2023 年 40 巻 1-2 号 p. 23-29
2023 年 40 巻 1-2 号 p. 23-29
Background: The aim of this randomized controlled study was to compare the effects of ultrasound-guided erector spinal block (ESPB) with those of opioid-based analgesia. Methods: This prospective, randomized, open, blinded-endpoint study evaluated the analgesic effects of ESPB in patients undergoing lumbar surgery. The outcome measures were remifentanil and propofol consumption during operation, fentanyl consumption during 24 hours after anesthesia induction. Results: Data from fifteen patients were analyzed with seven and eight patients in the control and ESPB groups, respectively. There was difference between the groups in remifentanil consumption (median μg/kg lean body mass) 44.1 [37.1, 49.3] and 22.4 [17.3, 26.1]; p = 0.002 in control and ESPB groups during operation. There was no difference between the groups regarding other outcomes including fentanyl consumption for postoperative analgesia. Conclusions: ESPB reduced remifentanil consumption during operation, but did not reduce fentanyl consumption for postoperative analgesia within 24 hours after anesthesia induction in lumbar spine surgery.
Adequate postoperative pain control can result in faster recovery from surgery, fewer complications, and improved patient satisfaction during perioperative spine surgery [1]. Postoperative pain management in spine surgery relies heavily on opioids because of their excellent analgesic effects. However, nausea, vomiting, and itching are common opioid-related side effects, and respiratory depression may occur in rare but serious cases. Furthermore, opioid abuse has become a social problem in spine surgery in recent years [2,3,4].
A recent review recommended the use of multimodal analgesia, including peripheral nerve blocks, to minimize the use of opioids after spine surgery [5]. Erector spinae plane block (ESPB) was reported in 2016 as a new trunk interfascial plane block [6]. Theoretically, ESPB blocks the posterior branches of the spinal nerves and may reduce pain originating in the dominant regions [7]. In a systematic review and meta-analysis of ESPB for lumbar spine surgery, ESPB provided effective postoperative analgesia resulting in better patient satisfaction and recovery with decreased postoperative nausea and vomiting in patients undergoing lumbar surgery compared to the control [8].
On the other hand, it has been reported that the analgesic effect of single-dose ESP is 6 to 8 hours after lumbar spine surgery [9]. The exact duration of the analgesic effect of single-dose ESP is unknown.
This prospective, randomized, open, blinded-endpoint study aimed to evaluate the analgesic effect of ESPB in patients undergoing lumbar surgery. The aim of this study was to compare the effects of ESPB with opioid-based analgesia (control) on intraoperative remifentanil consumption and postoperative fentanyl consumption and VAS score.
This was a prospective, randomized, open, blinded-endpoint study. Patients aged between 20 and 80 years in American Society of Anesthesiology (ASA) physical status I–III, who were scheduled for lumbar spine surgery were included in the study. The exclusion criteria were emergency surgery for same-day application, spinal fusion surgery, and surgery for more than 4 vertebrae. Patients with a history of lumbar spine surgery were also excluded. The study protocol was approved by the Shimane University Institutional Committee on Ethics Evaluation Form Regarding the Research Proposal (20181108-1) on January/18/2019. The study was conducted in accordance with the provisions of the Declaration of Helsinki and the International Conference on Harmonisation Guidelines for Good Clinical Practice. All patients provided written informed consent before study entry. The date of patient enrollment was 3/3/2019. The trial registration number is UMIN000035698. The link to our registration documents was https://center6.umin.ac.jp/cgi-openbin/ctr/ctr_view.cgi?recptno=R000040660.
Eligible patients were randomly assigned to either the ESPB or control group using simple fixed allocation randomization. The randomization sequence was generated by a statistician. Patients and anesthesiologist were not blinded to the group assignments; however, the evaluators were.
Patients were placed in the prone position to perform ESPB before general anesthesia.
The puncture level was determined according to the surgical site: at that level for one intervertebral, at either for two intervertebral, and in the middle for three intervertebral.
