Abstract
The purpose of this study was to clarify the effects of preoperative inpatient rehabilitation on the incidence of postoperative pneumonia and length of hospital stay in patients with esophageal cancer. Twenty patients were requested for inpatient rehabilitation one week before surgery and 13 patients were used as historical control. The training consisted of respiratory muscle training, lower limb strength training, and aerobic exercise for one hour each in the morning and afternoon for one week. Outcomes are including the length of hospital stay and incidence of postoperative pneumonia. Postoperative hospital stay was 21 days for the intervention group and 35 days for the control group (p = 0.001), and the total length of hospital stay was 28.5 days and 37 days, respectively (p = 0.01). However, the incidence of postoperative pneumonia was 45% and 53.8%, respectively (p = 0.62). Inpatient preoperative rehabilitation for one week is a beneficial measure because it can decrease the hospital stay without adverse events.
INTRODUCTION
Esophageal cancer surgery is highly invasive and is accompanied with many postoperative complications, and postoperative pneumonia in particular affects the length of stay in the hospital [1]. Although the effectiveness of preoperative rehabilitation (prehabilitation) has been reported by a systematic review [2], it is often difficult to continue outpatient rehabilitation from 1–3 months in advance, both temporally and socially, and the merit of intensive rehabilitation in the short period before surgery is considered to be advantageous. According to Tajima et al. of Wakayama Prefectural Medical University, he reported good results through intensive rehabilitation by hospitalization for one week before surgery [3].
Therefore, since September 2018, our hospital has also introduced preoperative intensive rehabilitation to prevent postoperative complications. Although it can be said that inpatient rehabilitation for one week before surgery is contrary to the trend of the modern medical care system aiming to shorten the number of days of hospitalization, it is acceptable medical care if the occurrence of postoperative complications can be suppressed and the postoperative hospitalization period can be shortened. Training for one week before surgery after hospitalization is recognized as respiratory rehabilitation covered by health insurance.
According to cancer rehabilitation guidelines compiled by the Japanese Society of Rehabilitation Medicine in 2019 [4], only weak recommendations were made for rehabilitation, including preoperative respiratory rehabilitation. The reasons for this were the small number of patients, uneven content of treatment, and lack of research that provided strong evidence in Japan.
The purpose of this study is to clarify the effectiveness of preoperative intensive rehabilitation for the patients with esophageal cancer by comparing the effects of historical controls prior to the introduction of intensive rehabilitation in our hospital.
PATIENTS AND METHODS
Patients
The subjects were 20 patients (18 men and 2 women, mean age 68.8 years) who underwent intensive inpatient rehabilitation at Shimane University Hospital for one week prior to esophageal cancer surgery between September 2018 and December 2020. As a control, 13 patients (8 men and 5 women, mean age 65.7 years) who underwent esophageal cancer surgery between September 2014 and August 2018 were selected.
Inclusion criteria included that the patient’s performance status was 0 to 2 and that there were no severe circulatory or respiratory dysfunction that would interfere with performing light exercise. Exclusion criteria included patients with suture failure and patients with difficulty exercising due to metastatic bone tumors. Although suture failure is one of the serious postoperative complications, suture failure is influenced by the surgeon’s experience and learning curve, and once it occurs, it greatly affects the duration of postoperative hospitalization, so cases of suture failure were excluded.
Surgical methods
As for the surgical method, thoracoscopic surgery was performed in all cases. Fifty percent of patients in the intensive rehabilitation group had robotic assisted surgery (Da Vinci surgery), but none in the control group.
Outcome measure
The basic survey items were age, sex, body mass index (BMI), preoperative serum albumin, preoperative hemoglobin, preoperative respiratory function (% forced vital capacity (%FVC) and % forced expiratory volume for 1 second (FEV1%)), smoking history, preoperative chemotherapy, preoperative comorbidities, esophageal cancer staging [5], esophageal cancer development sites, and reconstruction pathways. Preoperative hemoglobin, serumalbumin, and respiratory function were measured before prehabilitation. Main outcome measures were the postoperative hospitalization period and the total hospitalization period. Secondary outcome measures were the incidence of postoperative pneumonia, defined by Clavien-Dindo classification [6] of grade II or higher, and changes in the 6-minute walking distance in the intensive rehabilitation group. The walking distance for 6 minutes was assessed at the time of admission and immediately before surgery.
