2021 年 6 巻 論文ID: 20210008
2021 年 6 巻 論文ID: 20210008
Objectives: We aimed to identify the quadriceps muscle strength (QMS) thresholds below which exercise capacity is compromised in men with chronic obstructive pulmonary disease (COPD).
Methods: We measured the quadriceps isometric maximum voluntary contraction (QMVC) and calculated the QMVC values normalized to weight (QMVC-BW), height squared (QMVC-H2), and body mass index (QMVC-BMI) in 113 patients with COPD. The functional exercise capacity was evaluated using the 6-minute walk distance (6MWD), and 6MWD <350 m was defined as functional exercise intolerance. Thresholds were determined for QMVC and its normalized values to achieve high specificity (>0.90) with maximal sensitivity. P-values <0.01 were considered statistically significant.
Results: Data from 99 male patients (age, 74 ± 6 years; percentages of predicted forced expiratory volume in 1-s, 56.9 ± 26.4%) were analyzed; 3 women and 11 participants with the missing data were excluded. Multivariate logistic regression models identified significant associations of QMVC and QMVC-H2 with 6MWD, after adjustment for age and dyspnea. C-statistics showed that the area under the curves of all QMVC parameters were comparable. The thresholds of QMVC and QMVC-H2 for predicting compromised exercise capacity were 26.2 kg and 9.6 kg/m2, respectively.
Conclusions: QMS thresholds in men with COPD could help clinicians evaluate whether QMS is insufficient to achieve 6MWD ≥350 m and thereby identify patients who should be specifically targeted for muscle strengthening training during their pulmonary rehabilitation program.
Quadriceps muscle weakness is an important extrapulmonary manifestation of COPD1) and is observed in approximately one-third of patients with stable COPD.2) Robust evidence points toward the adverse effects of quadriceps muscle weakness on exercise capacity,3) chair-stand ability,4) and survival1) in COPD patients. Therefore, muscle strength training is a key component of,5) and muscle strength is an important outcome of,6) pulmonary rehabilitation in patients with COPD.
Two thresholds of quadriceps isometric maximum voluntary contraction (QMVC), measured as a marker of quadriceps muscle strength (QMS), have been established in COPD.1,4) First, QMS ≤120%, which is the ratio of QMVC to body mass index (BMI), can predict mortality in patients with COPD.1) Second, QMVC normalized to the square of the body height (men: ≤8.30 kg/m2, women: ≤5.99 kg/m2) can distinguish patients with COPD who are able to rise from a chair from those who cannot.4) However, no threshold has been established for identifying exercise intolerance, as evaluated by the 6-minute walk distance (6MWD), in patients with COPD.
The 6MWD is an important outcome for functional exercise capacity in COPD and better reflects the patient’s functional exercise level for daily physical activities than does lung function.7,8) Reductions in 6MWD have also been associated with increased risk of mortality7,9) and exacerbation-related hospitalization9) in COPD. A 6MWD <350 m is an established cut point for predicting mortality in patients with COPD.7) Because of associations between reduced 6MWD and adverse outcomes in COPD, determinants of poor 6MWD should be identified. To date, pulmonary function, dyspnea, and psychological factors have been identified as significant determinants of poor 6MWD (<350 m).10) This previous study,10) however, did not measure QMS, which is moderately to strongly associated with 6MWD2) and gait performance11,12) in COPD patients. Consequently, associations of QMS and poor 6MWD should be investigated in COPD patients. Furthermore, the relationship between muscle strength and walking performance is nonlinear in healthy adults13) and the elderly population.14) A threshold of QMVC below which 6MWD is compromised should be determined for COPD.