First, we identified the right or left transverse process on ultrasound after placing a transducer (15–6 Hz, FUJIFILM SonoSite, Japan) in the longitudinal plane. The needle was inserted in-plane, and we administered 1.5 mg/kg (up to 75 mg) of 0.5% levobupivacaine. We observed linear fluid spreading deep into the erector spinae muscle. We then performed the same ESPB procedure on the opposite side. Thus, we administered a total of 3.0 mg/kg (up to 150 mg) levobupivacaine.
Before anesthesia induction or ESPB, we administered 1 mg midazolam and 1 μg/kg (lean body mass) fentanyl intravenously. General anesthesia induction was achieved by administering 1–2 mg/kg propofol, 1 μg/kg (lean body mass) fentanyl, and 0.6–0.9 mg/kg rocuronium. Pulse oximetry, electrocardiography, non-invasive blood pressure (NIBP), end-tidal carbon dioxide measurement, neuromuscular monitoring to derive train-of-four (TOF) ratio values, and the bispectral index (BIS) was monitored during anesthesia maintenance. General anesthesia was maintained with propofol and remifentanil continuously, and a single shot of rocuronium as appropriate so that the BIS maintained a range of 40–60 and TOF ratio <2/4. At the end of surgery, 15 mg/kg (up to 1000 mg) Acetaminophen was administered intravenously for postoperative analgesia, 1.25 mg droperidol was administered intravenously to prevent postoperative nausea and vomiting, and neuromuscular reversal occurred with 1–2 mg/kg of sugamadex administered intravenously. All patients were given patient-controlled analgesia (PCA) devices, set to deliver a 0.5 mg/kg (lean body mass) bolus dose of fentanyl, with a 10-minute lockout time. In addition, a rescue dose of acetaminophen and NSAIDs was available. VAS score at 6, 12, and 24 hours after anesthesia induction was recorded, as well as the incidence of nausea, vomiting, total fentanyl consumption during the 24 hours period after anesthesia induction. An anesthesiologist, masked to the study groups, was responsible for postoperative follow-up.
The outcomes were remifentanil and propofol consumptions during the operation, fentanyl consumption at 6, 12, and 24 hours after anesthesia induction, total fentanyl consumption for 24 hours after anesthesia induction, VAS score at 6, 12 and 24 hours after anesthesia induction, time of first rescue dose after surgery, incidence of side effects (nausea, vomiting, itching, and respiratory depression: < 10 breaths/min) at 6, 12 and 24 hours after anesthesia induction.
In preliminary cases in our hospital, the mean use of fentanyl 24 hours after anesthesia was 50% less in patients who received ESPB compared to patients who received only general anesthesia. The standard deviation was assumed to be 30 μg. With 80% power and an error of 0.05, the sample size necessary to detect a difference in postoperative fentanyl requirements at 24 hours, comparing the ESP group with the control group, was calculated as seven patients for each group. Ten patients were included in each group to compensate for potential dropouts. All analyses were performed in accordance with the protocol set. Fisher’s exact test was used to compare the categorical data. Continuous variables were summarized as medians and quartiles. Nonparametric methods were used, regardless of the distribution, to provide a robust comparison. Differences in continuous measurements were evaluated using the Mann-Whitney U test. All tests were two-sided, and P values less than 0.05 were considered to indicate statistical significance. All statistical analyses were performed using EZR [11] (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics. The findings from the study are described in accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines [12].
