2021 Volume 6 Article ID: 20210003
2021 Volume 6 Article ID: 20210003
Background: Surgical treatment of femoral neck fractures is usually performed as an urgent procedure so that restoration of the ability to stand and walk can be achieved as quickly as possible. However, orthopedic surgeons need to be aware of undertreated or untreated diseases in their patients. Organ transplant recipients require immunosuppressive agents and steroids postoperatively. Hemodialysis patients also exhibit immunological deterioration and are included among immunocompromised patients. We report a case in which conservative treatment was chosen for a hepatic transplant recipient on hemodialysis who suffered a femoral neck fracture because signs of inflammation of unknown etiology were intermittently seen.
Case: The patient was a 70-year-old man who had undergone liver transplantation from a living donor as treatment for hepatocellular cancer and hepatic failure with cirrhosis. Dialysis for end-stage renal failure was initiated at approximately 1 year postoperatively. Cyclosporine was administered as an immunosuppressive agent. The patient subsequently fell off a bicycle and was unable to walk because of right hip pain. He was brought to our hospital by ambulance, and a right hip radiograph revealed a femoral neck fracture. His white blood cell count and C-reactive protein levels were intermittently elevated with unknown etiology. Conservative treatment was finally adopted, although a bipolar hip arthroplasty was planned. At 5 months after the injury, the patient was able to walk alone in a stable manner using a pair of crutches and was discharged.
Discussion: Conservative treatment for a femoral neck fracture, which generally requires surgery, may be acceptable in organ transplant recipients on hemodialysis.
Femoral neck fracture, which is especially common in elderly patients, is an injury that negatively influences activities of daily living (ADL) and quality of life (QOL).1,2,3) Conservative treatment requires a long period of bed rest and causes complications such as dementia and aspiration pneumonitis that can sometimes lead directly or indirectly to patient death.1,3,4,5) Surgical treatment is usually performed as an urgent procedure because development of the above-mentioned complications can be prevented by restoring the ability to stand and walk as soon as possible.3,4,5,6) Elderly patients often have several diseases associated with mortality risk for surgery,1,3,5,7) and, because of these diseases, orthopedic surgeons need to be cautious when indicating surgical treatments.1,3,5)
According to The Japan Society for Transplantation, the numbers of organ transplantations are continuing to increase in Japan.8) Transplant recipients require immunosuppressive agents and steroids for the rest of their lives after surgery.9,10,11) As a consequence, their bones can become osteoporotic through use of steroids and the risk of fracture can be comparatively high, even for relatively young patients. The Japanese Society for Dialysis Therapy reported that the number of hemodialysis patients is also continuing to increase, as are the rates of older patients undergoing hemodialysis.12) Hemodialysis patients also exhibit immunological deterioration, and their bones can become osteoporotic through renal failure.11) Both organ transplant recipients and hemodialysis patients are included among immunocompromised patients with osteoporosis.13) Orthopedic surgeons should be cautious about intraoperative fractures and postoperative infections when they perform surgical treatments on organ transplant recipients or hemodialysis patients, even for relatively young patients.1,5) There are few reports of postoperative clinical outcomes of organ transplant recipients with orthopedic injuries and diseases, including femoral neck fractures, unlike the case for hemodialysis patients.14,15,16) Nevertheless, organ transplant recipients who suffer femoral neck fractures will become less rare in the near future because osteoporosis progresses with age. We report a case in which conservative treatment was chosen for a hepatic transplant recipient on hemodialysis who suffered a femoral neck fracture. Written informed consent was obtained from the patient and his wife for the reporting of this case, including the inclusion of photographs of the patient.
The patient was a 70-year-old man who underwent liver transplantation from a living donor for hepatocellular cancer and hepatic failure with cirrhosis. Dialysis for end-stage renal failure was initiated approximately 1 year postoperatively. Cyclosporine was administered as an immunosuppressive agent. Cholangitis occurred once after the transplantation. At 11 years after the transplantation, the patient fell off a bicycle and was unable to walk because of right hip pain. He was brought to our hospital by ambulance. A right hip radiograph revealed a femoral neck fracture classified as type 3 in the Garden classification, and the patient was admitted for surgical treatment to the Department of Orthopaedic Surgery (Fig. 1).

Radiograph of the hips at the time of the injury. An anteroposterior hip radiograph showed a right femoral neck fracture classified as type 3 according to the Garden classification. A bipolar hip arthroplasty was planned just after admission.
At 3 days after admission, the degree of systemic inflammation was determined to be severe on blood analysis, and surgery was postponed (Fig. 2). Consultations were undertaken with the Department of Digestive Surgery and the Department of Dialysis because cholangitis or infection related to dialysis was suspected. However, the reasons for the inflammation findings remained unclear. The patient’s temperature and C-reactive protein (CRP) levels were intermittently high (Fig. 2). Therefore, surgical treatment was rejected, although the patient complained about being unable to move and staying in bed because of right hip pain.