Preoperative intervention
Preoperative intensive rehabilitation consisted of three parts: inspiratory muscle training using incentive spirometry, strength training using a leg press machine, and aerobic exercise using an exercise bike. Inspiratory muscle training was performed 30 times in two sets using Threshold IMT® (Philips, NV, USA) at 30% of maximum inspiratory muscle strength. For leg strength training, a leg press machine (Weltonic®, MINATO, Osaka, Japan) was used and 2 sets of training were performed 30 times at 60% of maximum strength. Aerobic exercise with an exercise bike was performed for 30 minutes at a conscious intensity of Borg scale 11–13 using two motorcycles (Aerobike 2100R®, Konami, Kanagawa, Japan, and Cordless Bike V65Ri®, Senoh, Chiba, Japan). These three types of training were continued for one hour each in the morning and afternoon for a week.
Postoperative intervention
In postoperative rehabilitation, a physical therapist started pulmonary rehabilitation and sedentary training at the bedside of the ICU from the day after surgery, and shifted to standing and walking training while paying attention to the general condition.
Statistical analysis
Statistical analysis was performed using Mann-Whitney U test, and Chi-square test in BellCurve for Excel® ver.2.0 (SSRI Co., Ltd. Tokyo, Japan) and statistical significance was accepted for values of p < 0.05. Non-parametric continuous variables were reported as median and standard deviation and compared using the Mann-Whitney U test. Categorical variables were compared using Fischer’s exact test.
RESULTS
The basic characteristics of the patients were shown in Table 1 (Table 1). There was no significant difference between the intervention group and the control group in terms of age at the time of surgery. There was no significant difference between two groups for gender, BMI, preoperative serum albumin, preoperative hemoglobin, preoperative % vital capacity, and preoperative forced expiratory volume in 1 second (Table 1). Smoking history was significantly higher in the intervention group (p = 0.001), and preoperative chemotherapy was also significantly higher in the intervention group (p = 0.001).
Preoperative comorbidities were shown in Table 2 (Table 2), with some patients in the intervention group having mild restrictive ventilatory compromise and chronic bronchitis.
Esophageal cancer staging was shown in Table 3 (Table 3) and no significant difference was observed between the intervention and control groups. The sites of esophageal cancer development were shown in Table 4 (Table 4), and no significant difference was observed between the two groups. Reconstruction pathways were shown in Table 5 (Table 5), and no significant difference was observed between the two groups.
The number of preoperative training sessions in the intervention group was 7.2 ± 1.0 times (minimum 4 times, maximum 11 times), and variations were observed. There were no cases of dropout.
In the intervention group, when comparing the six-minute walking distance at the time of admission and immediately before surgery, there was a significant increase from 493 m to 522 m (p = 0.008).
