2022 Volume 7 Article ID: 20220055
2022 Volume 7 Article ID: 20220055
Objectives: The WISH-type S-form hip brace (WISH brace) has significantly improved hip function and functional mobility in patients with hip osteoarthritis (OA). However, most patients later undergo surgery. The main purpose of this study was to evaluate how long the orthosis can be effectively used by patients with hip OA, and to reveal the associated prognostic factors.
Methods: This prospective study examined the survival curve of the equipment by using surgery as an endpoint and investigated how the duration of use affects patients. Harris Hip Score, muscle strength, and the Timed Up and Go test (TUG) were evaluated as prognostic factors.
Results: By drawing the survival curves of 26 patients, approximately one third were expected to be still using the brace after 7 years. A rapid decrease in use was observed at around 1 year. A significant difference between patients with and without bracing at 1 year was found for the TUG result with the unaffected leg inside (ULI) at the start of bracing. A cut-off value of 9.5 s for the TUG with ULI significantly differentiated patients with and without bracing at 1 year, suggesting a possible predictor of brace survivorship in the early phase.
Conclusions: The TUG with ULI with a cut-off value of 9.5 s, or at most 10 s, may be a possible predictor of persistence of brace use in the early phase.
Hip osteoarthritis (OA) is a common condition worldwide, particularly in older individuals.1) Radiographic deterioration over time is common, although the rate varies from person to person.1) The pain associated with hip OA usually limits function, so therapy for hip OA has two major objectives: to relieve pain and to preserve hip functions.2)
From a general literature review, interventions for hip OA use surgery in 74% of cases, pharmaceuticals in 19%, and non-pharmaceuticals in 7%.3) For total hip arthroplasty (THA), the latest second-generation non-cemented stems with a proximal circumferential porous or hydroxyapatite (HA) coating are considered to be suitable for young OA patients, but polyethylene wear, liner problems, and osteolysis around THAs are major problems with modern non-cemented acetabular components.4) Pharmacologic therapy is effective in reducing pain and improving function of the hip but has side effects.2)
As a conservative therapy for hip OA, we developed the WISH-type hip brace.5) Suitable candidates for this therapy are patients that experience relief from hip pain during weight-bearing gait by applying manual pressure on the greater trochanter. We have previously described the positive effects of the brace on the hip function of patients with hip OA.5,6) The relief of pain in the stance phase by use of the brace equipment results in strong steps in the early stance phase, as demonstrated by force-plate analyses.7) Another direct effect of this brace is significant improvement of postural control.8) Furthermore, the average time to complete the Timed Up and Go test (TUG) was significantly shorter in patients with the brace, especially during the turning phase.9) This improvement of functional mobility may be related to augmentation of the hip-abduction muscle strength, acquired by daily walking exercise.10) Although both direct and indirect positive changes have been observed in response to the WISH-type brace,11) some patients underwent surgery in the follow-up course of this orthosis therapy.5) The purpose of this brace is not to replace surgical management forever, but rather to delay the need for it.
The main purpose of this study was to evaluate how long the orthosis offers benefit to patients with hip osteoarthritis. Using surgery as an endpoint, we investigated how the brace affected the subjects’ overall long-term survival and the shape of the survival curve.
Patients with symptoms of unilateral OA of the hip were referred to the outpatient clinic of our institution. Hip OA was defined according to the clinical criteria of the American College of Rheumatology.12) Patients in whom the hip pain induced by weight bearing during gait was notably reduced by manual pressure on the greater trochanter were recruited for this investigation. Subjects were excluded if they were on a waiting list for hip replacement, had previously undergone hip replacement, or used a WISH brace for both hips. The radiological grade of OA was estimated according to the grading system proposed by Crowe et al.,13) and patients with radiological grade III or IV were excluded. In addition, the Kellgren and Lawrence grade (K/L grade) and lateral center edge angle (LCE angle) were evaluated.
Fifty-one patients accepted this orthosis therapy with WISH-type hip brace during the clinical trial period from October 2006 to September 2015. The TUG was performed by 26 patients from August 2007 to April 2013, and these participants were analyzed until September 2015. Age, height, weight, medical history, complications, and drug therapy were recorded for each patient.
This study was conducted after approval by the Gunma University Hospital Clinical Research Review Board (Approval No. 515). Written informed consent for the study was obtained from each participant.
