2021 Volume 6 Article ID: 20210046
2021 Volume 6 Article ID: 20210046
Objective: The objectives of this study were to investigate whether student athletes with anterior cruciate ligament (ACL) injuries who returned to sports (RTS) without reconstruction could continue their sporting activities until the end of the season and whether there was an increase in secondary damage associated with knee instability.
Methods: Altogether, 288 skeletally mature patients aged <25 years with new-onset isolated primary ACL injuries were included. Of these, 20 student athletes continued playing sports without ACL reconstruction to try to finish the season and were classified as the early return to sports (ERS) group; the remaining 268 patients, who immediately quit sports and underwent surgery, were classified as the non-ERS group. Knee symptoms and sporting performance for the rest of the season were assessed for the ERS group. The presence of secondary damage, e.g., meniscus injuries and chondral lesions, associated with instability were compared between the two groups.
Results: Fourteen ERS-group athletes (70%) indicated that their knees had given way during sporting activities, and seven athletes (35%) were unable to complete the season. In the ERS group, the mean self-estimated performance level after injury was 3.8 ± 2.5 (numeric rating scale 0–10). Despite the RTS period being relatively short, medial meniscus tears (P <0.001) significantly increased in the ERS group, and three patients experienced locking of the medial meniscus and required immediate surgery.
Conclusions: Although ERS without reconstruction to complete the season may be a reasonable strategy for ACL injury, patients’ self-estimated performance level was low and meniscal and cartilage injury rates significantly increased.
Anterior cruciate ligament (ACL) injury is a relatively common knee injury, particularly among young student athletes.1) Because the ACL is one of the most important knee stabilizers, it is difficult for most athletes to participate in pivoting sports without ACL reconstruction (ACLR). Multiple studies have reported that delayed reconstruction after ACL injury increases meniscus and cartilage injury rates.2,3,4,5,6,7,8,9,10) Furthermore, delayed ACLR is considered a risk factor for subsequent meniscal surgery.11) Early ACLR prevents future meniscus tears and cartilage injuries and may reduce consequent osteoarthritis.12,13) Therefore, the standard treatment for ACL injury is reconstruction in conjunction with a recommendation to temporarily suspend sports activity until after ACLR.14) However, a few athletes, commonly referred to as “copers”,15) reportedly resume their prior levels of activity without dynamic instability after ACL rupture.
ACLR has several disadvantages, including graft site morbidity, long post-surgical rehabilitation period, and high repeat injury rate.16) Returning to sports too early involves an increased risk of repeat injury; a recent study has recommended delaying returning to sport for at least 9 months after ACLR.17) Although careful management is recommended after ACLR, a recent systemic review reported that 63.4% of athletes returned to pre-injury level of sports, and the average time to return to sport (RTS) after reconstruction surgery was 17.2 months.18) Because RTS is difficult within the same season after ACLR, athletes, especially student athletes, may wish to continue playing until the end of the season prior to surgery.19) It remains unclear how these student athletes achieve successful RTS without ACLR and to what degree secondary injury could occur during the short remaining season. There have been several reports demonstrating the efficacy of conservative therapy for ACL injuries.20,21) Moreover, in some cases, surgeons may consider granting permission to continue sporting activities to student athletes who are eager to RTS until the end of the season immediately after ACL injury, despite the patient knowing the risks involved.
The objectives of this study were to investigate whether student athletes who RTS without ACLR were able to continue their sporting activities until the end of the season and whether the rate of secondary damage associated with knee instability increased during this period. We hypothesized that, without ACLR, student athletes would not be able to achieve RTS at a satisfactory level and would suffer a higher rate of secondary injury.
This retrospective study was approved by the Ethics Committee of Hirosaki University (#2011–251), and all patients provided written informed consent. Between January 2013 and December 2018, 658 patients underwent ACLR at our institution. The inclusion criteria for the current study were student athletes, age <25 years, and a history of arthroscopic primary ACLR; consequently, 414 patients were included. The exclusion criteria were as follows: multiple knee ligament injury other than ACL injury combined with grade 1 medial collateral ligament injury (n=13); revision ACL surgery (n=90); history of knee surgery and combined surgery, such as high tibial osteotomy or medial patellofemoral ligament reconstruction (n=4); patients with open physis (n=5); and RTS without diagnosis or delayed diagnosis of ACL injury and unclear injury date (n=14) (Fig. 1).
