2020 年 37 巻 3 号 p. 83-94
2020 年 37 巻 3 号 p. 83-94
Fractures of the mandibular condyle make up a significant proportion of all mandibular fractures. Open reduction and internal fixation has become the standard treatment for subcondylar fractures as a result of recent advancements in technology, the development of osteosynthesis devices, enhanced surgical techniques, and the introduction of various feasible surgical approaches. This clinical mini-review discusses several routine intraoral (with or without endoscopic assistance) and extraoral (e.g., preauricular, retromandibular, submandibular, and high-submandibular) surgical approaches to open treatment of open reduction and internal fixation of mandibular condylar fractures. It focuses on the features of these approaches as well as their clinical applicability and complications.
Mandibular condylar fractures make up 18–52% of all mandibular fractures, such that the mandibular condylar process is the most common site of such fractures [ 1, 2]. Although absolute and relative indications for open reduction and internal fixation (ORIF) have been proposed, treatment choices in such patients tend to be based on the surgeon’s experience and preferences [ 3, 4]. However, debate continues over whether closed or open treatment is appropriate for management of condylar fractures [ 1]. When mandibular condylar fractures cause oromandibular dysfunction, surgical treatment may be needed for better occlusion and temporomandibular joint function because accurate reduction and rigid fixation allow good anatomical repositioning and immediate functional recovery [ 2- 4].
Surgical management of condylar fractures has increasingly become the standard treatment because of advancements in technology, the development of indigenous osteosynthesis devices, enhanced surgical techniques, and better understanding of surgical anatomy [ 3- 5]. A recent systematic review and a meta-analysis showed that ORIF provides superior oral and maxillofacial functional clinical outcomes during the management of adult mandibular condylar fractures, with more rapid rehabilitation of oromandibular function and reintegration into social activity, based on both subjective and objective comparisons to conservative treatment [ 5- 7]. These clinical benefits have helped ORIF become the standard treatment for condylar fractures, supported by technical progress in less invasive surgical approaches, an accumulation of clinical evidence, the development of hardware (e.g., three-dimensional anatomically specific and biomechanically stable locking plate systems for open treatment of condylar fractures), the introduction of computer-assisted surgical techniques and devices, and better understanding of the osteobiology of maxillofacial fracture healing (including mandibular condylar fractures) [ 6- 8].
The mechanism of fixation plate systems used in ORIF following correct anatomical reduction of the fractured segment in patients with mandibular condylar fractures is based on the biomechanical and biophysical principles of functionally stable osteosynthesis during biting and the occlusal three-dimensional forcing mechanism [ 9]. Knowledge of these principles has revealed the importance of three-dimensional shape buttress fixation design with locking miniplate fixation for sufficient neutralization of tension and compression forces to promote stable healing at the functional temporomandibular joint [ 9, 10]. Currently the most commonly used osteosynthesis procedure is the use of two-miniplate fixation secured with screws, as well as a three-dimensional anatomical miniplate system. Dynamic osteosynthesis, a key principle of miniplate osteosynthesis, stipulates that plates must be placed along the physiological tension lines that appear during use [ 9, 10]. When the osteosynthesis plate position and physiological strain lines are superimposed in this technique, the posterior plate is aligned along the compression strain lines, whereas the anterior plate is located along tensile strain lines below the mandibular notch [ 9]. From a mechanical perspective, this two-miniplate technique is favorable and helps to satisfy the principles of dynamic osteosynthesis [ 10]. Two-plate techniques are typically required to achieve stable fixation, and a newly developed frame-like three-dimensional anatomical plate can also provide good stability, similar to conventional two-plate techniques [ 11].
