2021 Volume 6 Article ID: 20210033
2021 Volume 6 Article ID: 20210033
Objectives : An important role of convalescent rehabilitation wards is the short-term improvement of mobility and activities of daily living (ADL). We aimed to identify predictors associated with the length of stay (LOS) in a convalescent hospital after total hip and knee arthroplasty.
Methods : This study included 308 patients hospitalized in a convalescent ward following total hip or total knee arthroplasty. The following factors were examined: age, sex, orthopedic comorbidities, motor component of the functional independence measure (M-FIM), M-FIM gain, pain, 10-m walk test, timed up and go (TUG) test, functional ambulation category (FAC), cognitive function, and nutritional status. LOS was categorized as shorter (≤40 days) or longer (>40 days), based on the national average LOS in a convalescent ward, and was statistically analyzed with predictor variables.
Results : In our hospital, the average LOS was 36.9 ± 21.4 days, and the average M-FIM at admission to the convalescent ward and the M-FIM gain were 71.1 ± 7.0 and 16.3 ± 6.9, respectively. In univariate analysis, there was a significant correlation between LOS and M-FIM at admission and M-FIM gain, pain, TUG time, and FAC. Logistic multivariate analysis identified M-FIM at admission (odds ratio [OR] 0.93, 95% confidence interval [CI] 0.88–0.98) and TUG time (OR 1.10, 95% CI 1.03–1.18) as independent predictors of LOS.
Conclusions : The M-FIM and TUG test can be used to accurately estimate LOS and to plan rehabilitation treatment in a convalescent rehabilitation ward after lower-limb arthroplasty. Furthermore, preoperative or early postoperative intervention may lead to better quality motor activity and shorter LOS during the convalescent period.
The current aging of the population has a substantial impact on public health, and one area of focus is the difference between total life expectancy and healthy life expectancy.1) According to a basic survey about the lives of citizens in Japan, bone fractures/falls and joint disease, respectively, accounted for 12.5% and 10.8% of all factors resulting in the need for nursing care.2) Musculoskeletal disorders are one of the main reasons for needing nursing care, and these disorders can directly affect mobility and activities of daily living (ADL); therefore, rehabilitation treatment that includes a convalescent period is crucial for patients with these disorders. The convalescent rehabilitation system was set up in Japan in 2000 with the goal of improving post-incident ADL of affected patients and increasing their likelihood of being discharged home through rehabilitation care.3) Convalescent rehabilitation also plays an especially important role in the recovery of physical function and ADL for patients following lower-limb arthroplasty, leading to a shorter length of stay (LOS) and an increased home discharge rate.4,5,6) According to a survey by the Kaifukuki Rehabilitation Ward Association, the proportion of lower-limb arthroplasties among all inpatients was 6.5%, and the average LOS was 40.6 days.7)
Osteoarthritis is considered to be the most prevalent chronic joint disease and is one of the most common sources of pain and disability in the elderly. Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are the two major surgeries for patients with end-stage osteoarthrosis. Surgery and its postoperative rehabilitation are causally linked to the improvement of pain and the recovery of physical function. Insufficient recovery of mobility function is a strong predictor of prolonged LOS.8) Identifying the preoperative and early postoperative factors that affect future functional abilities would be especially useful for planning rehabilitation treatment and accurately predicting LOS. For patients after THA or TKA, previous studies of prolonged LOS have identified associations with older age, female sex, increased comorbidity, high-intensity pain, reduced strength of the quadriceps femoris muscle, reduced dynamic balance, higher body mass index (BMI), malnutrition, and a lower mental score.9,10,11,12) However, to our knowledge, factors associated with LOS in a convalescent rehabilitation ward for patients following hip and knee arthroplasty have been minimally discussed in the literature.
The aim of the present study was to determine the factors influencing LOS in a convalescent hospital for patients after total hip or knee arthroplasty.
