2020 Volume 5 Article ID: 20200023
2020 Volume 5 Article ID: 20200023
Objectives: To facilitate selection of the appropriate orthosis, this study assessed functional ambulation outcomes of subacute stroke patients using either an ankle–foot orthosis (AFO) or a knee–ankle–foot orthosis (KAFO).
Methods: The subjects were newly diagnosed hemiplegic stroke patients admitted to Hatsudai Rehabilitation Hospital between January and June 2016. Differences between the AFO group and the KAFO group were examined using unpaired t-tests. Multiple regression analysis with stepwise regression was used to identify predictive factors for the functional ambulation category (FAC) score at discharge.
Results: A total of 164 patients (99 men and 65 women; mean age, 69.2 ± 15.3 years; mean days from onset to admission, 31.9 ± 12.3 days) were included in the study. The AFO, KAFO, and non-orthosis groups contained 38, 79, and 47 patients, respectively. In the AFO group, the median Stroke Impairment Assessment Set (SIAS) motor scores were 2.5–3, and the median sensory scores were 2. In the KAFO group, the median SIAS motor scores were 0–1, and the median sensory scores were 1. At discharge, 32 (84.2%) patients in the AFO group and 20 (25.3%) patients in the KAFO group had an FAC score ≥3. Multiple regression analysis found that age and the Functional Independence Measure cognitive score could be used to predict the FAC score at discharge in the AFO group. The Berg Balance Scale score was an additional predictive factor in the KAFO group.
Conclusions: This study showed that the AFO group had good outcomes for independent ambulation. Furthermore, balance control is an important factor contributing to walking ability in patients with severe hemiparesis.
Loss of independent ambulation is the most disabling consequence of stroke and affects every aspect of activities of daily living (ADL).1) Although most stroke patients have gait disturbances at admission to a rehabilitation facility, approximately 60–70% of subacute stroke patients have regained the ability to walk independently at discharge.2)
The goal of intensive rehabilitation during the subacute phase of stroke is to improve basic mobility and ADL. Consequently, gait rehabilitation is the most important aspect of rehabilitation. The use of a lower extremity orthosis in hemiparetic patients promotes active rehabilitation and facilitates gait recovery.3,4,5,6) An ankle–foot orthosis (AFO) or a knee–ankle–foot orthosis (KAFO) may be used in patients with hemiparesis. An AFO is the most commonly used orthosis and provides (1) mediolateral stability at the ankle during the stance phase to prevent inadvertent twisting of the ankle; (2) dorsiflexion during the swing phase to prevent dragging of the toe, stumbling, and falling; and (3) push-off stimulation during the latter part of the stance phase, thereby approximating more normal gait and reducing energy expenditure. KAFOs are usually needed by patients who have weakness around the foot and ankle and are unable to stabilize the knee securely during the weight-bearing phase of the gait cycle. Selection of the most appropriate orthosis is important for gait rehabilitation and functional recovery of gait. Proper selection of orthoses depends on variables such as motor function, sensory function, age, and patient needs.
Few reports have shown differences in indications or outcomes for functional ambulation with AFO or KAFO in subacute stroke rehabilitation. Previous studies have used motor evaluations such as the Brunnstrom stage (BRS).3,5,6) However, these studies did not include detailed in-depth evaluations. To facilitate the selection of the most appropriate orthosis, the aim of this study was to assess impairment and functional ambulation outcomes of subacute stroke patients using either an AFO or a KAFO.
The participants were initial stroke patients with hemiparesis who were admitted to Hatsudai Rehabilitation Hospital from January to June 2016. Patients with infratentorial lesions, brainstem lesions, or subarachnoid hemorrhages were excluded. This study was approved by the institutional review board (No. H29-58), and written informed consent was waived because of the study’s retrospective design.
Clinical AssessmentsMedical records were reviewed retrospectively. Basic profiles (age, side of hemiparesis, and the mean time since stroke onset) were recorded. Lower extremity (LE) motor function and sensory function were assessed using the Stroke Impairment Assessment Set (SIAS)7) at admission and discharge. SIAS LE motor function examinations consisted of a hip flexion test (hip), a knee extension test (knee), and a foot tap test (foot). SIAS LE sensory items include light touch (touch) and position sense (position) scores.