Although the 6-minute walk test (6WMT) is well established for investigating exercise capacity in COPD patients, it is not often used in the clinical setting because it requires time, space, and resources.15) Many patients are not able to undergo assessment of their exercise capacity, and this situation may lead to exercise intolerance being overlooked (e.g., 6MWD <350 m), despite exercise intolerance being a risk marker of mortality. Consequently, an easy-to-conduct screening method for exercise intolerance is required to identify the need for further exercise capacity assessment in a setting where the 6MWT cannot be used routinely. A threshold of QMVC that can predict poor 6MWD could be used as such a screening approach, thereby avoiding the need to perform the 6MWT.
Against this background, we aimed to determine the thresholds for QMVC and for associated values normalized by anthropometric parameters below which 6MWD is compromised in patients with COPD; the predictive capabilities of these thresholds were compared. Defining a threshold for QMVC may enable clinicians to evaluate whether QMS is insufficient to achieve 6MWD ≥350 m without performing the 6MWT. This approach would be useful for targeting patients for muscle strength training during pulmonary rehabilitation programs and could be used as a screening tool for poor 6MWD in patients with COPD.
This retrospective cross-sectional study included 113 outpatients with COPD who were referred to the outpatient pulmonary rehabilitation unit of Akita City Hospital between April 2013 and December 2017. All participants met the following inclusion criteria: a diagnosis of COPD in accordance with international guidelines16); a stable condition with no infection or exacerbation of COPD for at least the previous 3 months; and the absence of severe and/or unstable cardiac disease, orthopedic disease, or mental disorder.
We obtained the results of QMS measurements, the 6MWT, pulmonary function tests, and a questionnaire that collectively formed the baseline assessments for the outpatient pulmonary rehabilitation program. Pulmonary function tests were performed by well-trained laboratory medical technologists, and well-trained physical therapists performed the other measurements. This study was reviewed and approved by the Medical Ethics Committee of Akita City Hospital (2018, approval No. 61) and was conducted in compliance with the Declaration of Helsinki. Informed consent was waived because the study was retrospective in nature. We used bulletin boards in our hospital as an opt-out method to provide opportunities for participants to decline participation in this study.
Quadriceps Muscle Strength MeasurementQMVC was measured with a Hydromusculator GT-160 (OG Giken, Okayama, Japan) to evaluate QMS in accordance with the technique described by Seymour et al.2) Participants were positioned in the standard fashion (seated with knees and hips flexed at 90°) and their hip joints and thighs were fixed with belts to ensure that they remained seated. QMVC was defined as the highest mean force that could be sustained for longer than 1 s. Measurements were carried out at least three times. A 30- to 60-s rest period was permitted between contractions to allow participant recovery. The highest measured force was recorded as the participant’s QMVC. This value was normalized according to weight (QMVC-BW), the square of the height (QMVC-H2), and BMI (QMVC-BMI), to adjust for body composition.
Six-minute Walk Distance MeasurementThe 6MWD was measured as an indicator of functional exercise capacity. Participants performed the 6MWT in accordance with the European Respiratory Society (ERS)/American Thoracic Society (ATS) technical standard.17) The examiners encouraged participants continuously using two phrases, i.e., “You are doing well” or “Keep up the good work.” Participants were allowed to stop and rest during the test but were instructed to resume walking as soon as they could. Participants did not practice the 6MWT, and all participants underwent a single test. Participants were asked to take all usual medications but did not inhale a short-acting bronchodilator just before undertaking the 6WMT. Participants who were using long-term oxygen therapy inhaled oxygen during the test. In this study, 350 m was defined as the threshold of reduced 6MWD.7)
Other VariablesThe forced expiratory volume in 1-s (FEV1), a measure of pulmonary function, was evaluated using a spirometer (CHESTGRAPH HI-701, Chest MI, Tokyo, Japan). Pulmonary function tests were performed with inhalation of bronchodilators. FEV1 values were expressed as percentages of the predicted values, as reported by Berglund et al.18) Airflow obstruction was evaluated using the Global Initiative for Chronic Obstructive Lung Disease classification of severity of airflow obstruction (GOLD stage).16) Modified Medical Research Council dyspnea scores (MMRC) were obtained as markers of the degree of dyspnea.19)
Statistical AnalysisP-values less than 0.01 were considered statistically significant. All participants were divided into two groups based on their 6MWD, i.e., 6MWD <350 m and 6MWD ≥350 m. The assumption of normality was assessed using the Shapiro-Wilk test. Group differences were assessed using the independent-samples t-test for continuous variables, the Mann-Whitney U-test for nonparametric and discrete variables, and the Chi-squared test for nominal scales.
