2023 年 40 巻 1-2 号 p. 31-36
2023 年 40 巻 1-2 号 p. 31-36
Femoral valgus osteotomy (FVO) is used as a surgery for advanced and terminal hip osteoarthritis (OA). The purpose of this study was to clarify the effect of FVO on preventing the progression of OA. The subjects were 10 patients (43.6 ± 4.6 years) who received FVO. The survey items were hip function (JOA score) and the number of patients who underwent total hip arthroplasty (THA). The causative diseases were developmental dysplasia of the hip in 7 patients, epiphyseal dysplasia 2, and pseudoarthrosis after femoral neck fracture 1. The JOA score improved from 45.4 ± 6.7 points to 60.8 ± 27.2 points at the final survey (p = 0.091). The follow-up period was 133.5 ± 32.9 months, and three joints were converted to THA (131 ± 21.7 months after osteotomy). The preoperative stages of the patients who underwent THA were advanced stages. FVO for early and advanced hip OA under the age of 50 allowed relief of symptoms and joint preservation for more than 10 years.
Hip osteoarthritis (OA) is a disease that causes deformation of the hip joint as a result of joint destruction due to degeneration and wear of articular cartilage of the hip and reactive bone proliferation. As a result, hip pain, limited range of motion, gait disturbance, and as the disease progresses, activity of daily living (ADL) and quality of life (QOL) impairment occur. The basis of treatment is conservative therapy, but if it does not work, surgical treatment is indicated, and if the stage has not progressed in young patients, joint-preserving surgery is recommended [1, 2].
Joint-preserving surgery includes acetabular rotational osteotomy (RAO), Chiari pelvic osteotomy, femoral varus osteotomy, femoral valgus osteotomy (FVO), and arthroscopic surgery, each with different indications and objectives. For the purpose of relieving symptoms and preventing progression of the disease, joint-preserving surgery is used as a curative treatment for young patients whose stage has not progressed [3].
In adolescent patients, RAO [4], Chiari pelvic osteotomy [5], and FVO [6] are performed in anticipation of joint compatibility and symptom relief, even at the advanced or end stage of hip OA.
FVO can move the joint load more to the inside of the femoral head. As a result, joint congruency between the loading surface of femoral head (including osteophytes on the medial side) and the inside of the acetabulum occurs, and the mechanical environment of the hip joint can be improved [6].
For the patients at the advanced and end stages of hip OA after middle age, FVO is performed to relieve symptoms. Although its postoperative outcomes are inferior to those in younger patients and patients at the early stage of hip OA, it is often chosen as a treatment for patients who do not want to undergo total hip arthroplasty (THA) or for the purpose of postponing the timing of THA [3].
The purpose of this study was to clarify the effect of FVO on preventing progression of the disease stage of hip OA and maintaining postoperative activity of daily living (ADL) function in the patients with hip joint diseases.
Patients
We evaluated 11 joints (5 men and 5 women) in 10 patients who were treated at our hospital from September 2006 to March 2019. The patients were 43.6 ± 4.6 years old, 159.4 ± 9.3 cm in height, 65.1 ± 7.9 kg in weight, had a BMI of 25.9 ± 2.0 kg/m2, and followed up for an average of 133.5 months (Table 1).
This study included patients with empowered walking by their lower limbs, no serious cardiovascular or respiratory diseases that interfere with postoperative therapy, no psychiatric disorders, and patients with osteophyte formation on the medial side of the femoral head on X-ray and enlarged lateral joint space on maximum adduction of the hip. We excluded patients with subchondral bone fractures of the femoral head due to bone atrophy, patients who wish to undergo THA, and patients who have difficulty staying in the hospital for a long period of 1 month or more. The study subjects were patients who chose FVO after explaining the surgical indications described above, and not consecutive. Patients who chose FVO were younger patients with early stage of hip OA or patients with advanced stages but did not request THA.