Gait function was assessed based on the functional ambulation category (FAC)8) at admission and discharge. FAC grades gait ability from 0 to 5 according to the amount of physical support required. A score of 5 represents independent ambulation, 3 represents ambulation which is dependent on supervision, and 0 represents nonfunctional ambulation. We defined patients with an FAC score at discharge ≥3 as walkers and those with a score ≤2 as non-walkers.
The Berg Balance Scale (BBS) and Functional Independence Measure (FIM) motor and cognition scores were assessed at admission and discharge. The BBS was devised by Berg et al. and is a scale composed of 14 sitting and standing balance items. Each item is rated from 0–4.9,10) The scale is a balance evaluation tool that is relatively easy to perform in the clinical setting and addresses positions that are involved in ADL.
OrthosesWe prescribed the orthoses within a week of patient admission and classified patients into three groups according to the type of orthosis prescribed: AFO, KAFO, and no orthosis. The groups were based on the first orthosis introduced to each patient. In some patients, KAFOs were later changed to AFOs, and in other cases, patients continued to use KAFOs.
Statistical AnalysisDifferences between the AFO and KAFO groups were examined using unpaired t-tests. Differences between admission and discharge were compared using paired t-tests. The data were normally distributed. A P-value <0.05 was considered significant. Stepwise multiple regression analysis was conducted to determine variables that could predict the FAC score at discharge. The independent variables were age, sex, hemiplegia side, number of days from onset to admission, SIAS scores (hip, knee, foot, L/E touch, L/E position), BBS, and FIM cognitive score. To investigate possible collinearity or multicollinearity among the predicting variables, we used variance inflation factors (VIF) to detect multicollinearity in the regression analysis. A VIF greater than 5 is highly correlated, and we set the threshold for significant collinearity to be greater than 10. Statistical analyses were performed using IBM SPSS Ver. 25.
In total, 164 stroke patients (99 men and 65 women; mean age, 69.2 ± 15.3 years; range, 25 to 94 years) were included in the study. Ninety-two patients had right hemiplegia and 72 had left hemiplegia. The mean time since stroke onset was 31.9 ± 12.3 days, and the mean length of hospital stay was 102.3 ± 46.5 days.
Among the 164 participants, 38 used AFOs, 79 used KAFOs, and 47 used no orthoses. Table 1 shows the clinical characteristics of patients on admission. Comparisons between the AFO group and the KAFO group at admission showed significant differences in age (P=0.002), SIAS LE motor score (P<0.001), SIAS LE sensory score (P<0.001), BBS (P<0.001), FIM (motor, cognition) (P<0.001), and FAC (P<0.001).
| AFO (n=38) | KAFO (n=79) | P value | |
| Age | 62.6±15.9 | 72.3±15.2 | 0.002** |
| Sex | 0.366 | ||
| Male | 25 (65.8%) | 45 (57.0%) | |
| Female | 13 (34.2%) | 34 (43.0%) | |
| Hemiplegia | 0.561 | ||
| R | 20 (52.6%) | 37 (46.8%) | |
| L | 18 (47.4%) | 42 (53.2%) | |
| Days since stroke onset | 30.2±11.8 | 34.2±12.0 | 0.092 |
| Days of hospital stay | 105.8±37.9 | 119.3±45.7 | 0.12 |
Data are mean±SD.
AFO, ankle–foot orthosis; KAFO, knee–ankle–foot orthosis; L, left; R, right.
*P<0.05, **P<0.01.
At admission, the median SIAS hip, knee, and foot scores in the AFO group were 3, 3, and 2.5, respectively, and the median LE touch and position scores were 2. These scores indicated that the AFO was applied in patients who could flex the paretic hip, extend the paretic knee, and dorsiflex the paretic ankle. All patients in the AFO group had intact sensory function for light touch and position sense. Patients in the KAFO group had median SIAS hip, knee, and foot scores of 1, 1, and 0, respectively, and median LE touch and position sense scores of 1. These scores indicated that patients wearing KAFOs could not perform hip flexion, knee extension, or foot taps. Muscle contractions were palpable in the iliopsoas and quadriceps femoris but were not palpable in the tibialis anterior. Sensory function in KAFO patients was impaired, as shown by both the light touch and position sense scores.