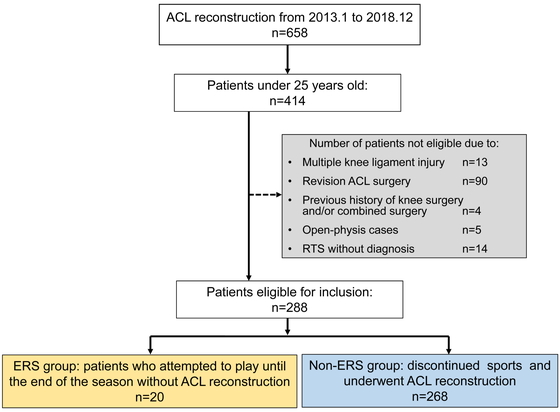
Participant selection process. Of the 414 subjects aged less than 25 years who underwent anterior cruciate ligament reconstruction, 288 were included in this study. Of these, 20 patients decided to return to sport to try to complete the season.
In total, 288 patients (183 female and 105 male) were included in this study, with a mean age of 17.6 ± 2.8 years. Although all patients were advised to stop sporting activities and undergo ACLR, some desired to return to competitive sports until the end of the season without undergoing surgery. Although we comprehensively explained the possibility of the knee “giving way” and secondary injury resulting from knee instability, some athletes still decided to RTS to finish the season. These athletes made up the early RTS without surgery (ERS) group (n=20). Those who immediately quit sports and underwent immediate or elective ACLR were classified as the non-ERS group (n=268) (Fig. 1).
All patients in the ERS group wore an ACL knee brace and underwent athletic rehabilitation. The rehabilitation program was performed under the supervision of a physical therapist. Physical therapy was performed in seven steps: range of motion exercises, isometric muscle-strengthening exercises, full weight-bearing and closed kinetic chain exercises, running, open kinetic chain exercises, jump-landing training, and sports-specific training. However, athletes in the ERS group decided on their own whether to participate in sporting activities, as the remaining time in the season was limited.
Status and Satisfaction Relating to Early Return to SportsThe questionnaire survey items for the ERS group included the following: the time between injury and RTS, whether sporting activities were continued until the end of the season, the period for which sports activity was continued (from RTS to the end of the season or quitting sports), experience of knee giving way, and catching or locking episodes during sports activity.15) A numerical rating scale (NRS) was used to assess the self-estimated satisfaction score with the decision to RTS without surgery (10: completely satisfied, 0: completely dissatisfied), and the sports performance level (10: same as pre-injury level, 0: impossible to participate in the game).
Evaluation of Meniscus Tears and Cartilage InjuriesInitial magnetic resonance imaging (MRI) results after ACL injury were analyzed by radiologists who were unaware of the treatment options chosen by the patients. Medial meniscus (MM) and lateral meniscus (LM) injuries found on the initial MRI were defined as radiological meniscus injuries and were compared between the ERS and non-ERS groups. All arthroscopic ACLRs were performed or directly supervised by the senior author (Y.I.). Meniscus injuries found during ACLR were defined as definitive meniscal injuries and were compared between the groups. Meniscal injuries included both complete and partial thickness tears as well as ramp lesions. Articular cartilage injuries were assessed by arthroscopy according to the International Cartilage Repair Society (ICRS) system. The locations of the lesions were classified as follows: patellar, trochlear, medial femoral condyle, medial tibial plateau, lateral femoral condyle, or lateral tibial plateau.
Statistical AnalysisTo achieve 80% statistical power with an alpha of 0.05, power analysis indicated that a minimum of 12 patients in the ERS group and 157 patients in the non-ERS group would be required to detect any differences in the prevalence of concomitant injuries using the chi-square test. Post hoc power analysis showed that the actual power of the current analysis was 0.953, with an alpha of 0.05.