| Patients | 10 patients (11 joints) |
| Male | 5 (6) |
| Female | 5 (5) |
| Causative diseases | |
| DDH | 7 (7) |
| MED | 2 (3) |
| Pseudoarthrosis | 1 (1) |
| Age (years) | 43.6 ± 4.6 (24–50) |
| Height (cm) | 159.4 ± 9.3 (141–174) |
| Body weight (kg) | 65.1 ± 7.9 (58–80) |
| BMI (kg/m2) | 25.9 ± 2.0 (23.1–29.9) |
| Follow-up period (months) | 133.5 ± 32.9 (24–192) |
DDH: developmental dysplasia of the hip; MED: multiple epiphyseal dysplasia; Pseudarthrosis: pseudoarthrosis after femoral neck fracture
Surgical methods
As for the surgical procedure, lateral open wedge osteotomy of the femur [7] was performed in 8 joints in 7 patients, and trochanteric valgus osteotomy of the femur [8] was performed in 3 joints in 3 patients. Acetabular-plasty (shelf operation; Spitzy method) [9] was added to two joints because the acetabular head index (AHI) was less than 70% [6].
Postoperative rehabilitation
As postoperative therapy, patients began to receive active and passive range of motion exercises and to use a wheelchair on the second postoperative day. One-third partial load walking started at 4 weeks and shifted to full load walking at 3 months. As a postoperative rehabilitation for patients who underwent shelf operation, skin traction was used for 4 weeks, partial load walking using crutches was started at 8 weeks, and full load walking was performed from 3 months after surgery.
Outcome measure
The items investigated were the causative disease, the hip function assessment using the Japanese Orthopaedic Association hip score (JOA score) [10], the radiological stage of hip OA by JOA classification [11], and whether THA was performed.
Statistical analysis
Statistical analysis was performed using the Wilcoxon signed-rank test in BellCurve for Excel® ver. 2.0 (SSRI Co., Ltd. Tokyo, Japan) for comparison of clinical evaluation scores, and statistical significance was accepted for values of p < 0.05.
The causative disease was developmental dysplasia of the hip (DDH) in 7 patients with 7 joints, multiple epiphyseal dysplasia (MED) in 2 patients with 3 joints, and pseudoarthrosis after femoral neck fracture in 1 patient with 1 joint (Table 1). There were three patients with bilateral hip joint disease. The JOA score improved from 45.4 ± 6.7 points preoperatively to 60.8 ± 27.2 points at the time of the final study, but there was no significant difference (p = 0.091), as this included the results of patients who transitioned to THA (Table 2).
In preoperative radiological staging, there was one joint in one patient at the early stage, 10 joints in 9 patients at the advanced stage, and no end stage (Table 3). As for the evaluation at the time of the final survey, there was 1 joint in one patient at the early stage, 6 joints in 5 patients at the advanced stage, and 4 joints in 4 patients at the end stage (Table 3). THA was performed 131 ± 21.7 months after osteotomy in 3 of 4 patients who progressed to the end stage, and all of these patients were at the advanced stage preoperatively.
Figure 1 shows an X-ray of a 42-year-old male patient with MED (Fig. 1). The patient’s preoperative stage was the advanced stage and had a JOA score of 48 points. This patient showed no stage progression 11 years after surgery and maintained a JOA score of 83 points.
Figure 2 shows an X-ray of a 24-year-old female patient with DDH (Fig. 2). This patient was at the early stage preoperatively, with a JOA score of 55 points. This patient remained at the early stage of the disease at 8 years postoperatively and had a JOA score of 80 points.