The relationships between QMVC, QMVC-BW, QMVC-H2, and QMVC-BMI and 6MWD were determined using multivariate logistic regression analysis. Each analysis included the classification of 6MWD according to the threshold (350 m) as a dependent variable, along with one QMS outcome as an independent variable. Age and MMRC were also included in all models to adjust for age and degree of dyspnea. Akaike’s information criterion (AIC) and the adjusted root mean squared error (RMSE) calculated by the tenfold cross-validation method were used to compare the four models.
The abilities of QMVC, QMVC-BW, QMVC-H2, and QMVC-BMI to predict poor 6MWD (<350 m) were evaluated using the C-statistic [area under the curve (AUC)] of the logistic model. Differences among the AUCs of the four QMVC parameters were compared. Thresholds were determined from the point on the receiver operating characteristics curve with high specificity (>0.9) and the highest sensitivity. There were two reasons why we selected this point as a threshold of QMVC. First, 6WMD <350 m is not a serious life-threatening condition. Second, we aimed to estimate a minimal threshold below which 6WMD was compromised. In other words, most patients would be able to walk less than 350 m during the 6MWT (disease positive) if their QMVC was less than the threshold (test positive).
The required total sample size was estimated using Buderer’s method20) for sensitivity and specificity analysis with an α of 0.05, a power of 0.80, a marginal error of 0.15, a predetermined sensitivity of 0.69,4) a predetermined specificity of 0.69,4) and a predetermined prevalence of poor 6MWD of 0.41.10) The calculated total sample sizes for sensitivity and specificity analyses were 89.1 and 61.9, respectively. Therefore, the minimum sample size was set at 90 participants. Statistical analyses were performed with IBM SPSS Statistics 21.0 (IBM Corporation, Armonk, NY, USA) and R (version 3.6.1).
The three women among the 113 potential subjects were excluded from analysis because the number of female participants with COPD was very low, and muscle strength is lower in women than in men.21) Eleven other participants were excluded from analysis because of missing data. Finally, 99 male participants with COPD were included in the analysis. The Shapiro-Wilk test showed that all continuous variables were distributed normally (P≥0.01). The characteristics of the participants are presented in Table 1.
| All (n=99) | 6MWD ≥350 m (n=69) | 6MWD <350 m (n=30) | Mean difference (99%CI) | P Value | |
| Age, years | 74 (6) | 73 (6) | 78 (6) | 5 (2, 9) | <0.001 |
| Body height, cm | 163.8 (5.7) | 164.7 (5.6) | 161.8 (5.6) | –3.9 (–6.1, 0.5) | 0.025 |