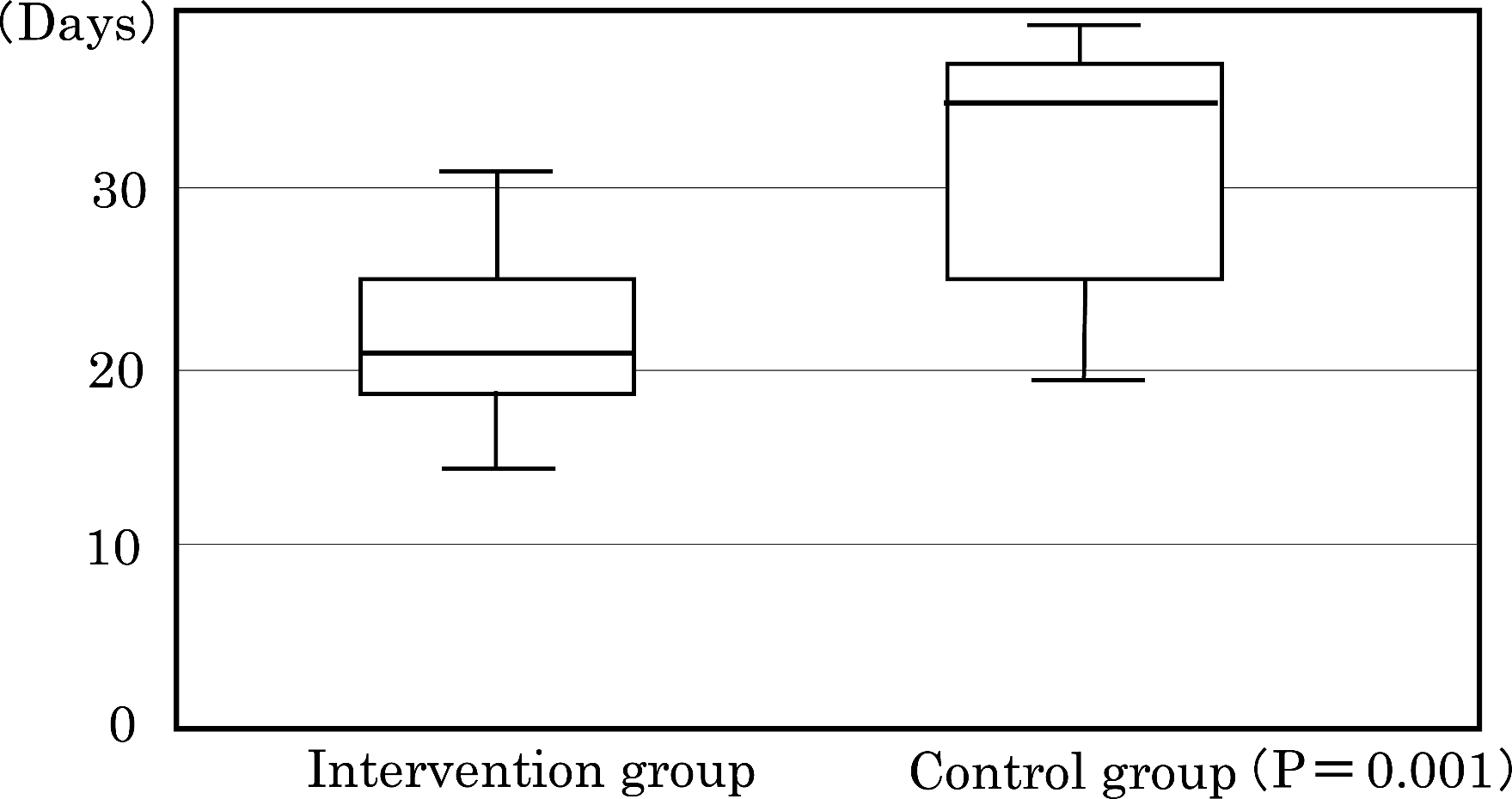
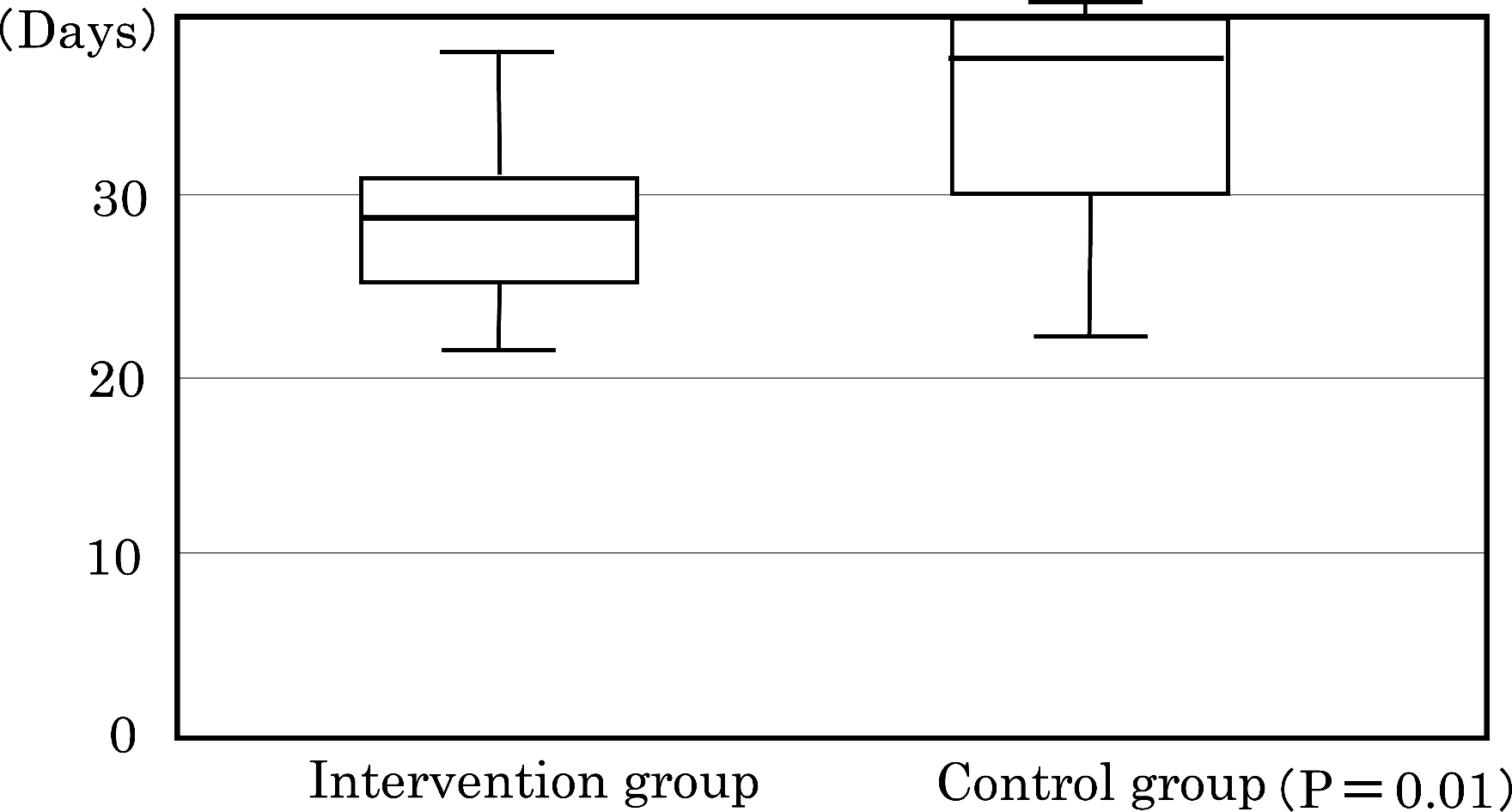
The duration of postoperative hospitalization was 21 days in the intervention group and 35 days in the control group, and was shortened by about 2 weeks in the former (p = 0.001) (Figure 1). The total length of hospitalization was 28.5 days in the intervention group and 37 days in the control group, which was reduced by about 9 days in the former (p = 0.01) (Figure 2).
The incidence of postoperative pneumonia was 9 of 20 (45%) in the intervention group and 7 of 13 (53.8%) in the control group, with the control group tending to be slightly more likely but not significantly different (p = 0.619) (Table 6).
Table 1. Patient characteristics
|
Intervention group (n = 20) |
Control group (n = 13) |
p value |
| Age at operation (years) |
68.8 ± 6.7 |
65.7 ± 7.6 |
0.56 |
| Gender (male / female) |
18 / 2 |
8 / 5 |
0.08 |
| BMI (kg/m2) |
20.6 ± 2.1 |
20.9 ± 2.5 |
0.79 |
| Preoperative albumine (g/dL) |
3.67 ± 0.44 |
3.96 ± 0.48 |
0.08 |
| Preoperative hemoglobin (mg/dL) |
11.7 ± 1.4 |
12.1 ± 2.0 |
0.48 |
| Preoperative %FVC (%) |
98.0 ± 12.9 |
100.3 ± 12.6 |
0.45 |
| Preoperative FEV% (%) |
73.3 ± 7.8 |
77.0 ± 9.5 |
0.21 |
| Smoking history (yes / no) |
15 / 5 |
9 / 4 |
0.001 |
| Preoperative chemotherapy (yes / no) |
15 / 5 |
2 / 11 |
0.001 |
Data are shown as mean ± standard deviation. Preoperative hemoglobin, serum albumin, and respiratory function are measured before prehabilitation.