Figure 3 shows an X-ray of a 50-year-old male patient with unilateral DDH (Fig. 3). Preoperative X-ray showed that the disease was at an advanced stage, with osteophyte formation in the acetabulum. Eleven years later, THA was taking place.
| Preoperative (points) | Final follow-up (points)* | P value |
|---|---|---|
| 45.4 ± 6.7 | 60.8 ± 27.2 | 0.091 |
* In THA conversion cases, JOA scores immediately before surgery were adopted.
| Stage (JOA) | Preoperative | Final follow-up |
|---|---|---|
| Early | 1 patient (1 joint) | 1 (1) |
| Advanced | 9 (10) | 5 (6) |
| End | 0 (0) | 4 (4) |
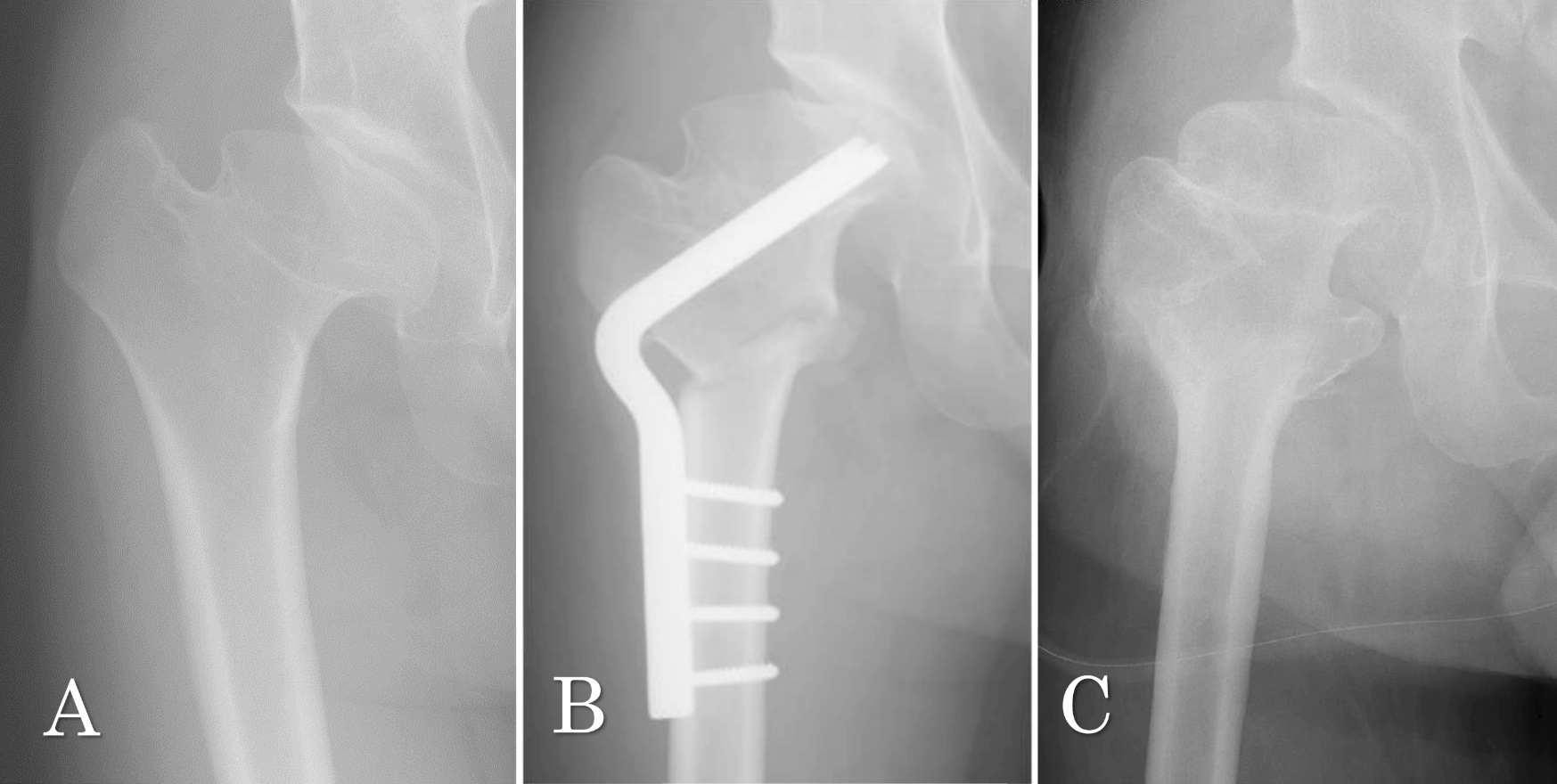
A: Preoperative X-ray shows the advanced stage of hip OA. JOA score is 48 points. B: Just after osteotomy. C: 11 years after osteotomy. JOA score is 83 points. Hip joint modeling has progressed and the stage remains at the advanced stage.