This study retrospectively analyzed patients following THA and TKA who were admitted to the convalescent ward of our hospital between April 2017 and March 2020. Included were patients with hip and knee osteoarthritis who underwent primary unilateral total arthroplasty at a single acute care hospital. In the acute care hospital, THA and TKA were performed using consistent surgical procedures and clinical paths for perioperative management and standardized rehabilitation until patients were discharged to our hospital. Full weight bearing was allowed immediately after surgery. Exclusion criteria were the development of severe postoperative complications or adverse events including infection, periprosthetic fractures, and dislocation of total hip joint. We also excluded patients who were transferred to other hospitals to receive integrated treatment for comorbid conditions. Consequently, five patients were excluded, and a total of 308 patients (187 with THA, 121 with TKA) were enrolled in the present study. Following the admission assessments, a multidisciplinary team established rehabilitation goals and a treatment plan, including muscle strength, range of motion of the operated joint, gait, and ADL training. All patients participated in their individualized occupational and physiotherapy treatment at least twice per day for 1 h each time. This was a retrospective cohort study performed at the Fukuoka Mirai Hospital in Fukuoka, Japan. Because of the retrospective nature of the study, an opt-out procedure for recruitment was instituted that allowed patients to withdraw from the study at any time. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Fukuoka Mirai Hospital Ethics Review Board (approval number: 202104–2).
Length of StayThe LOS was defined as the number of calendar days between admission to the convalescent ward of our hospital and hospital discharge. In this study, our discharge criterion for THA and TKA patients was the ability to perform a series of daily activities independently at home, e.g., bathing, stair climbing, and walking outdoors. Patients were divided into two groups, namely those with shorter (≤40 days) and longer (>40 days) LOS; the cutoff of 40 days was determined based on the average LOS in patients following lower-limb arthroplasty reported in a survey by the Kaifukuki Rehabilitation Ward Association.7)
Outcome MeasuresThe medical records of the included patients were reviewed for age, sex, the presence of comorbidity, ADL, the extent of pain, physical and cognitive function, and nutritional status. We also examined general comorbidity using the Charlson Comorbidity Index13) and the presence of other orthopedic comorbidities,14) including lower-limb osteoarthritis on the contralateral side. ADL were evaluated using the motor component of the functional independence measure (M-FIM) at both admission and discharge. The effectiveness of rehabilitation between admission and discharge was assessed by the improvement in the M-FIM (i.e., [M-FIM score at discharge] – [M-FIM score at admission]).15) Pain intensity was measured at admission using a numerical rating scale (NRS).16) Muscle strength was assessed as the isometric knee extension force measured with a hand-held dynamometer17) on both the affected and unaffected sides and the grip power.18,19) Furthermore, gait and mobility function were evaluated using the 10-m walk test, the timed up and go (TUG) test,20,21) and the functional ambulation category (FAC).22) Cognitive functions were assessed using the mini-mental state examination and the Hasegawa dementia rating scale–revised. The nutritional status was evaluated using the BMI, arm circumference (AC), triceps skinfold (TSF), arm muscle circumference (AMC), and calf circumference (CC). The average of the left and right values was used for measurements of grip power, TUG time, AC, TSF, AMC, and CC. All these assessments were carried out within a few days after admission.
Statistical AnalysisDescriptive data are presented as the mean plus/minus the standard deviation or the number and percentage. The significance of differences between two groups was statistically analyzed using unpaired t tests for continuous parametric data and Chi-squared tests for categorical variables. Variables with a P value of <0.2 in the univariate analysis and those associated with admission assessment only were used in the logistic regression model. Multiple logistic regression analysis was used to determine predictors associated with prolonged LOS in patients after lower-limb arthroplasty. Results were presented as odds ratios (OR) with 95% confidence intervals (CI). The receiver operating characteristic (ROC) curve was generated, and the area under the curve (AUC) was calculated to assess the diagnostic value and accuracy of different parameters as predictive factors for differentiating shorter and longer LOS. Statistical analyses were performed using JMP version 15.0 (SAS Institute Inc., Cary, NC, USA). A P value of less than 0.05 was considered statistically significant.