Table 2. Preoperative comorbidity
|
Intervention group (n = 20) |
Control group (n = 13) |
| Hypertension |
4 |
2 |
| Diabetes mellitus |
3 |
3 |
| Restrictive lung disease |
1 |
0 |
| Chronic bronchitis |
1 |
0 |
| Chronic kidney disease |
1 |
0 |
| Thrombocytopenia |
1 |
0 |
| Iron deficiency anemia |
0 |
1 |
| Atrial fibrillation |
0 |
1 |
| Atrioventricular block |
0 |
1 |
Table 3. Stage of esophageal cancer
|
Intervention group (n = 20) |
Control group (n = 13) |
| Stage 0 |
0 |
1 |
| Stage I |
3 |
4 |
| Stage II |
5 |
0 |
| Stage III |
10 |
7 |
| Stage IVa |
2 |
1 |
| Stage IVb |
0 |
0 |
(P = 0.84)
Table 4. Location of esophageal cancer
|
Intervention group (n = 20) |
Control group (n = 13) |
| Upper |
2 (10%) |
1 (7.7%) |
| Middle |
10 (50%) |
7 (53.8%) |
| Lower |
8 (40%) |
5 (38.5%) |
(P = 1.00)
Table 5. Route of reconstruction
|
Intervention group (n = 20) |
Control group (n = 13) |
| Mediastinal |
20 (100%) |
12 (92.3%) |
| Retrosternal |
0 (0%) |
1 (7.7%) |
(P = 0.94)
Table 6. Rate of postoperative pneumonia (Severe than Clavien-Dindo stage II)
|
Intervention group (n=20) |
Control group (n=13) |
| Pneumonia (+) |
9 (45%) |
7 (53.8%) |
| Pneumonia (-) |
11 (55%) |
6 (46.2%) |
(P = 0.62)
The incidence of postoperative pneumonia was 9 of 20 (45%) in the intervention group and 7 of 13 (53.8%) in the control group (p = 0.619).
DISCUSSION
In our study, inpatient intensive preoperative rehabilitation (1 hour each in the morning and afternoon, 2 hours a day, for a week) consisting of aerobic exercise, leg strength training, and inspiratory muscle training significantly reduced hospital stays. Even though patients had been hospitalized for an extra seven days before surgery, their total stay could have been shortened by another nine days by our modest protocol. The training time was shorter than the other facility [3], and it was a highly feasible program with no dropouts, and a great effect was obtained with the minimum necessary effort.
The problem is that the average number of preoperative rehabilitations is 7.2 (the expected number is 10), which is less than planned. These changes in the rehabilitation schedule of patients were due to examinations and the like. Previous reports [3,7] have not provided clear evidence of a correlation between the intensity and amount of exercise therapy and its beneficial effects. In a multicenter study across four European countries on the effects of preoperative pulmonary rehabilitation [8], the exercise improved inspiratory muscle strength and endurance. However, the incidence of postoperative pneumonia was not significantly different between the intervention and control groups. This may be due to the fact that this RCT study was conducted on outpatient home exercises and that only respiratory muscle training was performed, no aerobic or strength training. Comprehensive rehabilitation during hospitalization is considered to be effective, but in other countries, there are restrictions on medical treatment covered by insurance, and it is a special type of rehabilitation that can only be performed in Japan. According to a recent systematic review of prehabilitation in patients with esophageal cancer, the optimal protocol has not been clarified [9]. For patients with physical problems, a program that provides maximum effect with minimal load is appropriate, and it is necessary to clarify the optimal training content in the future.
In our study, the incidence of postoperative pneumonia was 45% in the intervention group and 53.8% in the control group, and this result was slightly higher compared to previous reports (40–60%) [10,11]. Although it was difficult to significantly reduce the incidence of pneumonia through our inpatient intensive rehabilitation, we were able to significantly shorten the length of hospital stay. This suggests that our intervention prevented the occurrence of severe postoperative pneumonia that affected the length of hospital stay. The Clavien-Dindo classification was used to assess postoperative pulmonary complications, but it was a rough classification, making it difficult to assess the severity of pneumonia. By using the Utrecht scoring system [12], it is possible to qualitatively evaluate the severity of pneumonia and to determine the effect of preoperative rehabilitation in detail.