Gait Function and the Type of OrthosisTable 2 shows the changes in FAC scores in the AFO and KAFO groups between admission and discharge. FAC scores in both the AFO and KAFO groups significantly improved. Thirty-two patients (84.2%) in the AFO group and 20 patients (25.3%) in the KAFO group had an FAC score ≥3 at discharge. The SIAS LE motor score, SIAS LE sensory score, BBS, FIM motor, and FIM cognition scores significantly improved between admission and discharge in both the AFO and KAFO groups.
| AFO | KAFO | |||||
| Admission | Discharge | P value | Admission | Discharge | P value | |
| FAC | 1.58±0.72 (2, 0–3) | 3.50±1.13 (4, 1–5) | 0.007** | 0.44±0.68 (0, 0–2) | 1.77±1.28 (1, 0–5) | <0.001** |
| SIAS | ||||||
| Hip | 2.76±1.30 (3, 0–5) | 3.26±1.11 (3, 1–5) | <0.001** | 1.43±1.55 (1, 0–5) | 2.16±1.54 (2, 0–5) | <0.001** |
| Knee | 2.55±1.37 (3, 0–5) | 3.26±1.16 (3, 1–5) | <0.001** | 1.48±1.61 (1, 0–5) | 2.19±1.58 (2, 0–5) | <0.001** |
| Foot | 2.18±1.61 (2.5, 0–5) | 2.66±1.48 (3, 0–5) | <0.001** | 1.25±1.67 (0, 0–5) | 1.75±1.77 (1, 0–5) | <0.001** |
| L/E touch | 2.05±0.84 (2, 0–3) | 2.26±0.72 (2, 1–3) | <0.001** | 1.25±0.95 (1, 0–3) | 1.58±1.02 (1, 0–3) | <0.001** |
| L/E position | 1.79±0.94 (2, 0–3) | 2.16±0.82 (2, 0–3) | 0.003** | 1.08±1.01 (1, 0–3) | 1.38±1.14 (1, 0–3) | <0.001** |
| BBS | 21.39±14.19 (22, 0–56) | 42.29±13.25 (46.5, 0–56) | 0.013* | 4.85±7.51 (2, 0–37) | 16.49±17.78 (7, 0–56) | <0.001** |
| FIM | ||||||
| Motor | 43.76±13.68 (43, 23–70) | 69.68±17.91 (77, 14–91) | <0.001** | 24.66±12.73 (21, 13–55) | 40.81±23.37 (33, 13–90) | <0.001** |
| Cognitive | 22.11±7.14 (21.5, 10–35) | 26.71±7.40 (29, 9–35) | <0.001** | 13.67±7.22 (14, 5–32) | 18.19±9.14 (20, 5–35) | <0.001** |
Data are mean ± SD (median, range).
BBS, Berg balance scale; FAC, functional ambulation category; FIM, functional independence measure; L/E, lower extremity; SIAS, stroke impairment assessment set.
*P<0.05, **P<0.01.
Table 3 shows the results of stepwise multiple regression analysis; Figs. 1 and 2 show scatter plots of the actual and predicted FAC scores at discharge. The AFO dataset had a medium fit (R2=0.44), and analysis showed that the variables “age” and “FIM cognitive” could be used to predict the FAC score at discharge. Both “age” and “FIM cognitive” were statistically significant (P <0.05). Neither of these variables exhibited a high VIF (>10); consequently, we were able to conclude that there was no significant collinearity or multicollinearity between these variables.
| Estimate | Std. Error | t value | Pr (>|t|) | Coefficient | Standardized coefficient | 95% CI − Lower | 95% CI − Upper | |
| AFO | ||||||||
| (Intercept) | 4.245 | 0.961 | 4.416 | <0.001** | 4.245 | |||
| Age | –0.032 | 0.010 | –3.212 | 0.003** | –0.032 | –0.446 | –0.052 | –0.012 |
| FIM cognitive | 0.056 | 0.022 | 2.554 | 0.015* | 0.056 | 0.355 | 0.012 | 0.101 |
| KAFO | ||||||||
| (Intercept) | 2.868 | 0.620 | 4.627 | <0.001** | 2.868 | |||
| FIM cognitive | 0.050 | 0.016 | 3.083 | 0.003** | 0.050 | 0.284 | 0.018 | 0.083 |
| BBS | 0.067 | 0.015 | 4.434 | <0.001** | 0.067 | 0.394 | 0.037 | 0.098 |
| Age | –0.029 | 0.007 | –4.029 | <0.001** | –0.029 | –0.345 | –0.044 | –0.015 |
Estimate: The intercept and partial regression coefficient values calculated from the data.
Pr (>|t|): Significance probability for each test of intercept and partial regression coefficient.