| Body weight, kg | 56.6 (9.3) | 58.6 (9.1) | 52.0 (8.0) | –6.6 (–11.5, –1.8) | <0.001 |
| BMI, kg/m2 | 21.1 (3.2) | 21.6 (3.1) | 19.9 (3.2) | –1.7 (–3.6, 0.1) | 0.014 |
| FVC, L | 3.05 (0.81) | 3.23 (0.77) | 2.64 (0.74) | –0.59 (–1.03, –0.15) | <0.001 |
| FEV1, L | 1.38 (0.65) | 1.51 (0.62) | 1.08 (0.62) | –0.43 (–0.79, –0.07) | 0.002 |
| FEV1, % predicted | 56.9 (26.4) | 61.2 (24.8) | 47.2 (27.6) | –13.0 (–21.9, 2.6) | 0.040 |
| GOLD stage, I/II/III/IV | 13/35/32/19 | 4/23/27/15 | 9/12/5/4 | N.A. | 0.003 |
| LTOT, n (%) | 9 (9) | 3 (4) | 6 (20) | N.A. | 0.013 |
| MMRC | 2 (1, 3) | 2 (1, 2) | 3 (2, 3) | N.A. | <0.001 |
| 6MWD, m | 411 (161) | 501 (75) | 203 (102) | –298 (–354, –242) | <0.001 |
| QMVC, kg | 34.6 (11.4) | 38.8 (10.2) | 25.0 (7.8) | –13.8 (–18.7, –8.7) | <0.001 |
| QMVC-BW | 0.61 (0.18) | 0.66 (0.17) | 0.49 (0.16) | –0.17 (–0.27, –0.08) | <0.001 |
| QMVC-H2, kg/m2 | 12.8 (4.1) | 14.3 (3.6) | 9.6 (2.9) | –4.7 (–6.6, –2.9) | <0.001 |
| QMVC-BMI, kg/(kg/m2) | 1.65 (0.52) | 1.81 (0.48) | 1.28 (0.43) | –0.53 (–0.79, –0.27) | <0.001 |
Data are mean (SD) or median (25th, 75th percentile) except where otherwise indicated.
6MWD, 6-minute walk distance; BMI, body mass index; FVC, forced vital capacity; FEV1, forced expiratory volume in 1-s; GOLD, Global Initiative for Chronic Obstructive Lung Disease classification of severity of airflow obstruction; LTOT, long-term oxygen therapy; MMRC, modified Medical Research Council dyspnea score; QMVC, quadriceps isometric maximum voluntary contraction; BW, body weight; H2, body height squared.
Table 2 summarizes the results of multivariate logistic regression analyses. QMVC and QMVC-H2 were significantly associated with 6WMD after adjusting for age and MMRC. The AICs for QMVC and QMVC-H2 were lower than those for QMVC-BW and QMVC-BMI. The adjusted RMSEs calculated using the tenfold cross-validation method were similar among the four models.
| Variables | Coefficient | Odds ratio | 99%CI | P value | AIC | Adjusted RMSE |
| QMVC, kg | –0.15 | 0.86 | 0.77, 0.97 | 0.001 | 78.0 | 0.31 |
| QMVC-BW | –4.74 | 0.01 | 0.00, 1.51 | 0.018 | 85.7 | 0.29 |
| QMVC-H2, kg/m2 | –0.38 | 0.68 | 0.50, 0.93 | 0.002 | 78.4 | 0.30 |
| QMVC-BMI, kg/(kg/m2) | –1.84 | 0.14 | 0.02, 1.11 | 0.015 | 85.4 | 0.30 |
The dependent variable was 6MWD (6MWD <350 m or 6MWD ≥350 m). Age and modified Medical Research Council dyspnea score were also included as independent predictors in all regression analyses for covariate adjustment.
The adjusted RMSE for each regression model was calculated using the tenfold cross-validation method.
Coefficient (β), partial regression coefficient; 99%CI, 99% confidence interval; AIC, Akaike’s information criterion; RMSE, root mean squared error.