When open treatment of ORIF is selected, several surgical approaches can be used to expose, reduce, and stabilize the fracture site [ 12]. Each of these approaches has its own set of advantages and disadvantages, and their use is largely determined by each surgeon’s experience and preferences [ 12, 13]. Surgical approaches to treating mandibular condylar fractures are broadly classified into intraoral and extraoral approaches. Intraoral approaches can be performed with or without endoscopic assistance. However, extraoral approaches are commonly used because they provide better visualization of the fracture site, thereby facilitating fracture reduction and fixation. To establish visualization, different approaches to the mandibular condyle are used [ 12]. The four most commonly used approaches are preauricular, retromandibular, submandibular and high-submandibular [ 12, 13]. The choice of approach is often based on the type of fracture [ 12, 13]. Fractures are subdivided into condylar head (intracapsular), and subcondylar fractures of the condylar neck (extracapsular) and condylar base as in Fig. 1 [ 12, 13]. The preauricular or perilobular approach may be useful for treating high condylar fractures, the retromandibular approach may be useful for treating medium fractures, and the retromandibular approach or a variety of submandibular approaches (e.g., a recently popularized high-submandibular, high-perimandibular approach) may be useful for treating medium and lower condylar fractures. However, the use of extraoral approaches is further complicated by increased risk for injury to the facial, great auricular, and auriculotemporal nerves as well as visible scars, sialoceles, Frey syndrome, and salivary fistulae compared to intraoral approaches as in Fig. 2 [ 12- 14].
This clinical mini-review presents an overview of several routine intraoral and extraoral surgical approaches to open treatment of ORIF of mandibular condylar fractures. It focuses on the features of these approaches as well as their clinical applicability and complications.
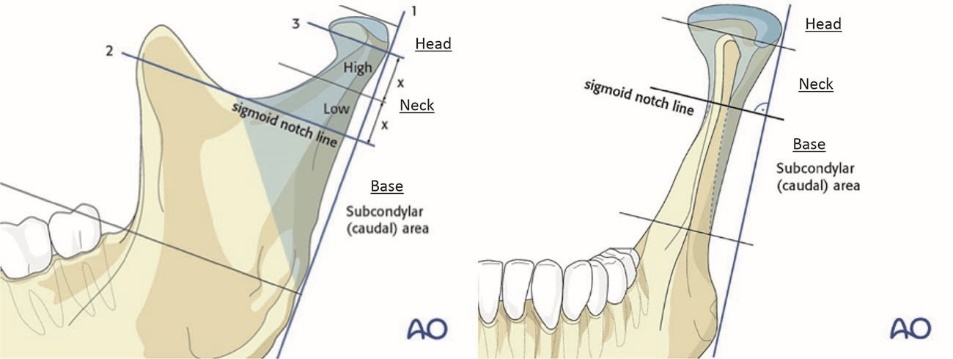
AO classification. The condylar process and head is a mandibular subunit defined by an oblique line running backward from the sigmoid notch to the upper masseteric tuberosity. The condylar process is divided into three subregions: head, subcondylar areas of the neck, and base. Source: https://surgeryreference.aofoundation.org/cmf/trauma/ (Accessed June 29, 2020)
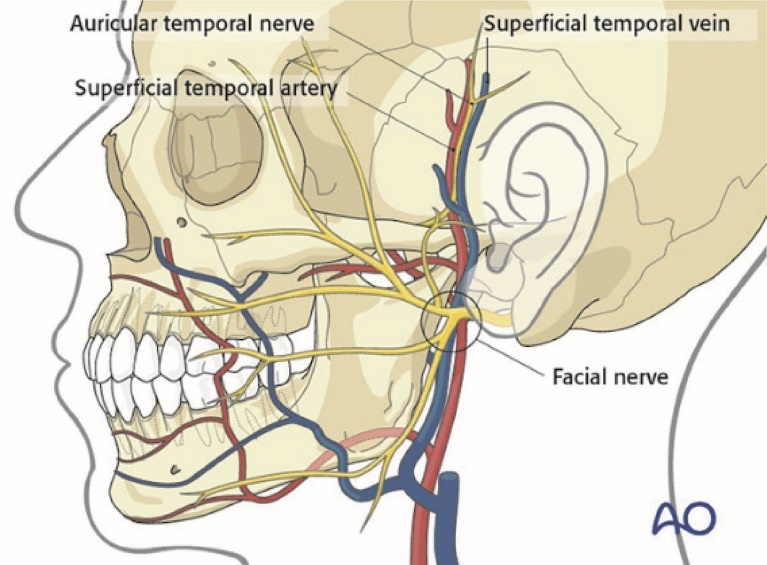
An overview of surgical anatomy for open treatment of ORIF of mandibular condylar fractures. Source: https://surgeryreference.aofoundation.org/cmf/trauma/ (Accessed June 29, 2020).