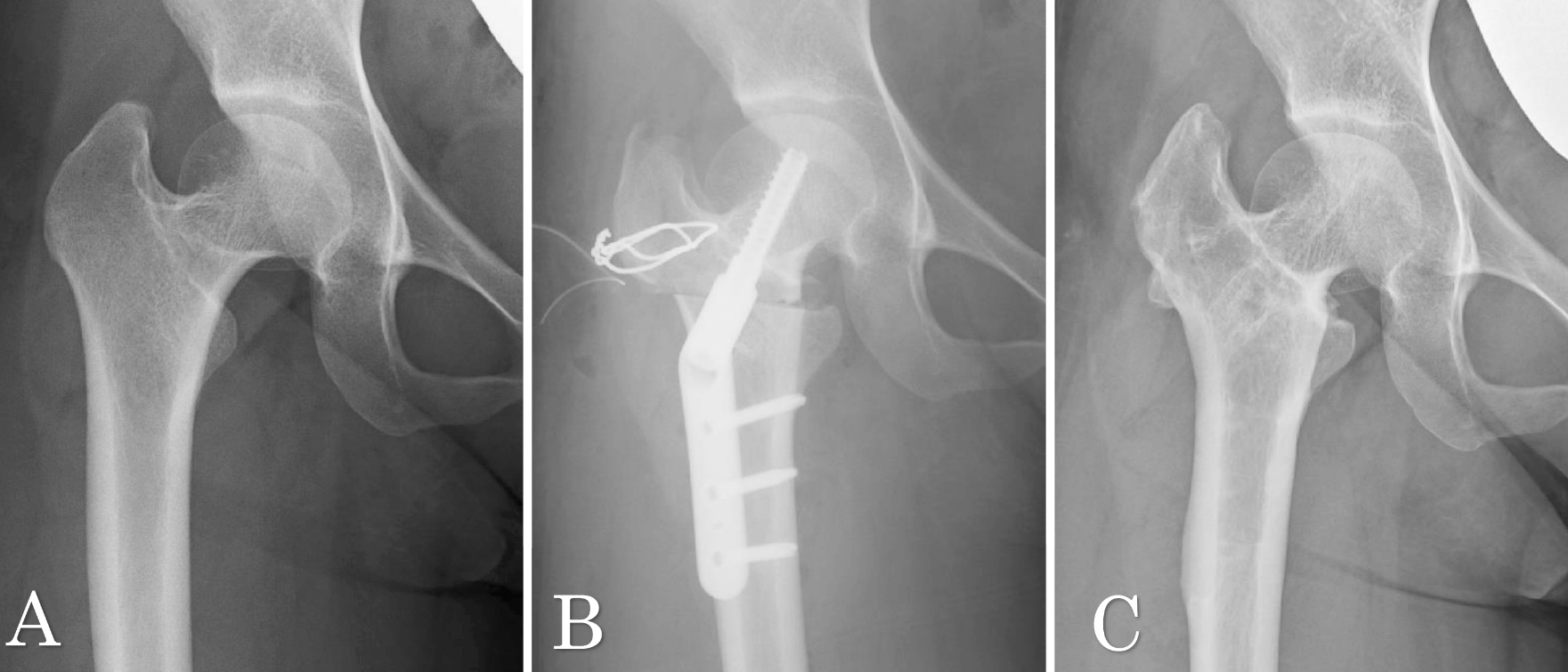
A: Preoperative X-ray shows the early stage of hip OA. JOA score is 55 points. B: Just after osteotomy. C: 8 years after osteotomy. JOA score is 80 points. OA stage remains at the early stage.