With prolonged exercise, skeletal muscle produces Interleukin-6 (IL-6) and releases it into the circulation [13]. IL-6 is one kind of myokine, a kind of cytokine with anti-inflammatory properties, and other known myokines include IL-8, IL-5, and brain derived growth factor (BDNF) [14]. It is thought that exercise-induced myokine inhibits postoperative inflammation, improves glucose, fat and muscle metabolism, and suppresses the occurrence of complications in postoperative patients. Since we have not quantified myokines, we cannot prove a direct causal relationship, but it is thought that the length of hospitalization was shortened by the effect of myokine, which was increased by exercise.
Studies conducted in young men have shown that five days of aerobic exercise and proper diet intake increase plasma volume [15]. Even in middle-aged and elderly patients, aerobic exercise while regularly eating hospital meals may have increased plasma volume. We could not prove this because we have not measured circulating blood volume, but this may have contributed to the reduction of postoperative complications and the promotion of recovery.
Study limitations
This study was conducted in a single institution, and the low number of cases and the use of historical controls are limitations of this study.
Since the study is retrospective with a historical patient and the research period is long, the second limitation is that it is influenced by newly introduced treatments for the treatment of esophageal cancer. For example, the number of patients receiving preoperative chemotherapy has increased, and the share of robot-assisted surgery (Da Vinci surgery) has also increased. As a result, patient backgrounds are different, and it has become difficult to simply compare the effects of preoperative intensive rehabilitation.
The third limitation in this study was the exclusion of patients with suture insufficiency. Suture failure is important as a postoperative complication, but it is greatly influenced by the learning curve of the surgeon’s skill acquisition, so it was excluded to eliminate its influence.
The fourth problem is that there is a difference in smoking history between the two groups, the certainty of smoking cessation before surgery has not been confirmed, and the Brinkman index could not be examined. Smoking cessation for more than two months has been reported to improve short-term outcomes after esophageal cancer surgery, as well as improve prognosis for patients with locally advanced cancer [16].
The last problem is sarcopenia. Sarcopenia, defined as a condition of low muscle mass and strength, is known to adversely affect postoperative outcomes in cancer patients. According to a report examining the association between easily measurable handgrip strength and postoperative pneumonia, a significant association was found by multivariate analysis [17]. Further studies are needed to improve postoperative outcomes and survival rates by treating sarcopenia preoperatively.
CONCLUSIONS
In patients with esophageal cancer, intensive inpatient rehabilitation was performed one week before surgery, and the postoperative hospitalization period was reduced by about 14 days, and the total hospitalization period was also reduced by about 9 days. However, there was no significant improvement in the incidence of postoperative pneumonia. Our prehabilitation is a beneficial measure because it is covered by health insurance and because the participating patients did not drop out nor developed adverse events.
Ethical Approval
This study was conducted in accordance with the principles of the Declaration of Helsinki and the Good Clinical Practice Guidelines. This study was also conducted with the approval of the Shimane University School of Medicine and the Medical Ethics Committee (Accreditation No. 5272).
All participants provided written informed consent.
Authors Contribution
All authors contributed to the study conception, and data collection and analysis were performed by Sho Fukuhara and Yuki Hara. The first draft of the manuscript was written by Sokichi Maniwa and all authors commented on the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors wish to acknowledge Dr. Yoshitsugu Tajima, Professor of Digestive and General Surgery, and Dr. Noriyuki Hirahara, Associate Professor of Digestive and General Surgery, Shimane University Faculty of Medicine, for their instruction and cooperation.
Funding
No research funds were used for this study.
Conflict of interest
All authors confirm that there are no conflicts of interest to declare.
REFERENCES
- 1) van Egmond MA, van der Schaaf M, Klinkenbijl JH, Engelbert RH, van Berge Henegouwen MI. Preoperative functional status is not associated with postoperative surgical complications in low risk patients undergoing esophagectomy. Dis Esophagus 2017;30:1-7. doi: 10.1111/dote.12469.