Intraoral Approaches (With or Without Endoscopic Assistance)
The intraoral approach was first described by Silverman in 1925 for low subcondylar fractures ( Fig. 3A) [ 15]. Later, Ellis and Dean evaluated this surgical approach in a comprehensive instructive article regarding the rigid fixation of mandibular condylar fractures [ 16]. They emphasized two advantages: no facial scars and no risk for facial nerve damage. Note that they also mentioned poor accessibility. They also described transcutaneous trocar insertion in the preauricular region for instrumentation and concluded that it was limited to use in low subcondylar fractures of the condylar neck and condylar base fractures with minimal edema [ 16, 17]. However, these comments were based on old instrumentation and devices. A different conclusion might have been reached had modern surgical instruments, including the small-head angulated screwdriver, been available then or a similar clinical evaluation been conducted using intraoral approaches alone, as we reported in the previous article [ 1]. With updated instrumentation, the risk for external scarring (including during the removal of the plate and screw) is completely eliminated. Furthermore, both facial nerve damage and salivary fistulae are avoided.
A sole transoral incision, similar to sagittal splitting ramus osteotomy in standard orthognathic surgery, is made in the mucosa through the periosteum overlying the external oblique ridge [ 1, 18]. The periosteum and masseter muscle are elevated over the ascending mandibular ramus lateral to the posterior border. The entire surface of the ramus, from the sigmoid notch to the mandibular angle, can be visualized using a set of Bauer retractors, long Langenbeck retractors, or other soft tissue retractors to provide a clear surgical field for ORIF [ 1, 18, 19]. Although the surgical working space for gaining access to the subcondylar area is somewhat limited, no transbuccal trocar or additional surgical incision is needed for instrumentation. In this regard, an endoscopically assisted view can enhance and support clearer views during ORIF. Kitagawa et al. showed that the more complex procedure of screw tapping without a transbuccal stab trocar is also possible using a transoral approach alone for ORIF of slightly dislocated subcondylar fractures with an angulated screwdriver [ 20]. The working space is limited, in particular when reducing severely dislocated condylar segments. However, each dislocated condylar segment is reduced anatomically using curved periosteal elevators and manipulation of distal mandibular segments.
Recently, an endoscopically assisted approach to open reduction and miniplate fixation of condylar mandibular fractures that features a limited transoral incision has drawn considerable attention from surgeons and patients ( Fig. 3A) [ 1, 18, 21]. Surgical management has become easier since the introduction of endoscopically assisted open reduction. Transoral endoscopically assisted condylar fixation has gained in popularity because the surgeon has direct visualization of a magnified and illuminated operative field and the assistant has an unobstructed view, which overcomes the limitations of intraoral approaches [ 21, 22]. Over the past two decades, endoscopically assisted open treatment of subcondylar fractures has been widely used in several surgical institutions, including our Shimane University Hospital and Kagawa Prefectural Central Hospital [ 1]. In these institutions, pioneering maxillofacial surgeons have used minimally invasive surgical procedures to treat maxillofacial trauma with good clinical results and relatively long-term follow-up [ 21- 23]. Internationally, some of these pioneering institutes have reported randomized controlled studies comparing extraoral (e.g., submandibular, preauricular, and retromandibular) approaches without endoscopic assistance for ORIF to a transoral endoscopically assisted procedure [ 23, 24]. It is noteworthy that the transoral endoscopically assisted procedure generally produces better clinical results with respect to the occurrence of surgical complications (e.g., facial nerve damage and scar formation) [ 7, 22]. However, direct visualization and accessibility of the fracture site remain difficult. Moreover, specialized instruments and training are necessary. Our opinion is similar to that of other clinical researchers: Intraoral approaches offer great advantages in terms of minimal surgical complications (e.g., surgical risks, visible scars, facial nerve injury) compared to extraoral approaches [ 1, 12, 13, 22].
However, the applicability of intraoral approaches may be still limited to linear mandibular subcondylar fractures. In addition, these approaches might be limited to condylar neck and condylar base fractures with condylar segment deviation [ 22- 24]. Although intraoral approaches are associated with minimal or no risk for facial nerve injury, treating condylar fractures intraorally (even if assisted endoscopically) presents technical difficulties and may impact the predictability of the results. Condylar head and high condylar neck fractures are not possibly manageable by intraoral approaches [ 1, 12, 13]. Severely dislocated subcondylar fractures should also be approached surgically with other extraoral approaches to secure clinical outcomes of ORIF with immediate functional recovery [ 22].