The thresholds and predictive abilities of QMVC, QMVC-BW, QMVC-H2, and QMVC-BMI below which 6MWD is compromised (<350 m) are presented in Table 3 and Fig. 1 The AUCs of QMVC and QMVC-H2 tended to be higher than those of QMVC-BW and QMVC-BMI, but the differences were not statistically significant (P=0.033) (Fig. 2). The positive predictive values for QMVC-BW and QMVC-BMI tended to be higher than those for QMVC and QMVC-H2, whereas the negative predictive values of the four parameters were comparable. The positive likelihood ratios of the four parameters were moderate to large, whereas the negative likelihood ratios of the four parameters were low.22)
| Variable | 6MWD <350 m | |||||||
| Threshold | AUC (99%CI) | Sensitivity | Specificity | PPV | NPV | PLR | NLR | |
| QMVC, kg | 26.2 | 0.86 (0.76, 0.95) | 0.57 | 0.91 | 0.74 | 0.83 | 6.33 | 0.47 |
| QMVC-BW | 0.44 | 0.76 (0.63, 0.90) | 0.50 | 0.96 | 0.83 | 0.81 | 12.50 | 0.52 |
| QMVC-H2, kg/m2 | 9.6 | 0.85 (0.75, 0.95) | 0.50 | 0.91 | 0.71 | 0.81 | 5.56 | 0.55 |
| QMVC-BMI, kg/(kg/m2) | 1.20 | 0.78 (0.65, 0.91) | 0.50 | 0.94 | 0.79 | 0.81 | 8.33 | 0.53 |
AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value; PLR, positive likelihood ratio; NLR, negative likelihood ratio.

Scatter plots showing the relationships between the 6-minute walk distance (6MWD) and quadriceps muscle strength (QMS). The horizontal axes are (a) the quadriceps isometric maximum voluntary contraction (QMVC), (b) QMVC normalized to body weight (QMVC-BW), (c) QMVC normalized to body height squared (QMVC-H2), and (d) QMVC normalized to body mass index (QMVC-BMI). The vertical axes show 6MWD. Horizontal dashed lines show 6MWD=350 m, and vertical dashed lines show the QMS thresholds. i.e., (a) QMVC=26.4 kg, (b) QMVC-BW=0.44, (c) QMVC-H2=9.6 kg/m2, and (d) QMVC-BMI=1.20 kg/(kg/m2). Patients were located in one of the following quadrants: 1, preserved 6WMD (>= 350 m) and poor QMS [QMVC <26.2 kg, QMVC-BW <0.44, QMVC-H2 <9.6 kg/m2, or QMVC-BMI <1.20 kg/(kg/m2)]; 2, preserved 6MWD and preserved QMS; 3, poor 6MWD and poor QMS; 4, poor 6WMD and preserved QMS.
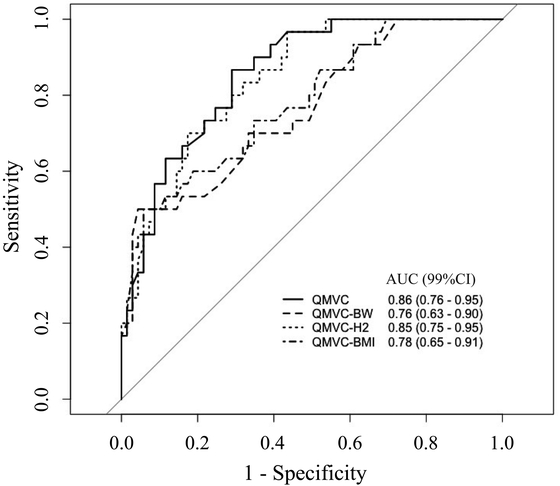
Receiver operating characteristic curve (ROC) and areas under the curve (AUC) of quadriceps muscle strength measures. This figure represents ROC and AUC for quadriceps isometric maximum voluntary contraction (QMVC) (solid line), QMVC normalized to body weight (QMVC-BW) (dashed line), QMVC normalized to body height squared (QMVC-H2) (dotted line), and QMVC normalized to body mass index (QMVC-BMI) (dot-dash line).
We have demonstrated QMS thresholds below which 6MWD was compromised in male patients with COPD. Although 6MWD in COPD is affected by both physical and psychological factors,10) QMVC thresholds may help clinicians to evaluate whether a patient’s QMS is insufficient to achieve a preserved 6MWD (≥350 m) and to identify patients who should be targeted for muscle strength training during pulmonary rehabilitation.