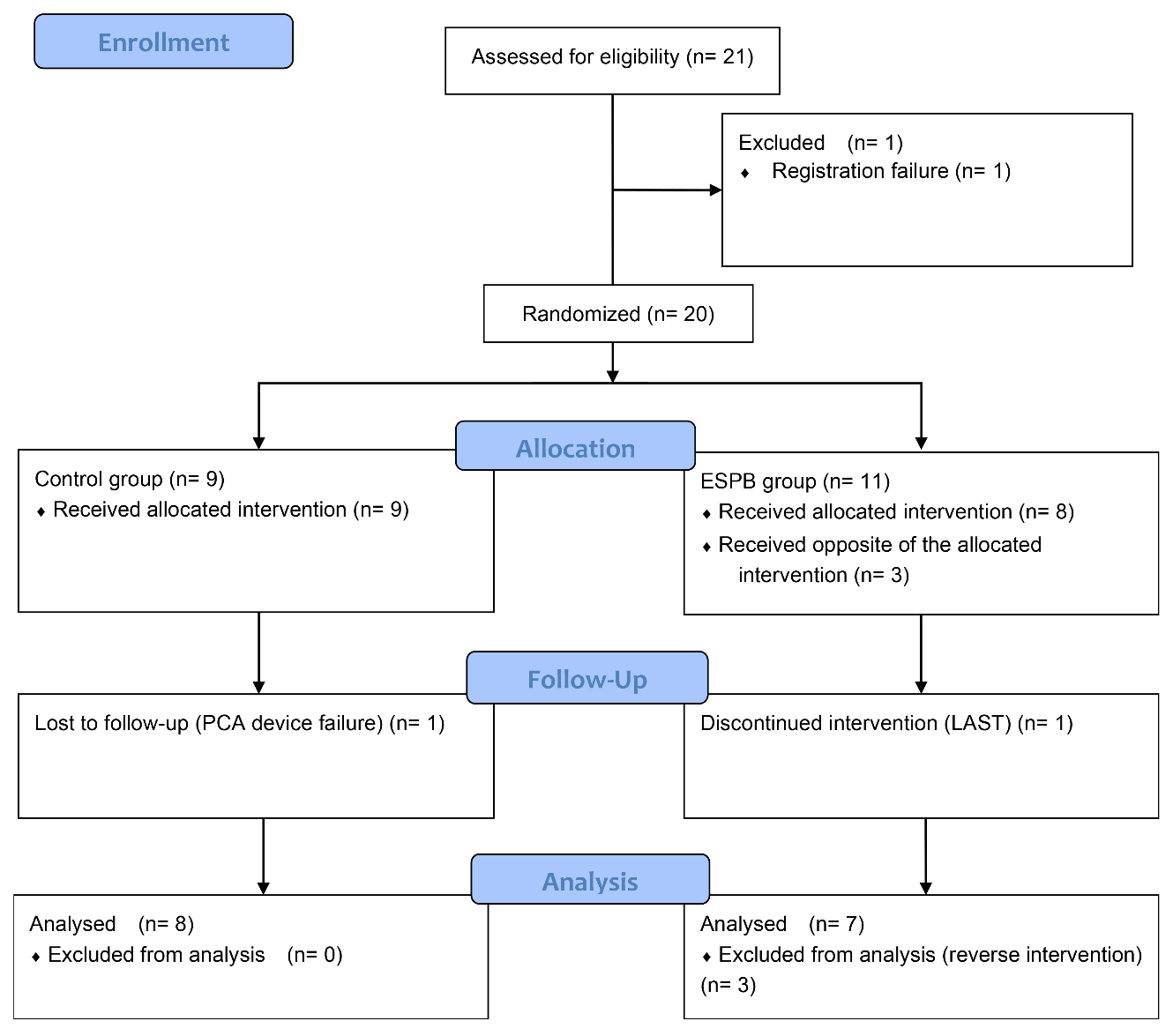
Twenty-one patients were enrolled in this study. One patient was excluded due to registration failure, resulting in twenty patients aged 35–79 years. All patients got surgery for lumbar spinal stenosis. Endoscopic laminoplasty or endoscopic laminectomy was performed, with surgical sites ranging from 1 to 3 in the control group and 1 to 2 in the ESPB group (Table 1). Nine and eleven patients were assigned to the control and ESPB groups, respectively. Three patients were excluded because they were incorrectly treated as part of the control group despite being assigned to the ESPB group. One patient was excluded because he suffered a disorder of consciousness and convulsions, which were suspected to be caused by local anesthetic systemic toxicity (LAST) 15 minutes after the block [16]. One patient was excluded because the PCA device was malfunctioning (Fig. 1).