Demographic data are shown as means and standard deviations. According to the Shapiro–Wilk test, none of the parameters were normally distributed. Consequently, age, body mass index, time between injury and MRI, time between injury and ACLR, and Tegner activity scale scores were compared between the ERS and non-ERS groups using the Mann-Whitney U test. Additionally, the prevalences of radiographic meniscus injury, definitive meniscus injury, and definitive cartilage injury were compared using the chi-square test or Fisher’s exact test. Data input and analyses were performed using SPSS version 27.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was set at P <0.05.
The ERS group comprised 14 female and 6 male patients (17.0±2.8 years), and the non-ERS group comprised 169 female and 99 male patients (17.7 ± 2.8 years). All athletes in the ERS group participated in competitive sports at the prefectural level or above. In contrast, most of the athletes in the non-ERS group competed at the prefectural level, but some were active only in recreational sports. There was no significant difference in the Tegner activity scores between the two groups. Moreover, there was no significant difference between the two groups in the number of days between injury and diagnostic MRI (Table 1). The period between injury and ACLR was significantly longer in the ERS group (162.8 ± 87.6 days) than in the non-ERS group (47.1 ± 37.7 days, P <0.001). The most common activity when acquiring ACL injury was playing basketball (Table 2).
| ERS group n=20 | Non-ERS group n=268 | P-value | |
| Age | 17.0 ± 2.8 | 17.7 ± 2.8 | 0.310 |
| Female/male | 14/6 | 169/99 | 0.534 |
| BMI | 23.9 ± 3.0 | 23.7 ± 3.8 | 0.542 |
| Perioda to MRI (days) | 8.1 ± 9.7 | 7.7 ± 14.2 | 0.419 |
| Periodb to ACLR (days) | 162.8 ± 87.6 | 47.1 ± 37.7 | <0.001 |
| Tegner activity score | 7.0 ± 0.6 | 6.9 ± 1.3 | 0.803 |
ERS, early return to sports, BMI, body mass index. MRI, magnetic resonance imaging, ACLR, anterior cruciate ligament reconstruction.
aDays from injury to first MRI taken for diagnosis.
bDays from injury to ACLR.
| Sports activity | ERS group n=20 | Non-ERS group n=268 |
| Basketball | 10 (50%) | 104 (38.8%) |
| Skiing | 2 (10%) | 36 (13.4%) |
| Soccer | 3 (15%) | 27 (10.1%) |
| Volleyball | 1 (5%) | 28 (10.4%) |
| Judo | 1 (5%) | 17 (6.3%) |
| Gymnastics | 1 (5%) | 13 (4.9%) |
| Rugby, American football | 0 (0%) | 11 (4.1%) |
| Track and field | 1 (5%) | 8 (3.0%) |
| Badminton | 0 (0%) | 8 (3.0%) |
| Baseball | 1 (5%) | 5 (1.9%) |
| Other sportsa | 0 (0%) | 6 (2.2%) |
| Other traumab | 0 (0%) | 5 (1.9%) |
aHandball, tennis, or dance.
bFalls or traffic accidents.
The average period until RTS after injury in the ERS group was 24.5 ± 23.4 (9–112) days (Table 3). Although 13 of the 20 ERS athletes continued their sporting activities until the end of the season, the remaining 7 athletes quit sports and underwent ACLR because of knee instability or MM locking. The mean period for which sports activity was continued was 79.0 ± 52.9 (14–210) days. Fourteen athletes (70%) experienced their knee “giving way” during sports activity, and seven athletes (35%) experienced catching or locking episodes. Of these, three athletes experienced MM locking; consequently, immediate MM repairs combined with ACLR were performed. The average satisfaction score was 6.5 ± 2.9 (range 1–10), and the average performance level after injury was 3.8 ± 2.5 (range 2–8).