Hip BraceThe WISH-type hip brace (PO Support, Takasaki, Gunma, Japan)5) was manufactured based on the design concept of the Wakayama Medical College.14) We improved the brace to make it lighter and more compact, and named this version the WISH-type. The resultant hip brace weighed around 0.9 kg, and the lateral prominence caused by the lateral bar was reduced.5) As previously reported,5) the brace consists of a pelvic portion, an S-form portion, and a lateral bar connecting them. The pelvic portion of the hip brace holds it in the correct position. The greater trochanter pad serves as a fulcrum and pushes the great trochanter inward when the affected limb is abducted or bears weight. The lateral bar has two joints, allowing flexion, extension, and abduction of the affected hip.
Exercise TherapyPatients fitted with the WISH brace were required to walk for at least 30 min every day to strengthen muscles around the hip joint required for gait. Weight exercises for strengthening hip muscles were suggested as home exercise. The performance of gait exercise in water was also recommended.5)
Hip Function AssessmentsHip function was evaluated using the Harris Hip Score (HHS)15) as the primary outcome measure. The HHS consists of four variables: pain, functional capacity, range of motion, and deformity. The maximum score is 100, and scores below 70 reflect poor function (poor category).15)
Timed Up and Go TestThe TUG measures, in seconds, the time taken by an individual to stand up from a standard armchair (approximate seat height of 46 cm), walk a distance of 3 m, turn, walk back to the chair, and sit down again.16) The subjects wore their regular footwear. When performing the TUG, subjects were given verbal instructions to stand up from the chair, walk 3 m as quickly as possible, pass around a cone on the floor, walk back, and sit down.17) Each subject performed the TUG separately with right and left turns. When a patient walked and rounded the cone with the equipped leg inside (ELI), the TUG with spin turn was evaluated. Conversely, when the test was performed with the unequipped leg inside (ULI), the TUG with step turn was evaluated.9) A stopwatch was used to time the performance.
Muscle Strength Assessment around the HipMuscle strength testing was performed as described previously.10) Muscle strength testing was performed with the patient lying on an examination table according to the method described by Thorborg et al.18) using the Power track II Commander Hand Held Dynamometer (HHD) (JTECK Medical, Midvale, UT, USA). The HHD was calibrated on each test day and all test procedures were standardized. All strength tests were isometric. Each subject performed hip flexion (FLEX), abduction (ABD), adduction (ADD), and knee extension (K-EXT). FLEX and K-EXT were assessed in the sitting position, and ABD and ADD were assessed in the supine position. K-EXT was measured according to a standardized method. The participants were instructed to stabilize themselves by holding the sides of the table with their hands. The examiner applied resistance in a fixed position and the patient exerted a 5-s isometric maximum voluntary contraction against the dynamometer and the examiner. For assessment of hip movements, the examiner’s hand was set just above the knee joint to avoid involvement of the knee joint. For examination of K-EXT, resistance was applied at the level of the malleoli. Each individual test was administered three times to reduce possible learning effects. There was a 30-s rest period between two consecutive trials to avoid a decline in strength across trials due to fatigue in patients with spinal cord injury.19) The mean maximal torque values were divided by the patient’s body weight to calculate the relative muscle torque (Nm/kg).
The TUG was performed and muscle strength and hip function were assessed prior to bracing treatment on the day the brace was completed and scheduled to be fitted. Hip function was assessed after another year or just before operation within a year.
Statistical AnalysesThe follow-up period was the difference between the date of orthosis application and the day of surgery or the last observation. Using surgical intervention as an endpoint of the survival of brace use, survivorship curves were created by the Kaplan–Meier method.20) The relationship between TUG at the start of orthosis therapy and the persistence of the orthosis therapy 1 year later was evaluated using Fisher’s exact test. Focusing on TUG with ULI, we divided the cohort into two groups based on a speed threshold of 9.5 s. We created survival curves for these groups and compared the results using a log rank test.21) Age, height, weight, hip function, TUG time, and muscle strength were compared between patients using the brace continuously for longer than 1 year (Over-1Y group) and those ceasing use by 1 year (Interrupted group). Differences were evaluated using a two-sample t-test. Comparisons of HHS at 1 year (Over-1Y group) or just before surgery (Interrupted group) with those at entry were analyzed by paired t-test. A P value less than 0.05 was considered significant.