Demographic data, average LOS, M-FIM at admission, and M-FIM gain are listed in Table 1. The average age at the time of admission to the convalescent ward was 71.2 ± 9.2 years. All patients in this series were discharged directly to home from the convalescent ward. The average number of postoperative days (POD) spent in the acute care hospital was 18.2 ± 4.2 days, and the average LOS in our convalescent ward was 36.8 ± 21.4 days. The average LOS at our hospital was slightly shorter than the national average. The average M-FIM score at admission was 71.1 ± 7.0 points, which was higher than the national average. The average M-FIM gain was almost the same as the national average.
| National data | Our single-center data | |
| Number of cases | 2718/year | 308/3 years |
| Age (years) | 74.4 ± 9.9 | 71.2 ± 9.2 |
| Sex (male:female) | 19:81 | 22:281 |
| POD in acute care hospital (days) | 16.6 ± 9.1 | 18.2 ± 4.2 |
| LOS in convalescent hospital (days) | 40.6 ± 23.1 | 36.8 ± 21.4 |
| M-FIM score at admission (score, 13–91) | 63.5 ± 15.3 | 71.1 ± 7.0 |
| M-FIM gain (score, 0–78) | 18.5 ± 12.5 | 16.3 ± 6.9 |
The characteristics of patients in the shorter and longer LOS groups are shown in Table 2. The shorter LOS group contained 207 patients and had an average LOS of 24.3 ± 8.8 days, whereas the longer LOS group included 101 patients, and had an average LOS of 62.6 ± 15.7 days. A lower M-FIM score at admission (P <0.01), a higher M-FIM gain (P <0.01), a higher pain intensity as assessed by NRS (P <0.01), a longer TUG time (P <0.01), and a lower FAC score (P <0.01) were significantly related to prolonged LOS. Comparing patient characteristics following THA to those following TKA, patients with THA were significantly younger (THA: 68.8 ± 9.6 years, TKA: 74.8 ± 7.1 years, P <0.01), had a lower pain score (THA: 3.4 ± 2.3 points, TKA: 5.8 ± 2.3 points, P <0.01), and had a greater extension strength in the affected knee (THA: 145.5 ± 66.6 kgf/kg, TKA: 85.5 ± 46.8 kgf/kg, P <0.01) than those with TKA. There were no statistically significant differences regarding other clinical factors between those undergoing THA and those undergoing TKA.
| Shorter LOS | Longer LOS | P value | |
| (n=207) | (n=101) | ||
| Age (years) | 70.6 ± 8.5 | 72.5 ± 10.3 | 0.11 |
| Female | 192 (92.8) | 89 (88.1) | 0.18 |
| Charlson Comorbidity Index (score, 0–37) | 0.8 ± 1.1 | 0.9 ± 0.9 | 0.81 |
| The presence of orthopedic comorbidity | 88 (42.5) | 53 (49.1) | 0.10 |
| POD in acute care hospital (days) | 18.1 ± 3.8 | 18.4 ± 5.0 | 0.61 |
| LOS in convalescent hospital (days) | 24.3 ± 8.8 | 62.6 ± 15.7 | <0.01* |
| M-FIM score on admission (score, 13–91) | 72.6 ± 5.8 | 68.1 ± 8.3 | <0.01* |
| M-FIM gain (score, 0–78) | 14.9 ± 6.1 | 18.8 ± 7.7 | <0.01* |
| Pain (numerical rating scale) (score, 0–10) | 4.0 ± 2.5 | 4.9 ± 2.7 | <0.01* |
| Knee extension force/affected side (kgf) | 124.5 ± 66.1 | 114.8 ± 67.3 | 0.42 |
| Knee extension force/unaffected side (kgf/kg) | 180.1 ± 75.5 | 167.0 ± 71.3 | 0.33 |
| Grip strength (kg) | 19.0 ± 6.5 | 18.6 ± 7.3 | 0.69 |
| 10-m walk test (s) | 10.1 ± 5.8 | 13.8 ± 17.7 | 0.06 |
| Timed up and go test (s) | 13.0 ± 4.6 | 17.0 ± 8.3 | <0.01* |
| Functional ambulation categories (score, 0–5) | 3.35 ± 1.2 | 2.44 ± 1.5 | <0.01* |
| Mini-mental state examination (score, 0–30) | 27.4 ± 3.5 | 27.2 ± 3.1 | 0.61 |
| Hasegawa dementia rating scale–revised (score, 0–30) | 27.4 ± 3.7 | 27.2 ± 3.1 | 0.77 |
| Body mass index (kg/m2) | 24.7 ± 3.8 | 24.5 ± 4.3 | 0.67 |
| Arm circumference (cm) | 26.6 ± 3.7 | 26.6 ± 3.8 | 0.89 |
| Triceps skinfold (cm) | 1.61 ± 0.8 | 1.54 ± 0.9 | 0.51 |
| Mid-upper arm muscle circumference (cm) | 21.5 ± 3.2 | 21.7 ± 3.3 | 0.59 |
| Calf circumference (cm) | 32.4 ± 3.9 | 32.7 ± 3.4 | 0.55 |
*Statistically significant
In multivariate logistic regression, prolonged LOS was independently associated with the M-FIM score at admission (OR 0.93, 95% CI 0.88–0.98) and TUG test time at admission (OR 1.10, 95% CI 1.03–1.18) (Table 3).