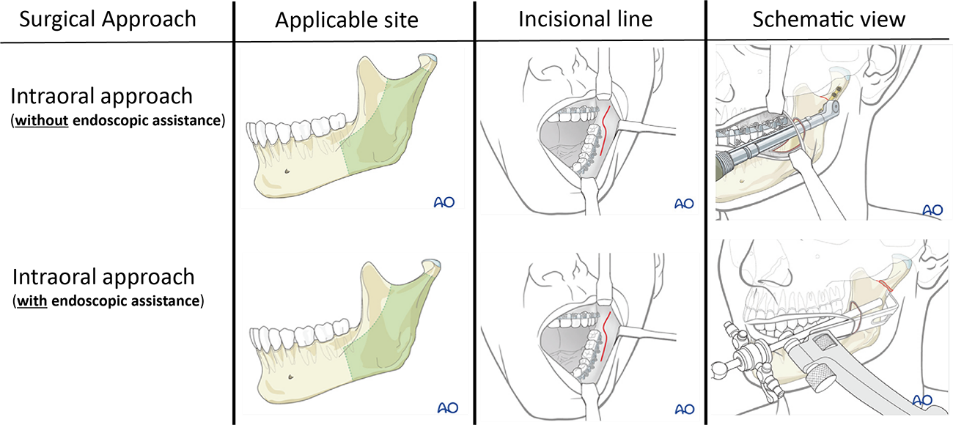

Fig. 3. An overview of several routine intraoral and extraoral surgical approaches to open treatment of ORIF of mandibular condylar fractures. The schematic view of High-submandibular approach in Fig. 3B was referred to and modified by reference 36. Source: https://surgeryreference.aofoundation.org/cmf/trauma/ (Accessed June 29, 2020).
Extraoral Approaches
Preauricular approach
The preauricular approach was first described by Thoma in 1945 and has since been discussed by Rowe and others ( Figure 3B) [ 25, 26]. It is commonly preferred for condylar head and upper condylar neck fractures, as applicable [ 12]. In general, the surgeon approaches the fracture by incising 3– 4 cm from the inferior border of the tragus toward the external auditory canal, along the skin crease of the anterior part of the external ear. This approach is particularly useful for medially displaced condylar fragments [ 12, 25- 27]. The advantages of this technique include excellent access to the fractured stump, convenient manipulation of the fractured segment, and minimal scar formation. The main risk associated with this approach is facial nerve injury [ 25]. However, the facial nerves remain at risk for injury with the preauricular approach, which cannot be ignored. Some surgeons have reported unsatisfactory results with the preauricular approach, such as an inability to raise the eyebrows, loss of ability to create forehead wrinkles, and ptosis [ 13, 14]. The incidence of facial nerve paresis ranges from 1% to 32% after this surgery [ 28]. To avoid the risk for facial nerve injury, a recent clinical study modified this technique to a supratemporalis approach [ 25]. Unlike in the traditional preauricular approach, in the supratemporalis approach the separation plane is located between the deep temporal fascia and the temporalis. Some clinical reports have noted that the supratemporalis approach prevents facial nerve injury and does not increase the frequencies of other complications [ 13, 25, 28]. Therefore, it should typically be used as a safe and standard approach to open treatment of ORIF at the condylar head extending to upper condylar neck fractures, for which results remain predictable.
Retromandibular approach
The retromandibular approach was first described by Hinds in 1967 ( Fig. 3B) [ 29]. This approach provides excellent visualization of the condylar neck and base. The surgeon approaches the condylar fracture by dissecting the skin and subcutaneous tissue vertically to the mandibular angle, using a 3 cm incision line that extends 5 mm inferior to the auricular lobe [ 12, 16]. Subcutaneous dissections are further divided into transparotid and non-transparotid of retroparotid (i.e., transmasseteric and anteroparotid/posteroparotid) approaches. The advantages of this approach include a shorter working distance from the skin incision to the condyle. The good access and visualization of the posterior border of the mandible and sigmoid notch facilitate fracture manipulation and reduction and leave an inconspicuous scar. However, this method requires a bisecting incision through the parotid gland, which increases risks for facial nerve injury and sialoceles or salivary fistulae [ 12, 13, 28]. Axonotmesis or neuropraxia can occur when excessive traction is applied on the retractor during the retromandibular approach to ORIF. The reported incidence of transient facial nerve palsy is about 0–30%, but almost all these cases resolve within 6 months [ 13, 29, 30]. The incidence of permanent facial nerve palsy is reported to be very low. Ellis et al. found a rate of 17.2% transient facial nerve palsy in 93 treated patients, all of whom exhibited resolution within 6 months [ 16, 17]. Salivary fistulae are observed at low rates. Paresthesia, hematoma, Frey syndrome, wound infection, and wound scar formation are also reported in the literature, but their rates are very low. A slightly modified approach to treating condylar neck and base fractures minimizes the occurrence of these complications. Clinical studies have shown that the retromandibular approach has many advantages: good exposure, minimal scarring, simple manipulation, short operating time, and minimal risk for facial nerve damage [ 16- 18, 30, 31]. Thus, it is the best choice for treating condylar neck and condylar base fractures with predictable results.