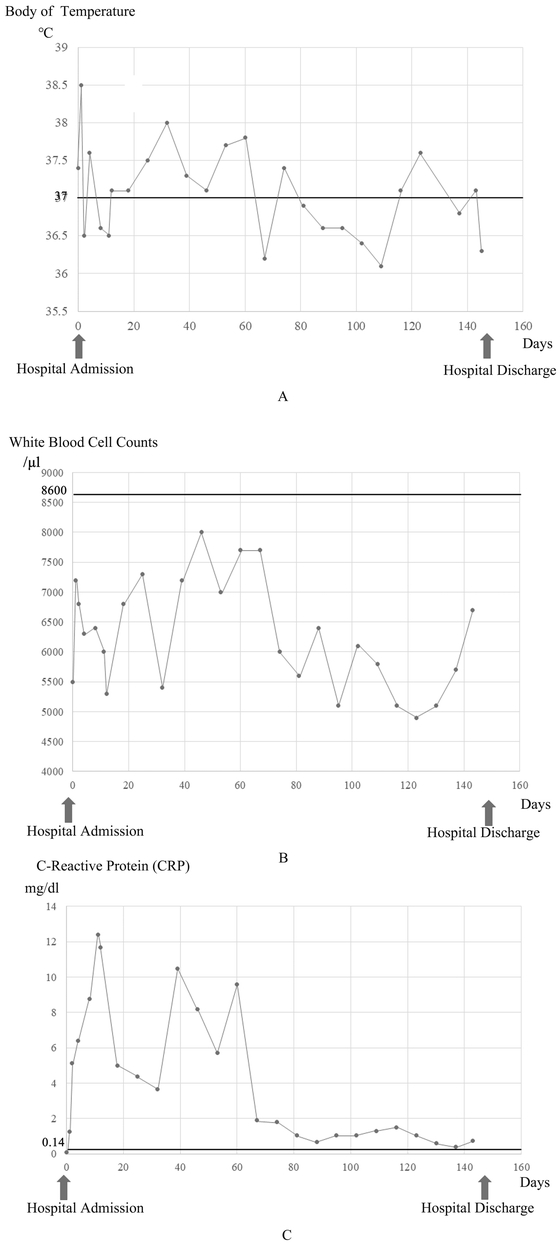
Time-dependent changes in body temperature and signs of inflammation. (A) Body temperature was intermittently higher than 37 °C and often exceeded 37.5 °C. (B) White blood cell counts were intermittently increased. The counts did not exceed 8600/μl, the upper limit of normal in the authors’ institution. (C) C-reactive protein levels were markedly increased. The levels did not decrease below 0.14 mg/dL, the upper limit of normal in the authors’ institution, but did decrease from about 2 months after the injury.
Rehabilitation was tentatively started to prevent complications including dementia and aspiration pneumonitis. Bone union was not expected because of the type of femoral neck fracture, and, if surgical treatment were to be performed, bipolar hip arthroplasty (BHA) was considered to be a better surgical procedure than osteosynthesis. Consequently, restrictions were not applied to the rehabilitation program to achieve the optimal condition in preparation for BHA at this time. Muscle strength exercises for the lower limbs were carried out with the patient on a bed and training for transfer to a wheelchair were mainly performed with acceptable pain levels. Gait training was impossible because of right hip pain. The right hip pain eventually decreased at 2 months after the injury. The signs of inflammation improved to some extent around the same time or slightly later. The patient then became able to turn and transfer to a wheelchair with some assistance. Surgical treatments were again considered. However, the patient’s temperature was sometimes raised. The unidentified fever and unexplained signs of inflammation together with the history of immunosuppressive agent and steroid use meant that surgical treatments were reluctantly abandoned. Measures to improve ADL without surgical treatments were duly selected. The goal was restoration of the ability to stand and walk using a pair of crutches or a walker with pseudoarthrosis in the right femoral neck. Gait training with a pair of crutches was initiated at about 3 months after the injury when the right hip pain had further decreased. The patient was able to walk on his own in a stable manner using a pair of crutches and was discharged at about 5 months after the injury (Fig. 3). He was consistently able to walk with a pair of crutches but used a wheelchair when covering more than a few hundred meters; however, bone union was not obtained in the right femoral neck, and mild right hip pain remained at 11 months after the injury (Fig. 4).

Photograph of the patient walking during rehabilitation. The patient was able to walk on his own using a pair of crutches at about 3 months after the injury.

Radiograph of the hips at 11 months after the injury. An anteroposterior hip radiograph showed that part of the right femoral neck fracture had not achieved bone union.
Environmental adjustments, including those to the patient’s home on the first floor of an apartment building, were not necessary, although he continued gait training at home by making use of a nursing-care service. The patient’s Barthel index was 85 points, and he was still self-sufficient at the final follow-up. The patient and his wife, who were satisfied with his ADL after discharge, desired surgical treatment for his right hip to improve his ADL. However, denial of surgery was the only option because signs of inflammation remained in occasionally positive findings, and cholangitis requiring readmission was diagnosed once at 3 years after the injury.