- 2) Bolger JC, Loughney L, Tully R, et al. Perioperative prehabilitation and rehabilitation in esophagogastric malignancies: a systematic review. Dis Esophagus 2019;32:1-11. doi: 10.1093/dote/doz058.
- 3) Kitahata Y, Hirono S, Kawai M, et al. Intensive perioperative rehabilitation improves surgical outcomes after pancreaticoduodenectomy. Langenbecks Arch Surg 2018;403:711-718. doi: 10.1007/s00423-018-1710-1.
- 4)
Japanese Society of Rehabilitation Medicine. Gastrointestinal Cancer. In: Japanese Society of Rehabilitation Medicine. Guidelines for Cancer Rehabilitation. 2nd ed. Tokyo: KANEHARA & CO., LTD.; 2019:28-37. (in Japanese)
- 5)
Japan Esophageal Society. Clinical Findings. In: Japan Esophageal Society. Japanese Classification of Esophageal Cancer. 11th Ed. Tokyo: KANEHARA & CO., LTD.; 2015:6-21. (in Japanese)
- 6) Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-196. doi: 10.1097/SLA.0b013e3181b13ca2.
- 7) Yamana I, Takeno S, Hashimoto T, et al. Randomized controlled study to evaluate the efficacy of a preoperative respiratory rehabilitation program to prevent postoperative pulmonary complications after esophagectomy. Dig Surg 2015;32:331-337. doi: 10.1159/000434758.
- 8) Valkenet K, Trappenburg JCA, Ruurda JP, et al. Multicentre randomized clinical trial of inspiratory muscle training versus usual care before surgery for oesophageal cancer. Br J Surg 2018;105:502-511. doi: 10.1002/bjs.10803.
- 9) Piraux E, Reychler G, de Noordhout LM, et al. What are the impact and the optimal design of a physical prehabilitation program in patients with esophagogastric cancer awaiting surgery? A systematic review. BMC Sports Sci Med Rehabil 2021;13:33. doi: 10.1186/s13102-021-00260-w.
- 10) Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-1892. doi: 10.1016/S0140-6736(12)60516-9.
- 11) Blencowe NS, Strong S, McNair AG, et al. Reporting of short-term clinical outcomes after esophagectomy: a systematic review. Ann Surg 2012;255:658-66. doi: 10.1097/SLA.0b013e3182480a6a.
- 12) van der Sluis PC, Verhage RJ, van der Horst S, et al. A new clinical scoring system to define pneumonia following esophagectomy for cancer. Dig Surg 2014;31:108-116. doi: 10.1159/000357350.
- 13) Muñoz-Cánoves P, Scheele C, Pedersen BK, Serrano AL. Interleukin-6 myokine signaling in skeletal muscle: a double-edged sword? FEBS J 2013;280:4131-4148. doi: 10.1111/febs.12338.
- 14) Aryana IGPS, Hapsari AAAR, Kuswardhani RAT. Myokine regulation as marker of sarcopenia in elderly. Molecular and Cellular Biomedical Sciences 2018;2:38-47. doi: 10.21705/mcbs.v2i2.32.
- 15) Goto M, Okazaki K, Kamijo Y, et al. Protein and carbohydrate supplementation during 5-day aerobic training enhanced plasma volume expansion and thermoregulatory adaptation in young men. J Appl physiol (1985) 2010;109:1247-1255. doi: 10.1152/japplphysiol.00577.2010.
- 16) Yoshida N, Eto K, Horinouchi T, et al. Preoperative smoking cessation and prognosis after curative esophagectomy for esophageal cancer: a cross-sectional study. Ann Surg Oncol 2022;29:8172-8180. doi: 10.1245/s10434-022-12433-z.
- 17) Kurita D, Oguma J, Ishiyama K, et al. Handgrip strength predicts postoperative pneumonia after thoracoscopic-laparoscopic esophagectomy for patients with esophageal cancer. Ann Surg Oncol 2020;27:3173-3181. doi: 10.1245/s10434-020-08520-8.