| Univariate analysis | Multivariate analysis | ||
| P value | OR (95% CI) | P value | |
| Age | 0.11 | 1.00 (0.97–1.04) | 0.72 |
| Female | 0.18 | 2.96 (0.91–9.65) | 0.07 |
| Orthopedic comorbidity | 0.1 | 1.37 (0.73–2.58) | 0.32 |
| M-FIM score at admission | <0.01* | 0.93 (0.88–0.98) | <0.01* |
| Pain (numerical rating scale) | <0.01* | 1.13 (0.99–1.28) | 0.06 |
| 10-m walk test | 0.06 | 0.95 (0.90–1.02) | 0.14 |
| Timed up and go test | <0.01* | 1.10 (1.03–1.18) | <0.01* |
| Functional ambulation category | <0.01* | 0.84 (0.64–1.11) | 0.22 |
OR, odds ratio; 95% CI, 95% confidence interval.
*Statistically significant.
We identified the cutoff points for the M-FIM score and the TUG time using ROC curves. Our results revealed that M-FIM scores differentiated patients with a longer LOS at a threshold of 68 points (AUC: 0.67, 95% CI: 0.58−0.73, P <0.05), whereas TUG differentiated patients with a longer LOS at a threshold time of 13.7 s (AUC: 0.66, 95% CI: 0.60−0.73, P <0.05). Figure 1 shows the ROC curve results.
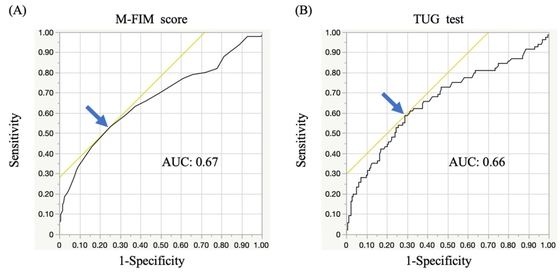
Receiver operating characteristic (ROC) curves for the M-FIM score (A) and the TUG time (B) on admission to the convalescent rehabilitation ward. Arrows indicate the best cutoff values. (A) The M-FIM score. Area under the ROC curve: 0.67 (95% CI: 0.58−0.73); 53.4% sensitivity and 74.9% specificity for a cutoff of 68 points. (B) The TUG test. Area under the ROC curve: 0.66 (95% CI: 0.60−0.73); 58.8% sensitivity and 70.1% specificity for a cutoff of 13.7 s.
The aim of this study was to identify determinants influencing the LOS at a convalescent rehabilitation hospital following THA or TKA at an acute care hospital. Our main results showed that prolonged LOS in the convalescent rehabilitation ward was independently associated with the M-FIM score and the TUG time at admission, suggesting that these assessment tools may be useful for accurately predicting LOS and thereby improving the planning of care. Furthermore, better physical function on admission to the convalescent ward is likely to be important for reducing LOS.
The purpose of intensive rehabilitation in a convalescent ward is to increase the recovery of mobility and the rate of discharge to home. Convalescent rehabilitation also has an important role for patients following total lower-limb arthroplasty, because it results in shorter LOS and the reduction of medical costs. In our study, the average LOS in the convalescent ward was 36.8 days, which was slightly shorter than the national average LOS (40.6 days) in a survey of patients after lower-limb arthroplasty.7) This result could be explained by the less severe postoperative complications and the reduced level of other adverse events in our study. Moreover, the higher M-FIM score at admission compared with national data seemed to have an effect on shortening LOS. The improvement in the ADL score during hospitalization at our institution was in line with the national average.