Submandibular approach
The submandibular approach is a classic method of reaching the mandibular ramus and posterior body region ( Fig. 3B). It is occasionally referred to as the Risdon approach, as it was first described by Risdon in 1934 to treat temporomandibular joint ankyloses [ 32]. This approach can be used to obtain access to condylar fractures during open treatment of ORIF [ 12, 13]. The surgeon makes an incision at a site 2–3 cm inferior to the inferior mandibular border, parallel to the inferior mandibular border, or along the skin crease. Note that descriptions of the approach differ among studies, but all incisions are made below the inferior mandibular border. This approach provides excellent visualization, which is limited to the condylar base region [ 12, 13]. However, it is easily learned and performed. Moreover, it requires virtually no learning curve and has extensive documentation in the surgical literature [ 28, 33].
Approaching the mandible from an incision below the marginal mandibular nerve is the most crucial aspect of the Risdon approach and may complicate facial nerve palsy of the marginal mandibular branch [ 28, 33]. A relatively longer incisional line is required, which may result in a longer and more conspicuous scar, compared to other extraoral approaches. Many studies have described frequent lesions of the facial nerve, mainly of the marginal branch, reaching up to 48.1% and 12.5% of transient and permanent facial palsies, respectively [ 14, 28, 33]. The causes include blind upward subplatysmal dissection, use of a plane where the marginal branch of the facial nerve is easily endangered in combination with a low skin incision (3–4 cm under the lower mandibular border), and a location far from the fracture line that requires strong retraction of soft tissue containing facial nerve branches. The marginal mandibular branch can be identified easily without considerable dissection; if a flap, including the nerve, is elevated, there remains some risk for facial nerve damage. Kanno et al. first reported the use of a modified technique for elevating the skin-muscle flap without requiring identification of the facial nerve, resulting in a low rate of complications [ 33]. Specifically, only one patient (4.2%) developed short-term transient temporary facial nerve weakness of the marginal mandibular branch. Salivary fistulae, paresthesia, hematoma, and infection have also been reported as surgical complications, but their incidences are low [ 14, 28, 33]. However, this approach exposes less of the mandibular ramus and condyle. Most surgeons agree that it yields insufficient exposure and to secure instrumentation working space to condylar fractures [ 12- 14, 33]. Therefore, if ORIF is impossible with only the classic submandibular approach to medium to higher condylar fractures (e.g., condylar neck fractures), a transbuccal trocar combined with the submandibular approach is required [ 12, 33].