The baseline characteristics were similar between the two groups, except for weight (Table 1). Remifentanil consumption (μg/kg lean body mass) during the operation in the ESPB group was significantly lower than that in the control group (22.4 [17.3, 26.1] vs. 44.1 [37.1, 49.3], p = 0.002), whereas all other outcomes did not differ between the two groups including fentanyl consumption for postoperative analgesia 24 hours after anesthesia induction between the groups (Table 2). The VAS score of ESPB group was half that of Control group at 10 minutes after extubation and 6 h after anesthesia induction, but this difference was not statistically significant (Figs. 2 and 3).
| Control group
(N = 8) |
ESPB group
(N = 7) |
P* | |
|---|---|---|---|
| Age median [quartile] | 70 [68, 77] | 70 [68, 73] | 1.000 |
| Male % (N) | 25% (2) | 71% (5) | 0.132 |
| Height (cm) median [quartile] | 153 [148, 161] | 162 [160, 167] | 0.152 |
| Weight (kg) median [quartile] | 56 [49, 66] | 74 [67, 79] | 0.021 |
| ASA-PS 2/3 (N) | 8/0 | 7/0 | |
| Opioid (Tramadol) use % (N) | 37.5% (3) | 28.5% (2) | 1.000 |
| Levels operated vertebrae median [quartile] | 1 [1, 2] | 2 [1,2] | 0.696 |
| Duration of surgery (min) median [quartile] | 195 [171, 215] | 155 [149, 180] | 0.397 |
| Duration of anesthesia (min) median [quartile] | 295 [258, 321] | 252 [224, 270] | 0.189 |
*Denotes the p-value based on the Mann-Whitney U test.
ESPB, erector spinae plane block
Notes: All date expressed as median [quartile].
ESPB, erector spinae plane block
PCA, patient controlled analgesia
LAST, local anesthetic systemic toxicity
| Control group
(N = 8) |
ESPB group
(N = 7) |
P* | |
|---|---|---|---|
| Remifentanil consumption (μg/kg lean body mass) | 44.1 [37.1, 49.3] | 22.4 [17.3, 26.1] | 0.002 |
| Propofol consumption (mg/kg) | 21.6 [19.2, 24.3] | 19.0 [15.1, 22.8] | 0.463 |
| Fentanyl consumption (μg/kg lean body mass)
6th h 12th h 24th h Total |
0.51 [0.50, 0.98] 0.50 [0.00, 0.99] 1.00 [0.00, 3.57] 2.75 [1.00, 5.18] |
0.50 [0.00, 0.76] 0.50 [0.25, 1.23] 0.50 [0.00, 2.22] 1.53 [0.75, 3.45] |
0.556 0.679 0.905 0.684 |
| Time of first rescue dose (min) | 1441 [1255, 1441] | 1441 [1441, 1441] | 0.800 |
*Denotes the p-value based on the Mann-Whitney U test.
ESPB, erector spinae plane block; VAS, visual analogue scale
Notes: All date expressed as median [quartile]

*Denotes the p-value based on the Mann-Whitney U test.
VAS, visual analogue scale
ESPB, erector spinae plane block
The VAS score of ESPB group was half that of Control group at 10 minutes after extubation, but there was no statistically significant difference at rest and on moving at all time points.

*Denotes the p-value based on the Mann-Whitney U test.
VAS, visual analogue scale
ESPB, erector spinae plane block
The VAS score of ESPB group was half that of Control group at 6 h after anesthesia induction, but there was no statistically significant difference at rest and on moving at all time points.
Our data showed that ESPB reduced remifentanil consumption during the operation, but it did not reduce fentanyl consumption for postoperative analgesia 24 hours after anesthesia induction in lumbar spine surgery.
It has been reported that the distribution of drug on MRI spread to the epidural space, neural foramina, and intercostal space following a thoracic ESPB in cadavers [13]. However, drug consistently spreads to the posterior branches but not to the ventral rami or paravertebral space following a lumbar ESPB in cadavers [14]. Thus, although drug spread may be different for thoracic and lumbar ESPB, lumbar ESPBs in lumbar spine surgery may provide analgesia by blocking the posterior branches.