A: Preoperative X-ray shows the advanced stage of hip OA. JOA score is 31 points. B: Just after osteotomy. C: 2 years after osteotomy. JOA score is 70 points. OA stage remains at the advanced stage. D: OA stage progresses to the end stage with 31 points for JOA score. E: THA is performed at 11 years after osteotomy. JOA score is 92 points.
There are some reports on FVO using various kinds of surgical technique for hip osteoarthritis, but not many have been followed for more than 10 years [12,13,14,15]. Yasunaga et al. performed FVO in patients with advanced secondary OA with an average age of 46 years and followed them for an average of 10.7 years [6]. They compared surgical outcomes in two groups, with FVO alone and FVO combined with shelf operation, and the survival rates using THA conversion as an endpoint were good in both groups, from 85.5% to 100% at 10 years and from 77.7% to 92.3% at 15 years. Their report suggested that even if acetabular dysplasia is moderate, the progression of the disease can be prevented by using shelf operation in combination with FVO.
In our case, a 50-year-old man converted to THA was at an advanced stage preoperatively, with the formation of osteophyte in the acetabulum, and the subluxation progressed (Fig. 3). In such patients, THA may have been chosen from the beginning, but if joint-preserving surgery had been chosen, Chiari pelvic osteotomy, which allows the femoral head to be medialized, should have been chosen instead of shelf operation [15].
This study has some limitations. The first is the small number of patients. Therefore, the treatment results for the same disease cannot be compared, and another problem is that two types of FVO were performed because the survey period was relatively long. In order to solve these problems, we believe that more cases are needed. The second limitation is that when FVO was combined with shelf operation, the effect of FVO alone cannot be clarified. Because it is empirically known that if a patient’s AHI is less than 70% outcomes of FVO alone would deteriorate [6], we followed this lesson and combined FVO with shelf operation. The third limitation is that patient subjective satisfaction was not assessed. The Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire (JHEQ) [16], which has recently been developed in Japan, has made it possible to evaluate subjective evaluation and QOL after surgery. These evaluations are essential for comparing the surgical outcomes of osteotomies and THA.
Advances in THA’s technology in recent years have provided significant benefits [17]. Improvements in the artificial joint material have resulted in less wear, and improved surgical approaches, which have resulted in early mobilization, shorter hospital stays, and reduced dislocation rates, and improved long-term outcomes owing to precise implant placement through a navigation system for surgery. Therefore, the indication of THA is spreading to relatively young patients, and postoperative sports activities are being expanded more than before [18].
However, the merits of joint-preserving surgery, such as relief from the anxiety of reoperation due to implant wear, breakage, infection, dislocation, and loosening of the implant, should not be underestimated, and joint-preserving surgery is a surgical method that should be considered for the younger patients at the early stage of hip OA.
We performed FVO in patients with early and advanced stages of hip OA under the age of 50 and confirmed that symptom relief and joint preservation were possible for more than 10 years. However, patients at the advanced stage after their 40s tended to shift to THA about 10 years after FVO.
Ethical Approval
This study was conducted in accordance with the principles of the Declaration of Helsinki and the Good Clinical Practice Guidelines. This study was also conducted with the approval of the Shimane University School of Medicine and the Medical Ethics Committee (Accreditation No. 4705).
Authors Contribution
All authors contributed to the study conception, and data collection and analysis were performed by Sokichi Maniwa. The first draft of the manuscript was written by Sokichi Maniwa and all authors commented on the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors wish to acknowledge Dr. Yuji Uchio, Professor of Orthopaedic Surgery, Shimane University Faculty of Medicine, for his instruction and cooperation.
Funding
No research funds were used for this study.
Conflict of interest
All authors confirm that there are no conflicts of interest to declare.