High-submandibular (high-perimandibular, modified Risdon, angular subparotid) approach
Following the progressive development of a dedicated osteosynthesis plate system, together with a detailed biomechanical study involving double buttress biomechanical distribution at the mandibular condyle and placement over the lateral cortical bone without exposing the lower mandibular border, Meyer et al. described a variation of the classic submandibular approach in 2006 ( Fig. 3B) [ 9, 10]. He called this innovative modified submandibular approach, the high-submandibular approach [ 10]. This approach is known as the high-perimandibular approach by the Japanese Society of Oral and Maxillofacial Surgeons and has also been introduced as the modified Risdon or angular subparotid approach [ 34, 35]. It is relatively easy and quick compared to other extraoral cutaneous approaches. It allows contact with all condylar base fractures and most condylar neck fractures located at least 1 cm below the top of the condylar head, as described by Meyer et al [ 36]. The mandibular angle is drawn and the skin incision is traced (approximately 4 cm in length) approximatively 1 cm under this angle in the uppermost natural cervical crease. The main modifications are a higher skin incision, location near the fracture line, and plane-by-plane dissection of muscular layers, which allow easy verification and preservation of facial nerve branches with consideration of marginal mandibular and buccal branches [ 36]. Briefly, after the incision is made, the platysma muscle is identified between cutaneous edges. An upward dissection is initiated in a strict subcutaneous plane, preserving the underlying platysma muscle. The subcutaneous dissection is continued 2–3 cm above the lower border of the angle. The platysma is then grasped between pliers at the highest level of the dissection, lifted, and cut obliquely toward the ear lobe, exposing the underlying masseter muscle. Care is taken at this step to preserve the superficial fascia covering the masseter, because a branch of the facial nerve (typically the buccal branch) may be observed running horizontally under this fascia. The facial nerve branches, lying one plane deeper, remain fully protected at this stage. The masseter is divided horizontally (over the facial nerve branch, if visible) in a single incision with a sharp scissors. This incision is completed (mainly backward) obliquely toward the earlobe. The goal is close contact with the fracture line and exposure of the posterior border of the ramus, which will aid in verification of condylar fragment reposition. The dissection is continued upward in the sub-periosteal plane and the condylar fragment is exposed. Use of this method drastically reduces the rate of facial nerve complications to near zero [ 14, 28, 35, 36]. The first systematic review and meta-analysis regarding the rate of facial nerve injury when performing ORIF of mandibular condylar fractures revealed that, when limited to ORIF of condylar base fractures, high-submandibular incisions with the transmasseteric anteroparotid approach as described here are the safest approach [ 14, 28, 35, 36]. Note that no cases of facial nerve weakness have been reported. Unfortunately, this first publication was in French [ 36]. Thus, this high-submandibular approach has often been confused with other submandibular or periangular approaches, with differences in deep dissection planes.
Concerning complications, Meyer et al. reported that 2.2% of patients exhibited transient facial nerve weakness and no patients exhibited permanent palsy in a retrospective clinical study of 434 patients and 496 approaches (including 21.2% condylar neck fractures and 78.8% condylar base fractures) [ 36]. Complications linked to this approach included 11 patients (2.2%) with temporary (0 definitive) palsy of the facial nerve, one patient (0.2%) with hematoma requiring revision, and one patient (0.2%) with abscess requiring revision. Scarring was hypertrophic or unaesthetic in five patients (1%). These safe surgical approaches with very low rates of complications have rapidly gained in popularity among surgeons and in our institute [ 34- 36]. Further clinical studies are under way to elucidate clinical feasibility with longer follow-up periods, because this newest extraoral approach to open treatment of mandibular condylar fractures predominates among surgeons. Although Meyer et al. described its applicability up to 1 cm under the top of the condylar head, the safest application in ORIF of mandibular condylar fractures could be from condylar base fractures to most condylar neck fractures [ 36]. Clinical results are promising and consistent with our most recent preferred extraoral approach.
Treating mandibular condylar process fractures has long been controversial [ 37]. Historically, such fractures have been treated by closed reduction, which produces relatively acceptable outcomes in most patients [ 6, 8, 38]. Until the late 20th century, open treatment using ORIF was considered hazardous, in particular with respect to facial nerve injury and extraoral facial scarring, because of the complex regional anatomy [ 7, 13, 37, 38]. Furthermore, before plate and screw fixation was introduced and well established, open reduction involved the placement of an interosseous wire to stabilize the reduced segments and required additional periods of maxillomandibular fixation to immobilize segments and permit osseous union [ 1- 3, 37]. Therefore, the value of open reduction was the subject of considerable debate.
After the development of rigid fixation permitted open reduction and stable internal fixation of mandibular condylar fractures without the requirement for postoperative maxillomandibular fixation, and understanding of the biomechanics of the temporomandibular joint and functional mechanics of the mandibular condyle improved, open reduction received renewed interest [ 37- 39]. Surgical treatment of condylar fractures has increasingly become the standard because of technological advancements, the development of osteosynthesis devices, enhanced surgical techniques, and the introduction of feasible surgical approaches [ 39, 40]. These changes are related to a better understanding of detailed surgical anatomy and may be further supported by additional clinical data. ORIF can clearly provide superior oral and maxillofacial functional outcomes with more rapid rehabilitation of oromandibular function and reintegration into social activity, according to subjective and objective comparisons to conservative treatment [ 37- 41]. The development of a safe surgical approach is necessary for first-line treatment of trauma patients with mandibular condylar fractures.