Characteristics of the Participants in This StudyIn the present study, participants who walked less than 350 m during the 6MWT were older and thinner than those who could walk 350 m or more. Participants with a poor 6MWD had more severe airflow limitation, a greater degree of dyspnea, and lower QMVC than those with an adequate 6MWD. A systematic review of the properties of the 6MWT for COPD showed that age, weight, severity of airflow obstruction, and degree of dyspnea were associated with 6MWD.23) QMS was shown to be positively correlated with functional exercise tolerance, as evaluated by 6MWD, in patients with COPD.24) Muscle weakness reportedly contributed to exercise intolerance in patients with chronic respiratory diseases.3) Furthermore, the participants’ mean QMVC-BW (0.61) was lower than that of age-matched healthy elderly Japanese men (>0.80).21) Participants in our study had the standard characteristics of patients with COPD.
Associations Between Quadriceps Muscle Strength and Functional Exercise CapacityThe current study showed that QMVC and QMVC-H2 were significant predictors of poor 6MWD, even after adjusting for age and MMRC in patients with COPD. Gosselink et al. found that QMVC was an independent predictor of 6MWD after adjusting for similar variables including age and body composition.24) This can be explained by the following structural changes in lower limb muscles known to occur in patients with COPD: muscle atrophy, weakness, shift in fiber type, poor oxidative capacity, and mitochondrial dysfunction.25) Weakness of the quadriceps muscle is proportional to muscle atrophy in most patients with COPD.24) Furthermore, earlier studies revealed that reduction in muscle strength, muscle mass, and muscle endurance might occur simultaneously in individuals with COPD.26,27) These changes in lower limb muscles may result in increased leg effort during exercise,3) the principal symptom limiting exercise capacity in approximately 40% of individuals with COPD.28) Therefore, it is not surprising that QMVC parameters were independently associated with poor 6MWD, after adjusting for possible confounders in the current study.
Interpretation of Quadriceps Muscle Strength ThresholdsThis is the first study to investigate QMS thresholds below which 6MWD is compromised in patients with COPD. The QMVC thresholds established in the current study were higher than those in the study by Canavan et al.4) This can be explained by the fact that Canavan et al. used chair-stand ability (whether a participant was able to stand from a chair) as their dependent variable,4) whereas we used walking ability (whether 6MWD was less than 350 m) as our dependent variable. The inherent difficulty of walking is greater than that of standing from a seated position. Consequently, different thresholds were observed in our study and in that of Canavan et al. Interestingly, the threshold of QMVC-BMI in the study by Swallow et al.1) was similar to that of the current study. A possible explanation is that 6MWD <350 m is an established threshold for predicting mortality in patients with COPD,7) and Swallow et al. used mortality as their dependent variable.1) Therefore, similar thresholds of QMVC-BMI were obtained in both studies.
In the current study, the following thresholds [QMVC of 26.2 kg, QMVC-BW of 0.44, QMVC-H2 of 9.6 kg/m2, and QMVC-BMI of 1.20 kg/(kg/m2)] resulted in moderate to large positive likelihood ratios (5.56–12.5). This indicates that a patient with a QMS less than these thresholds (test positive) is approximately five to twelve times more likely to exhibit 6MWD <350 m (disease positive). In other words, when the test is positive, the post-test probability of 6MWD <350 m is approximately 90% according to a nomogram22) and the pretest probability of 6WMD <350 m (41%).10) Therefore, these values could be used as thresholds of QMS below which exercise capacity is compromised in men with COPD. Moreover, in a setting where the 6MWT is not conducted routinely, QMS thresholds could be used as a screening method for exercise intolerance in COPD. In other words, a positive test result indicates the need for further assessment of exercise capacity.