Femoral neck fracture is a common injury, especially in elderly patients, and it negatively influences patients’ ADL and QOL.3) The occurrence of fractures in the proximal femoral region will continue to increase.1,2,6,7,17) These growing numbers are associated with problems related to osteoporosis, especially among elderly patients.4,18) The long period of bed rest during conservative treatment can lead to walking disability, sarcopenia, frailty, and other complications.5) Surgical treatment, including osteosynthesis and BHA, is usually performed as an urgent procedure to prevent such complications.4,5,6) Preoperative blood analysis, plain chest radiography, cardiac electrograms, and echocardiography sometimes show aberrant finding and malfunctions that prolong the time until surgical treatments can be performed. These examinations can even preface the discovery of other diseases, such as diabetes mellitus, cardiac failure, and cancer. Therefore, although surgical treatment is strongly recommended, orthopedic surgeons sometimes encounter difficulties in making decisions to proceed with surgery for femoral neck fractures. Comparatively high mortality rates have been reported after conservative treatments.2,3,7) However, surgical procedures should be halted or suspended if the risk of lethal complications is high.3,5,7,18)
Organ transplantations provide benefits to patients with fatal diseases, although they need to take immunosuppressive agents and steroids for the rest of their lives.9) These medicines elevate the risks of infection and osteoporosis.14) Patients are often comparatively young at the time of organ transplantation. However, patients tend to become curious about these risks when they reach middle age or become elderly. The present patient had undergone liver transplantation and was also on hemodialysis. Therefore, his immunological deterioration and osteoporosis may have been comparatively severe. The cause of the inflammation could not be identified, although cholangitis or infection related to dialysis was suspected. However, certain complications did occur in this case. The signs of inflammation were intermittently positive, and the orthopedic surgeons were unable to decide when the operation should be performed. In particular, the risk of surgical site infection (SSI) was considered to be very high, given the organ transplantation, terminal renal failure with hemodialysis, and intermittent signs of inflammation. The risk was high because the artificial materials inserted into the body during BHA and other arthroplasties are generally sensitive to infections.19,20) Even caries of the teeth can cause SSI after an arthroplasty.19,20) Revision surgery for infection after primary total hip arthroplasty (THA) reportedly increases the mortality risk during the first year after the second procedure.21) The indications for arthroplasty require discretion regarding the high risk of SSI, and appropriate preventive and treatment measures are also needed.21,22) In the current patient, an SSI would be unlikely to respond to treatment and would likely prove fatal. The implications of his condition was explained to the patient and his wife several times. After some amount of confusion and hesitation, they ultimately agreed with the decision not to undergo surgical treatments for the femoral neck fracture because his ADL gradually improved as his right hip pain decreased. BHA may be reconsidered to improve the patient’s ADL in the future if the signs of inflammation remain low. However, BHA requires caution because these signs have not yet become stabilized and have recurred.
There are some limitations to this case report. Bone mineral density and bone metabolism were not evaluated in this patient. Activated vitamin D had been administered. Necessary examinations and other effective treatments for osteoporosis should be considered.
BHA was selected as the optimal surgical procedure in this case. Osteosynthesis as another option for surgical treatment was little discussed. Femoral neck fractures are associated with difficulties in bone union. Non-dislocated fractures, which have the risk of becoming dislocated fractures and often necessitate osteosynthesis procedures, require extreme care to prevent dislocation of the fracture parts during conservative treatment.23,24,25) Even dislocated femoral neck fractures are considered for osteosynthesis procedures using screws with the goal of joint conservation without the demerits of BHA or THA, such as dislocation and ultimately component loosening, when patients are young or active older adults.6) Because the CRP levels remained critically high at about 60 days after admission in the current patient, all surgical procedures were considered to be high risk, especially with the risk of SSI. Furthermore, it may have been too late to perform osteosynthesis for femoral neck fracture by about 60 days after the injury. A previous case report described a patient with a non-dislocated femoral neck fracture who achieved bone union and became able to walk after 4 weeks of bed rest.2) Another case report described a patient with a dislocated femoral neck fracture who did not obtain bone union but was able to walk after 3 weeks of bed rest led to decreased pain.18) However, conservative treatment is realistic in older patients with a femoral neck fracture and severe underlying diseases like the present patient.
Because of fever of unknown cause and unexplained signs of inflammation, conservative treatment was chosen for a case involving a femoral neck fracture in a liver transplant recipient on hemodialysis. The patient was able to walk on his own in a stable manner using a pair of crutches at about 5 months after the injury. He was consistently able to walk with a pair of crutches but used a wheelchair when travelling more than a few hundred meters; bone union was not achieved at 11 months after the injury. Conservative treatment for a femoral neck fracture may be acceptable when organ transplant recipients on hemodialysis suffer medical problems like those in the present case.
The authors thank Alison Sherwin, PhD, from Edanz Group (https://en-author-services.edanzediting.com/ac) for editing a draft of this manuscript.
The authors certify that there are no conflicts of interest with any financial organizations regarding the material discussed in the manuscript.