An appropriate surgical approach is the first step in avoiding complications associated with the procedure, such as facial nerve injuries, facial scarring, and massive bleeding. Any surgical approach chosen must provide direct visualization of the fractured segment, adequate accessibility for reduction and the placement of fixation materials, and minimal invasiveness with few postoperative complications [ 37- 41]. The choice of surgical approach for reaching a mandibular condylar fracture depends mainly on the location, type and mode of fracture [ 12, 13]. Several important anatomical structures must also be considered, including nerves, blood vessels, and the parotid gland. However, to the best of our knowledge, the optimal surgical approach for treating mandibular condylar fractures remains the subject of debate. Although ORIF of mandibular condylar fractures may be nonhazardous, outcomes of both open and closed treatments have received considerable criticism [ 36- 38]. There remains a lack of established, evidence-based treatment strategies. Surgical complications remain the major limitation of open treatment of ORIF. A better definition of the most appropriate approach and knowledge of the exact risks for specific complications are essential in the decision-making process, as several surgical approaches have been advocated, each with potential complications, as described in this review [ 36- 41].
The fact that fractures, approaches, and surgical techniques are so diverse makes it difficult to generate an objective, clear, and useful comparison of surgical techniques for treating condylar fractures and their complications. Regarding the open treatment of mandibular condylar fractures, some pioneering surgeons have described the basic clinical flow of open treatment surgery for mandibular condylar fractures, considering limited available surgical guidelines and review studies [ 28, 37, 38]. Our present surgical treatment algorithm regarding surgical approaches follows the recommendations of the most current surgical literature, including our accumulated clinical and basic studies in the field of open treatment of mandibular condylar fractures ( Fig. 4) [ 1- 4, 30, 31, 33]. Further studies are needed to establish additional evidence regarding the best surgical approaches to open treatment. These studies should focus on the similarities and differences in extraoral approaches, various modifications, novel endoscopic techniques that advanced and less technically demanding, the monitoring of nerve integrity during surgery, intraoperative surgical navigation, and intraoperative radiographic evaluation (e.g., cone beam computed tomography) [ 40- 42]. In this way, an evidence-based protocol for treating complex mandibular condylar fractures can be created in the near future.
In conclusion, a clearer treatment protocol is needed to achieve predictable clinical practice, in particular in terms of surgical approach in our opinion. In cases of open treatment of ORIF of mandibular condylar fractures, this protocol should be interpreted and implemented with consideration of the surgeon’s skills. Based on the literature summarized in this review, we hope to propose a protocol for open treatment of mandibular condylar fractures, including surgical approaches, through a large, collaborative multicenter clinical safety study to address the demands of both surgeons and patients.
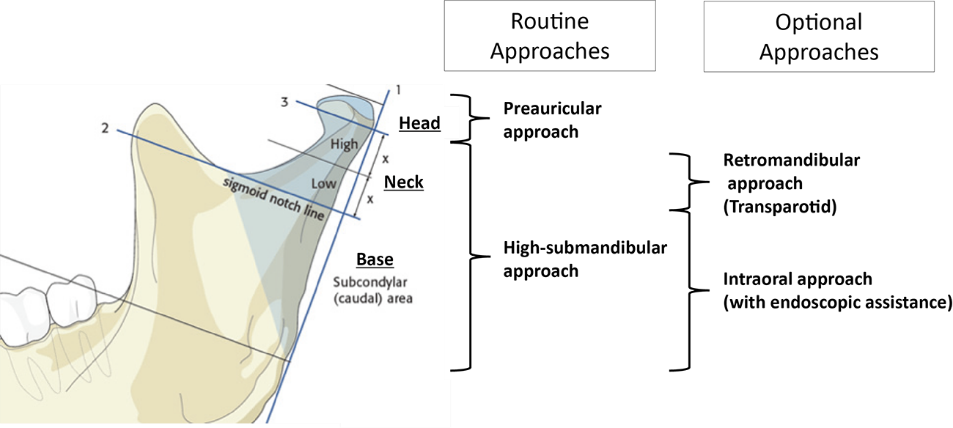
Schematic diagram of our current routine surgical approach methods of accessing fractured mandibular condylar processes to perform ORIF. Source: https://surgeryreference.aofoundation.org/cmf/trauma/ (Accessed June 29, 2020).
Conflict of interest
The authors declare no conflicts of interest.