| ERS group n=20 | |
| RTS after injury (days) | 24.5 ± 23.4 |
| Sports continuation to end of season | 65% (13/20) |
| Sport continuation period (days) | 79.0 ± 52.9 |
| Awareness of knee giving way | 70% (14/20) |
| Awareness of knee catching or locking | 35% (7/20) |
| Sports performance level | 3.8 ± 2.5 (2–8) |
| Satisfaction score | 6.5 ± 2.9 (1–10) |
The prevalence of radiological MM injury, as detected on initial MRI, was 25.0% and 23.1% in the ERS and non-ERS groups, respectively (P=0.789) (Table 4). The prevalence of radiographic LM injury was 35.0% and 46.3% (P=0.329), respectively. The prevalence of definitive MM in the ERS and non-ERS groups was 65.0% and 26.1%, respectively, whereas for definitive LM injuries, the prevalences were 40.0% and 57.8%, respectively. The prevalence of definitive MM injury in the ERS group was significantly higher than that in the non-ERS group (P<0.001). Articular cartilage injury was found in 30% and 15.3% of the patients in the ERS and non-ERS groups, respectively (P=0.086), and no grade IV lesions were detected. Most cartilage lesions were located on the medial femoral condyle in both groups, and the prevalence of medial femoral condyle injury in the ERS group was significantly higher than that in the non-ERS group (P=0.021).
| ERS group n=20 | Non-ERS group n=268 | P-value | |
| Radiological meniscus injury | |||
| Medial meniscus | 5 (25.0%) | 62 (23.1%) | 0.789 |
| Lateral meniscus | 7 (35.0%) | 124 (46.3%) | 0.329 |
| Definitive meniscus injury | |||
| Medial meniscus | 13 (65.0%) | 70 (26.1%) | <0.001 |
| Lateral meniscus | 8 (40.0%) | 155 (57.8%) | 0.121 |
| Definitive cartilage injury | |||
| Total number of patients | 6 (30.0%) | 41 (15.3%) | 0.086 |
| MFC | 6 (30.0%) | 32 (11.9%) | 0.021 |
| MTP | 0 (0.0%) | 3 (1.1%) | 1.000 |
| LFC | 1 (5.0%) | 5 (1.9%) | 0.353 |
| LTP | 0 (0.0%) | 1 (0.4%) | 1.000 |
| Patella | 0 (0.0%) | 7 (2.6%) | 1.000 |
| Trochlea | 0 (0.0%) | 0 (0.0%) | 1.000 |
MFC, medial femoral condyle, MTP, medial tibial plateau, LFC, lateral femoral condyle, LTP, lateral tibial plateau.
In the present study, the primary finding was that the performance level of young ACL-injured athletes who continued playing for the rest of the season without ACLR was relatively low. Although the athletes in the RTS group did not regret their decision, their performance level was significantly lower (3.8 ± 2.5) than they expected, and 35% of the RTS athletes could not continue their sporting activities until the end of the season. Despite the relatively short periods that RTS athletes were engaged in sporting activities, MM tears and cartilage lesions of the medial femoral condyle significantly increased in the ERS group. Furthermore, MM locking occurred in three patients (15%) and resulted in the discontinuation of sports activity and immediate surgery.
In the current study, 6.9% of patients under 25 years of age attempted to return to competitive sports without ACLR. The satisfaction scale score of 6.5 for the decision was low, even though the average time from injury to RTS was much shorter than that for the usual protocol after ACLR. During sporting activities, most players experienced pain, “giving way”, and catching of the injured knee. Only six members (30%) of the RTS group did not experience their knee “giving way” during a game, and self-estimated performance levels were less than half of the pre-injury levels. Furthermore, two athletes who did not experience their knee “giving way” experienced MM locking and discontinued sporting activities during the season. For athletes returning to sporting activities after conservative treatment of ACL injury, Takata reported a conscious performance score of 58.4%, and 90.5% of players experienced their knee “giving way” during participation in sport.19) As suggested in that study, conservative treatment of athletes with ACL injuries should be carefully assessed taking these findings into account. Baez et al. reported that injury-related fear was associated with RTS and physical activity levels after ACLR.22) Hartigan et al. reported that kinesiophobia before surgery was lower in potential copers than in non-copers, but kinesiophobia before surgery was higher than that after surgery in both groups.23) Although we did not investigate psychological factors, psychological evaluations should be conducted in future studies.