A total of 26 patients (1 male, 25 females) were recruited (Table 1). The patients ranged in age from 29 to 74 years, and the average age was 53.7 years (SD, 10.7 years). All patients had osteoarthritis secondary to acetabular dysplasia. Twelve patients had right-side involvement and 14 had left-sided involvement. The radiological grade was determined according to Crowe et al.13) Seventeen patients were assessed as grade I and 9 patients were grade II. For K/L grade, 2 patients were grade II, 8 patients were grade III, and 16 patients were grade IV. The LCE angle was 2.2 ± 8.1 degrees. Medical history and complications included lumbar spinal canal stenosis in 3 patients, lumbar disk herniation in 2 patients, spine osteoarthritis in 5 patients, osteoporosis in 1 patient, cervical spondylosis in 2 patients, and lumbar spondylosis in 1 patient. Drug therapy included the use of NSAIDs in 19 patients, prostaglandin E1 in 9 patients, and muscle relaxant in 5 patients. Of the 26 patients, 13 received THA and 1 received rotational acetabular osteotomy (RAO). The average time to surgery was 26.9 (SD 19.4) months.
| Patient number | Age (years) | Height (cm) | Weight (kg) | BMI (kg/m2) | Radiological gradea | Follow-up timeb (months) | Operation | HHS | |
| Start | 1 yearb | ||||||||
| 1 | 48 | 150 | 51.6 | 22.9 | I | 47 | THA | 49.7 | 75.7 |
| 2 | 41 | 162 | 64 | 24.4 | II | 56 | THA | 46 | 88 |
| 3 | 59 | 167 | 58 | 20.8 | I | 62 | THA | 55 | 94 |
| 4 | 70 | 155 | 63 | 26.2 | I | 85 | - | 51 | 90 |
| 5 | 52 | 154 | 50 | 21.1 | II | 78 | - | 60.8 | 75.7 |
| 6 | 59 | 157 | 42 | 17 | II | 62 | - | 48.7 | 66 |
| 7 | 50 | 153 | 44.5 | 19 | I | 62 | - | 47 | 95 |
| 8 | 59 | 148 | 46.5 | 21.2 | I | 30 | THA | 56 | 76 |
| 9 | 50 | 150 | 46 | 20.4 | II | 56 | - | 63 | 82.7 |
| 10 | 49 | 153 | 65 | 27.8 | II | 35 | THA | 50 | 95.7 |
| 11 | 38 | 158 | 58 | 23.2 | II | 39 | THA | 47.7 | 94 |
| 12 | 54 | 156 | 72 | 29.6 | I | 45 | - | 65.7 | 69 |
| 13 | 51 | 167 | 58 | 20.8 | I | 37 | THA | 66 | 60 |
| 14 | 57 | 163.5 | 65 | 24.3 | I | 43 | - | 61 | 81 |
| 15 | 65 | 152 | 49 | 21.2 | I | 16 | THA | 59 | 93 |
| 16 | 52 | 154 | 48 | 20.2 | I | 41 | - | 55.7 | 91.7 |
| 17 | 50 | 161.5 | 52 | 19.9 | II | 39 | - | 76 | 78 |
| 18 | 64 | 155 | 54.5 | 22.7 | I | 35 | - | 62.7 | 76 |
| 19 | 29 | 155 | 50 | 20.8 | I | 32 | - | 49.7 | 93 |
| 20 | 74 | 157 | 50 | 20.3 | I | 29 | - | 68 | 69.7 |
| 21 | 66 | 143 | 57 | 27.9 | I | 12 | THA | 62.7 | 60c |
| 22 | 43 | 153 | 55 | 23.5 | II | 7 | THA | 60 | 79c |
| 23 | 65 | 152.5 | 60 | 25.8 | I | 7 | THA | 66 | 53.3c |
| 24 | 58 | 149 | 56 | 25.2 | II | 11 | THA | 53.3 | 85c |
| 25 | 36 | 158 | 48 | 19.2 | I | 9 | RAO | 63 | 51c |
| 26 | 56 | 158 | 60 | 24 | I | 8 | THA | 41.7 | 65.7c |
| Average | 53.7 | 155.4 | 54.7 | 22.7 | 37.8 | 57.1 | 82.2 | ||
| SD | 10.7 | 5.6 | 7.4 | 3.1 | 22 | 8.3 | 11 | ||
a Radiological grade was evaluated according to Crowe et al.13)
b Time after starting brace use.
c Measurement taken just prior to operation.
Figure 1 shows the survivorship curve of the 26 patients, using surgical intervention as an endpoint of the survival of the brace equipment. A relatively rapid decrease in the curve is seen at around 12 months. Interestingly, one third of patients were expected to use the brace for 7 years.

Survivorship curve for all patients. Mo, months.