95% CI − Lower: 95% confidence interval − lower limit.
95% CI − Upper: 95% confidence interval − upper limit.
*P<0.05, **P<0.01.
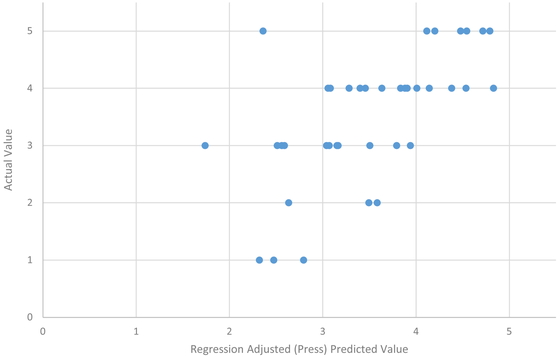
Scatter plot of the actual and predicted FAC scores at discharge in the AFO group.

Scatter plot of the actual and predicted FAC scores at discharge in the KAFO group.
The KAFO dataset also had a medium fit (R2=0.47), and analysis showed that the variables “FIM cognitive”, “BBS”, and “age” could be used to predict the FAC score at discharge. “FIM cognitive”, “BBS”, and “age” were statistically significant (P <0.05). None of these variables exhibited a high VIF (>10); consequently, we were able to conclude that there was no significant collinearity or multicollinearity among these variables.
This study revealed that patients who were fitted with KAFOs had more severe neurological impairment than patients using AFOs. Previous studies using the BRS as the motor function evaluation showed similar results. Maeshima et al. reported that the BRS was lower in the KAFO group than in the AFO group.3) Ota et al. reported that the KAFO group were older and had lower scores in all FIM items than did the AFO group.5,6) We used SIAS LE motor in which function is assessed on the paralyzed side by evaluating the hip joint, knee joint, and ankle joint. To our knowledge, this novel approach of conducting multifaceted analyses combining sensory function, balance function, and cognitive function has not previously been reported.
Indications for OrthosesKAFO is used to stabilize the knee securely during the weight-bearing phase of the gait cycle in patients with severe hemiparesis.11) More than half the patients using KAFOs in the current study could not flex the hip, extend the knee, or contract the tibialis anterior. These patients had impaired light touch and position sense, poor balance function, and poor cognitive function. In contrast, patients using AFOs had mild hemiparesis, intact sensory function, and good balance function. However, more than half the patients using AFOs could not fully dorsiflex the ankle. Therefore, AFOs were required for dorsiflexion during the swing phase of gait. Nikamp et al. reported that ankle kinematics and spatiotemporal parameters improved with the use of AFOs.4) Our study showed the conventional indications for AFOs and KAFOs based on median SIAS motor scores and sensory scores. At present, there are no clear criteria for selecting AFOs or KAFOs. This study aimed to determine the characteristics of patients who were prescribed AFOs or KAFOs in the clinical setting. The scores and physical characteristics that were identified showed the current applicability of these orthoses. These findings may help in selection of the most appropriate orthosis for gait rehabilitation. Further research is required to confirm our results, but our study findings can inform the design of future studies.
Gait Function Outcomes and OrthosesThis study showed that the AFO group had good outcomes regarding independent ambulation. In contrast, the KAFO group had a smaller proportion of patients with independent ambulation at discharge. In total, 32 of 38 patients (84.2%) in the AFO group and 20 of 79 patients (25.3%) in the KAFO group acquired ambulation without physical assistance in this study. A previous study reported similar rates of ambulation without physical assistance.12)
Based on our results, patients’ age and FIM cognitive scores could be used to predict the FAC score at discharge in the AFO group; moreover, age, FIM cognitive, and Berg Balance Scale scores could be used to predict the FAC score at discharge in the KAFO group. A previous study showed that balance control and cognitive function are important factors for predicting walking ability.13) Our study results suggest that balance control is an important factor for walking ability in severe hemiparesis. The use of KAFOs appears to be associated with good outcomes for independent ambulation in patients with severe hemiparesis demonstrating good balance control.
LimitationsAlthough the timing of the prescription for an orthosis in this study was generally within 1 week after admission, analysis using specific values was not performed. Therefore, we could not rule out the timing of the prescription as a contributing factor in our results. Moreover, analysis of various subtypes of AFOs is needed in the future.
The authors declare that there are no conflicts of interest.