The “rule of thirds” implies that one-third of patients with an ACL injury compensate well without ACLR (copers), one-third adapt by modifying their activities (adapters), and the remaining one-third require ACLR (non-copers).24) Thoma et al. reported that after 6 months of progressive neuromuscular and strength training, the proportion of potential copers increased.15) Although progressive rehabilitation might improve performance levels, patients in the ERS group did not have enough time for rehabilitation to take effect within the same season. A longer period of progressive rehabilitation might improve the performance and satisfaction scale scores reported in the current study.
Several previous studies reported that delaying ACLR increases MM tears and cartilage lesions, but does not increase LM tears.2,3,5.9) Although our results indicated similar outcomes in student athletes, more severe damage was detected because of continued engagement in competitive sports. This result was also consistent with a report by Anderson et al. that sporting activity and experience of knees giving way more than twice were risk factors for secondary injuries.2) At our institution, we routinely endeavor to conduct ACLR early; the mean time to ACLR from injury was 47.1 days in the non-ERS group. Therefore, rates of medial meniscus tears and cartilage lesions were relatively low compared with those reported in previous studies.2,3,4,5,6,7,8,9,10) Because early ACLR might reduce secondary MM and cartilage injury, clinical guidelines for ACL injuries recommend ACLR within 3–6 months of injury.12) Moreover, early surgical intervention also reduces the risk of subsequent meniscal surgery after ACLR.11)
LM tears are predominantly observed in acute ACL injury.25,26) In the current study, LM tears did not increase in the ERS group, compared with the non-ERS group, similar to the findings of previous studies.2,3,5,9) Shelbourne and Heinrich reported good long-term outcomes of ACLR without LM repair or resection.27) However, recent biomechanical and clinical studies have demonstrated the importance of LM repair in reducing anterolateral instability after ACLR.28,29,30) Therefore, unstable LM tears should be repaired to improve ACLR outcomes. Everhart et al. reported that the risk of high-grade medial chondral damage increased if the period between injury and ACLR was greater than 5 months.3) In the current study, the majority of cartilage damage occurred in the medial femoral condyle in both the ERS and non-ERS groups, and cartilage damage was more frequently detected in the ERS group than in the non-ERS group. Typical MRI findings for ACL injuries include bone marrow edema on the lateral femoral condyle. Just as for meniscus injuries, lateral femoral condyle lesions sometimes occur upon injury, whereas medial condyle injury may develop gradually after injury because of instability. However, Sugiu et al. reported that cartilage lesions had increased on second-look arthroscopy after successful ACLR.31) Their findings suggested that cartilage degeneration occurs progressively after ACLR. Further long-term follow-up with X-ray investigations and MRI will be necessary to evaluate and compare the progression of cartilage injury in the ERS and non-ERS groups.
The current study has several limitations that should be considered. First, the number of participants in the ERS group was relatively small, and the sample was not randomly selected. To reduce secondary intra-articular injuries, our primary therapeutic strategy for ACL-injured patients is to reconstruct the ACL as early as possible. As a result, patients in the ERS group were limited to athletes who were eager to RTS. Second, secondary meniscal injury was determined using two different methods: MRI and arthroscopic findings with probing. The MRI scan may have missed minor partial-thickness tears. Third, the current data were retrospectively collected, and all subjects underwent reconstruction surgery, likely excluding some coper subjects. Fourth, patients whose early RTS was successful without requiring future surgery are absent. Another limitation is that the sports performance level was evaluated using an NRS. We defined 10 as the same as the pre-injury level, and 0 as being impossible to participate in the game. But 1 to 9 were not defined and were completely subjective scores registered by the players. It would have been difficult to define performance levels more rigorously because the patients were involved in different sports. Finally, this study did not compare clinical results after ACLR. Despite these limitations, the current data are clinically relevant and indicate that healthcare providers should undertake careful management of young ACL-injured athletes who are eager to RTS for the rest of the season, because their sporting performance may be low and they may not be satisfied with their decision to RTS.
Although ERS in the same season as injury without ACLR appears to be a feasible strategy for ACL injury, patients’ self-estimated performance levels were low, and meniscal and cartilage injuries significantly increased. Physicians should clearly explain to patients that, in ERS, they will be unlikely to achieve their original sporting level and that ERS has a high complication rate.
The authors declare that they have no competing interests.