Because the survival curve showed a rapid decrease at around 1 year, we examined which of the parameters evaluated at the starting point affected the persistence of the brace over 1 year. Comparing the Over-1Y group (n=20) and the Interrupted group (n=6), there were no significant differences in HHS (56.9±8.3 vs 57.8±9, P=0.83), age (53.6±10.6 vs 54±12.1 years, P=0.93), height (156.4±5.4 vs 152.3±5.7 cm, P=0.12), weight (54.4±8.2 vs 56±4.4 kg, P=0.53), body mass index (BMI; 22.2±3.0 vs 24.3±2.9 kg/m2, P=0.15), or muscle strength (Table 2). However, the TUG result with ULI in the Over-1Y group (7.94 ± 1.27 s) was significantly faster than that for the Interrupted group (9.37 ± 1.65 s) (Fig. 2A), whereas the TUG result with ELI showed no significant difference between the two groups (8.19 ± 1.76 vs 9.12 ± 1.37 s,P=0.25) (Fig. 2B).
| Muscle measure | Affected (Nm/kg) | Unaffected (Nm/kg) | ||||||||
| Over-1Y group | Interrupted group | P value | Over-1Y group | Interrupted group | P value | |||||
| Average | SD | Average | SD | Average | SD | Average | SD | |||
| FLEX | 0.49 | 0.21 | 0.37 | 0.08 | 0.28 | 0.78 | 0.22 | 0.5 | 0.16 | 0.07 |
| ABD | 0.38 | 0.14 | 0.42 | 0.1 | 0.73 | 0.53 | 0.16 | 0.46 | 0.09 | 0.5 |
| ADD | 0.37 | 0.13 | 0.4 | 0.17 | 0.75 | 0.42 | 0.14 | 0.41 | 0.12 | 0.95 |
| K-EXT | 0.45 | 0.19 | 0.47 | 0.04 | 0.88 | 0.75 | 0.2 | 0.63 | 0.1 | 0.21 |
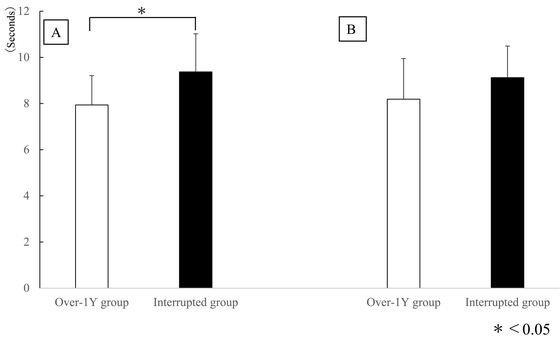
(A) Comparison of average time of TUG with ULI between the Over-1Y group and the Interrupted group. (B) Comparison of average time of TUG with ELI between the Over-1Y group and the Interrupted group. Asterisk indicates significant difference with P<0.05.
In the Over-1Y group, the mean HHS score significantly improved from 56.9±8.3 to 82.2±11.0 (P<0.01) at 1 year. In the Interrupted group, no significant improvement of HHS was observed before surgery (from 65.7±13.8 to 57.8±8.97; P=0.365).
Cut-off Value for TUG with ULIFocusing on the TUG with ULI, we postulated a walking speed threshold of 9.5 s and divided the cohort into two groups: 9.5 s or slower (slower group) and faster than 9.5 s (faster group). As shown in Fig. 3, the survival rate decreased gradually in the faster group. In contrast, the survival rate in the slower group decreased rapidly over 12 months, although the log rank test did not indicate a significant difference (P=0.08). However, Fisher’s exact test with a cut-off value of 9.5 s showed a significant difference between the two groups (P<0.034), suggesting that 9.5 s for TUG with ULI may be a predictor of persistence of brace use in the short term.

Survivorship curves of patients showing faster (<9.5 s, blue line) and slower (>9.5 s, red line) TUG times with ULI. The rapid decrease over 12 months observed in Fig. 1 was not observed in the survival curve for the faster group. Mo, months.
The survivorship curve for persistence of the WISH-type hip brace use showed a relatively rapid decrease around 12 months, although continuous use by one third of patients was expected to be seen for 7 years. The patients in the Over-1Y group showed shorter times for the TUG with ULI at entry. Interestingly, HHS was significantly improved after 1 year in the Over-1Y group, whereas this improvement was not observed in the Interrupted group. Using a walking speed threshold of 9.5 s for the TUG with ULI, the drop in the survivorship over 12 months was much less pronounced in the faster group. Fisher’s exact test with a cut-off value of 9.5 s showed a significant difference between the fast and slow groups.
