies without special preparation, but with specific food limitation