Implementation of Quadriceps Muscle Strength Thresholds in Clinical PracticeIn the current study, the predictive capabilities of the four QMVC parameters were comparable. These results suggest that QMVC and its ratios to anthropometric parameters could be used as QMS thresholds in patients with COPD. QMVC is a simple concept that is easily understood by patients. Consequently, normalization of QMVC to anthropometric parameters may not be necessary. From the clinical perspective, these thresholds can be used to evaluate whether QMS is insufficient to walk >350 m during the 6MWT and thereby identify patients who should be targeted for muscle strength training during pulmonary rehabilitation. For example, if a patient is classified as being in quadrant 3 (Fig. 1), both exercise capacity and QMS have deteriorated. Muscle strength training should be prioritized in these patients rather than other interventions such as aerobic training or breathing exercise. However, if a patient is classified as being in quadrant 4 (Fig. 1), exercise capacity is poor but QMS is preserved. Such patients should be targeted for other interventions (e.g., aerobic training or breathing exercise) rather than muscle strengthening training, because other factors (e.g., pulmonary function or dyspnea) may limit his/her exercise capacity. If QMVC or QMVC-H2 is less than the threshold, while the other is more than the threshold, we consider that the patient should be treated as if his/her QMS is insufficient and should undergo muscle strength training for the following reasons. First, if one test is positive (QMVC <26.2 kg or QMVC-H2 <9.6 kg/m2), the post-test probability of 6MWD <350 m is approximately 90%, as discussed above. Second, these thresholds were aimed at finding potential patients who should be targeted for muscle strength training. A single positive test result, even if the other test is negative, indicates that the patient’s QMS may be insufficient to achieve preserved 6MWD. As a result, we recommend that such patients should be targeted for muscle strength training. These thresholds, therefore, can allow clinicians to evaluate the need for muscle strength training for their patients and ensure the development of personalized pulmonary rehabilitation programs for patients with COPD.
LimitationsSome limitations should be considered while interpreting our results. First, measurement and confounding biases may have influenced the results of this retrospective study. However, all measurements of QMS and 6MWD were performed by well-trained specialists, in accordance with standardized methods.2,17) Possible confounders, such as cognitive function and comorbidities, were controlled by excluding patients with dementia and other severe and/or unstable comorbidities. Therefore, we suggest that these biases might not have limited the significance of our findings. Second, because of the small number of women with COPD in Japan, this study included only men. Whether the results of this study can be applied to women with COPD should be tested by future research. Third, 6MWT was performed only once in this study. Ideally, two 6MWTs should be performed to minimize the learning effect on 6MWD. However, the ERS/ATS technical standard states that two 6MWTs should be considered, but one test may be sufficient for assessing risk (e.g., likelihood of hospitalization or mortality).17) Consequently, the 6MWD obtained in this study could be used as a dependent variable for C-statistics. Fourth, the external validity of QMS thresholds should be investigated using another cohort. Finally, we did not assess the skeletal muscle mass. Although it would be ideal to measure both muscle strength and muscle mass, muscle strength is a better predictor of adverse outcomes than is muscle mass in older adults.29) A recent European consensus on sarcopenia defined muscle strength, instead of muscle mass, as a primary criterion of the diagnosis of sarcopenia.29) Therefore, we believe that the utility of the QMVC threshold is retained.
Summary and ConclusionsIn summary, we demonstrated significant thresholds of QMVC and its value normalized using patient height squared below which 6MWD is compromised in patients with COPD. Consequently, a QMVC of 26.2 kg and a QMVC-H2 of 9.6 kg/m2 could be used as QMS thresholds. These thresholds allow clinicians to identify patients who should be targeted for muscle strength training and can be used to develop personalized pulmonary rehabilitation programs. These thresholds can also be used as a screening tool to assess the need of further evaluation of exercise capacity in patients with COPD.
The authors are grateful to the members of the rehabilitation staff at Akita City Hospital for their assistance with data collection. We would like to thank Editage (http://www.editage.com) for editing and reviewing this manuscript for English language usage.
The authors have no competing interests to declare.