There are few studies describing the effects and limitations of hip braces for hip OA.22) In addition, there are few known scientific analyses on the persistence of bracing in hip OA patients. Although a review article about the hip brace was published recently, the role of the brace was focused on postoperative support after THA.23) We have scientifically and biomechanically investigated the WISH-type hip brace preoperatively.5,6,7,8,9,10,11) Another hip brace based on a new concept has also been reported.24) To our best knowledge, the present report is the first analysis of the persistence of hip bracing (i.e., the longevity of the brace until surgery). It is noteworthy that one third of the patients were expected to use the hip brace continuously for more than 7 years. Although the purpose of hip bracing is not to permanently replace surgical management,5,24) it has the potential to help patients avoid invasive surgery such as THA up until natural death without suffering the effects of hip disability in the interim.
The survivorship curve for persistence of the brace depicted a relatively rapid decrease at around 12 months, indicating the existence of patients in whom the effect of the brace was small or was lost within 1 year. This was confirmed by the hip functional scores that showed less improvement in HHS in the Interrupted group at 1 year, whereas the HHS in the Over-1Y group improved significantly. There was a significant difference in the TUG result with ULI between these groups. The improvement in the TUG result through use of the WISH-type hip brace was significant with ULI but not for ELI for the patients with unilateral hip OA.9) When a patient walked and rounded the cone with ULI, the TUG with step turn was evaluated for the affected limb. In the stepping strategy, hip abductor muscles in the stance leg control the duration of swing of the opposite leg.25) During turning with ULI, the affected hip joint rotates externally with abduction. A short-term longitudinal study revealed that the inherent hip abduction muscle strength was improved by the WISH brace to the same degree as the unaffected limb.10) Taken together, initial functional mobility evaluated from the TUG with ULI, which is mainly related to the abduction muscle strength, may be a predictor for the persistence of brace equipment use in the early phase, although the abductor muscle strength itself was not a direct predictor in the present study.
Fisher’s exact test with a cut-off value of 9.5 s showed a significant difference between the faster and slower groups. In addition, these two groups showed different Kaplan–Meier survival curves. Podsiadlo and Richardson reported that TUG results of less than 10 s could be used to identify freely independent individuals.16) Arnold and Faulkner reported a higher likelihood of frequent near-falls if TUG scores in older adults with hip osteoarthritis were over 10 s or if they were over the age of 75.26) Furthermore, Shumway-Cook et al. found that a TUG result of over 14 s in older adults indicates the risk of a fall.17) In the present study, the mean age of the participants was 53.7±10.7 years, which was lower than the subjects evaluated by Shumway-Cook et al.17) Taken together, 9.5 s, or 10 s at most, may be an appropriate cut-off value for the TUG, which is completed by walking as quickly as possible, when predicting the persistence of brace use in the early phase.
In summary, the survivorship curve of the equipment, using surgical intervention as an endpoint, revealed that one third of patients were expected to continue to use the brace for 7 years. Patients using bracing continuously for longer than 1 year were associated with significantly shorter times in the TUG using ULI at entry. When the walking speed threshold was taken as 9.5 s for the TUG with ULI, the survival rate decreased rapidly in the slower group over 12 months but decreased gradually in the faster group. Although this difference was not significant, Fisher’s exact test with a cut-off value of 9.5 s showed a significant difference between the two groups. This result suggests that a cut-off value of 9.5 s (or 10 s at most) for the TUG with ULI may be a predictor of persistence of brace use in the early phase.
No significant difference was observed in function scores or muscle strengths around the evaluated hip except for functional mobility. Given that muscle strength is related to functional mobility, more predictors of muscle strength should be extracted in further studies with larger numbers of subjects. One obvious limitation of the current study was the low number of subjects. In addition, we did not perform imaging evaluation before and after brace therapy intervention. However, we consider that the evaluation of joint space width in patients with OA of the hip is very important. Therefore, the use of imaging evaluations before and after brace therapy intervention is recommended for prosthesis prescription. This issue should be examined separately in future detailed studies.
The use of hip braces offers the possibility of avoiding invasive surgeries, such as THA, but must be carefully monitored over long periods of time. This outcome would be the ultimate and unexpected benefit of hip brace use for patients with hip OA.
This work was supported in part by a Grant-in-Aid for Young Scientists JP18K17710 (E.S.) from the Japan Society for the Promotion of Science.
The authors report no conflicts of interest.