Although Oh et al. reported that ESPB provided effective postoperative analgesia resulting in better patient satisfaction and recovery with decreased postoperative nausea and vomiting in patients undergoing lumbar surgery compared to the control in a systematic review of ESPB for lumbar spine surgery, the low-grade quality of evidence compromised the findings [8]. Yayik et al. reported that tramadol consumption and VAS, both at rest and during active movement, were lower in the ESPB group than in the control group [9]. On the other hand, Singh et al. reported that ESPB reduced postoperative morphine consumption and pain scores immediately after surgery and 6 to 8 hours after lumbar surgery with a fixation method [9]. This may suggest that the analgesic effect of ESPB is time-limited. As this result was obtained even with a fixation method which is more invasive, it is possible that the clinical effect of ESPB may not be achieved with laminectomy. The possible reasons for the differences between our study and previous studies showing that ESPB reduced opioid consumption are as follows. First, the analgesic effect of ESPB may be short. Singh et al. reported that ESPB reduced postoperative morphine consumption and pain scores immediately after surgery and 6 to 8 hours after surgery [9]. In our study, the duration of anesthesia was 4–5 hours, and remifentanil consumption during the operation in the ESPB group was lower than that in the control group. The VAS in the short postoperative period was half that of the control group in the ESPB group, although the difference was not statistically significant (Fig. 2). Second, limited cephalocaudal spreading of the drug [14] and thick lumbar erector spinae muscles may have resulted in inadequate block of the posterior branches of the spinal nerves at targeted vertebral levels. Since ESPB is a fascial surface block, an increased drug volume might be necessary for adequate drug spread, even if it means diluting the drug concentration. Third, preoperative opioid use and duration of disease may have influenced the results. There was no difference between two groups in terms of the percentage of opioid (tramadol) users, but we didn’t examine the amount of opioid and duration of illness.
The safe doses of local anesthetic to prevent LAST following lumbar ESPB in patients undergoing spine surgery are unknown. At least two cases of LAST have been reported after lumbar ESPB, including our case. In a case reported by Karaca and Pinar, LAST occurred following lumbar ESPB from the L4 level using 40 ml of local anesthetics containing 20 ml of bupivacaine, 10 ml of lidocaine, 9 ml of saline, and 1 ml of methylprednisolone (40 mg/ml) [15]. However, the study, as well as ours did not indicate the patient’s weight or the concentration of local anesthetic used. In another case, 30 ml of 0.5% (150 mg) levobupivacaine total volume in a 58 kg man (body mass index 21.8 kg/m2) was reported [16]. However, the incidence of LAST with the use of ESPB remained unknown. Given the short analgesic effect of ESPB and the risk of LAST, the benefit of ESPB in spine surgery may be limited.
This was a prospective, randomized, open, blinded-endpoint study in which three protocol violations and one registration failure occurred, which we consider to be a serious problem. Consequently, the registration system was changed from a single to a double check in this study. Additionally, patients and the anesthesiologists caring for them during the surgery were not blinded to group assignments. For this reason, the eight evaluators, who were also anesthesiologists, were blinded to the group assignments. Finally, it is possible that the sample size was too small. We calculated that seven patients were needed to detect a difference in fentanyl consumption for postoperative analgesia from the preliminary cases in our hospital. However, the variability in fentanyl use per case was greater than that expected in this study.
Remifentanil consumption during the operation in the ESPB group was lower than that in the control group. While this suggests ESPB has potential to reduce intraoperative opioid use, it may indicate that ESPB is only effective for a relatively short time. Although the effectiveness and safety of ESPB in lumbar spine surgery remains controversial, further studies are needed regarding the use of ESPB in spine surgery, in order to provide patients with maximum analgesia and minimal side effects.
Ethical Approval
The study protocol was approved by the Shimane University Institutional Committee on Ethics Evaluation Form Regarding the Research Proposal (20181108-1) on January/18/2019.
Author Contribution
YS and IN conceived the idea of the study and developed the statistical analysis plan and conducted statistical analyses. HM and YN collected data. SS contributed to the interpretation of the results. SY supervised the conduct of this study. All authors reviewed the manuscript draft and revised it critically on intellectual content. All authors approved the final version of the manuscript to be published.
Acknowledgement
Not applicable.
Funding
Not applicable.
Conflict of interest
No potential conflict of interest relevant to this article was reported.