THA and TKA represent two of the most common procedures used to alleviate pain resulting from degenerative diseases and to improve ADL and quality of life. Apart from avoiding serious adverse events, the main objective following hospital discharge after lower-limb arthroplasty is to ensure that the patient achieves postoperative functional improvement to be able to perform basic ADL. Previous reports have demonstrated that preoperative and early postoperative M-FIM scores were associated with LOS.23,24) A previous study demonstrated that, in patients following revision THA, lower M-FIM scores indicated lower functional motor capacity and more dependence in basic functional activities, resulting in prolonged LOS.23) Another report suggested that physical activities assessed by motor performance tests at admission to the rehabilitation facility were important predictors of LOS in patients following lower-limb arthroplasty.24) These results indicated that better quality motor activity before convalescent rehabilitation could result in reduced LOS following THA and TKA, which was consistent with our results. Considering these results together, preoperative and early postoperative rehabilitation for patients undergoing THA and TKA seemed to be important for accelerating functional recovery and reducing LOS.25,26,27)
The TUG test is a comprehensive motor ability assessment that includes functional mobility, dynamic balance, and walking ability.20,21,28) Several studies have demonstrated that preoperative and early postoperative TUG times are useful for predicting both short- and long-term mobility function following lower-limb arthroplasty.29,30) In patients after THA, one previous study suggested that the TUG test in the early stage was an effective indicator to predict ambulation ability at 6 months after surgery.31) Poitras et al. reported that the preoperative and postoperative day 2 TUG time could indicate hospital LOS and short-term functional capacity.32) In the current study, the TUG test was performed on admission to our convalescent ward, which usually occurred about 2–3 weeks after surgery, which was consistent with previous studies. The TUG test, which requires several complex movements, seems to reflect the performance of ADL for discharge to home better than other simple measurements such as muscle strength or balance. These findings suggest that the TUG test may be a good predictor of short-term function during hospitalization after lower-limb arthroplasty.
Even in patients without complications, poorly controlled pain is a major reason that hospital stays tend to be longer than expected. Inadequately managed pain negatively affects functional recovery, increases the risk of postsurgical complications, and may lead to persistent postsurgical pain in patients following THA or TKA. As a result, early postoperative physical therapy is hindered by pain, and LOS is prolonged.16,33) Therefore, postoperative interventions for pain control are important, and several strategies for pain management with various modalities have been suggested for patients following lower-limb arthroplasty.34,35) Pain control using multimodal medications in the acute care hospital setting during the early postoperative period seems to reduce pain intensity on admission to the convalescent ward. In this study, the pain score at admission had no association with LOS, and these results could be explained by the effect of pain relief during acute care hospitalization. These findings suggest that pain control during the early postoperative period following arthroplasty tends to lead to the earlier recovery of function and reduction in LOS following lower-limb arthroplasty.
The present study has several limitations. First, we did not investigate the impact on LOS of patient-related factors such as psychiatric factors, socioeconomic status, and living environment. In particular, patient motivation and the desire to participate in the rehabilitation process are closely associated with clinical outcomes and LOS;36) however, these data were not included in this study. Second, we could not describe predictors of LOS in the THA and TKA patient groups separately. Although separate data may provide useful information on how these relationships differ between the two groups of patients, we could not find national data on LOS in the convalescent hospital for each group. It seemed infeasible to accurately identify predictors of LOS without the availability of the national average data for each group. Moreover, there were some differences in the baseline characteristics between the two groups, and these could have affected the clinical outcomes. Consequently, we assessed only predictors for the total group of patients who underwent THA and TKA in this study. Third, no basic preoperative information about physical function, for example, could be obtained from the acute care hospital. Such data are important because preoperative physical activity levels and ADL influence postoperative mobility and LOS. Therefore, future studies are warranted to evaluate predictors for prolonged LOS for THA and TKA separately and to identify other factors related to LOS.
In conclusion, the current study investigated predictors that may influence LOS at a convalescent hospital for patients following THA or TKA. This study identified poor results on M-FIM and the TUG test at admission to the convalescent ward as significant predictors of prolonged LOS. These predictive factors can be used for planning rehabilitation treatment and accurately predicting LOS. Furthermore, our results indicate that preoperative and early postoperative intervention by collaborating with the acute care hospital may lead to higher motor functional activity and decreased LOS at the convalescent hospital.
The authors are grateful to the members of the rehabilitation staff at Fukuoka Mirai Hospital for their assistance with data collection. This study did not receive any grant funding.
The authors have no conflicts of interest directly relevant to the content of this article.