2013 年 230 巻 2 号 p. 117-121
2013 年 230 巻 2 号 p. 117-121
Most dialysis centers adopt a standard dialysate sodium prescription. While pre-hemodialysis (HD) serum sodium levels remain relatively constant in each individual patient on chronic HD, these levels can vary between different patients. Therefore, a single dialysate sodium prescription may not be appropriate for all patients. Nineteen stable patients on maintenance HD were dialyzed for 9 HD sessions with their current dialysis solutions, followed by another 9 sessions using individualized prescriptions created by aligning dialysate sodium levels to each patient’s serum sodium concentration. Patients were divided into 2 groups according to whether the average pre-HD serum sodium concentration was higher than (higher serum sodium group, n = 13) or equal to (equal sodium group, n = 5) the standard dialysate sodium concentration. Pre-HD serum sodium levels remained constant during entire study period in both groups. In higher serum sodium group, interdialytic weight gain increased after implementation of the sodium alignment (2.0 ± 0.3 kg vs. 2.3 ± 0.4 kg; P = 0.008). Thirst scores also increased in patients whose dialysate sodium was increased by 4 mmol/L (n = 7) (6.4 ± 1.5 vs. 7.6 ± 1.5, P = 0.015). There were no significant changes in blood pressure and intradialytic complications. In equal sodium group, significant differences were not observed in any parameters. Our results suggest that alignment of dialysate sodium levels to each patient’s serum sodium concentration is of little benefit in hemodynamically stable patients who have pre-HD serum sodium concentrations higher than dialysate sodium concentration.
The optimal dialysate sodium concentration has been debated despite numerous investigations (Flanigan 2000). In current clinical practice, most hemodialysis (HD) centers adopt a standard dialysate sodium prescription in the range of 136-142 mmol/L, with only a few variations according to patients’ clinical conditions. It has been documented that patients on chronic HD have relatively constant pre-HD serum sodium levels, but vary considerably from patient to patient (Peixoto et al. 2010; Basile et al. 2012). Therefore, a single dialysate sodium prescription for all HD patients may adversely affect sodium balance in a significant proportion of patients.
The direction of sodium flux during HD is determined by the sodium gradient, i.e. the difference in sodium concentration between dialysate and serum. Higher sodium concentrations in dialysate than in serum (positive sodium gradient) can cause unnecessary intradialytic sodium gain, resulting in increased thirst, fluid retention and hypertension in HD patients (Munoz Mendoza et al. 2011; Penne and Sergeyeva 2011). In contrast, diffusive sodium loss can lead to intradialytic symptoms, such as hypotension and muscle cramps, if the sodium concentration is lower in the dialysate than in serum (negative sodium gradient). Previous studies have reported that reduction in dialysate sodium based on pre-HD plasma sodium levels improves thirst, interdialytic weight gain (IDWG), hypertension and intradialytic hypotension (Murisasco et al. 1985; de Paula et al. 2004; Sayarlioglu et al. 2007). However, we could not find any studies on individualized dialysate sodium prescriptions for patients who have serum sodium concentrations higher than typical dialysate sodium concentrations. The aim of the present study was to determine the short-term effects of alignment of dialysate and serum sodium concentrations on blood pressure (BP), IDWG, thirst and intradialytic symptoms in patients with negative sodium gradients.
The study was approved by the Institutional Review Board of Seoul National University Hospital, and each subject gave written informed consent. Nineteen stable patients on maintenance HD were enrolled in the study. The patients had been on a dialysis program three times a week and had not had an alteration to the composition of their dialysate or dry weights for more than 3 months before enrollment. All patients had Kt/V greater than 1.2 and residual daily urine output less than 300 ml. Diabetic patients were excluded to avoid the possible effects of hyperglycemia on serum sodium concentrations. None of the patients were receiving hemodiafiltration or high-flux HD.
Study protocolThe study was divided into two 3-week periods: the standard and individualized periods. During the standard period, patients received 9 HD sessions with their current dialysis solutions whose sodium concentrations were set at 136 (n = 15) or 138 mmol/L (n = 4). During the individualized period, patients received 9 additional HD sessions using the individualized prescription in which the dialysate sodium levels were aligned to individual serum sodium levels. The dialysate sodium levels were adjusted to even numbers; thus, levels were set at 136 mmol/L if patient’s average pre-HD serum sodium levels were 135.0-136.9 mmol/L, at 138 mmol/L if 137.0-138.9 mmol/L, and at 140 mmol/L if 139.0-140.9 mmol/L. One patient who had a serum sodium concentration lower than the standard dialysate sodium concentration was excluded. The remaining 18 patients were divided into 2 groups: those whose average pre-HD serum sodium concentrations were higher than the dialysate sodium concentrations being used (higher serum sodium group, n = 13) and those equal to the dialysate sodium concentrations (equal sodium group, n = 5). The remainder of dialysis prescription, dry weight and hypertensive medications were not modified throughout the study period. A standard low-sodium diet was enforced, but no additional dietary interventions were performed.
Measurements and definitionsPre-HD serum sodium concentrations were measured just before the start of each midweek dialysis session using the indirect ion-selective electrode method (Hitachi 7600; Toshiba, Tokyo, Japan). BP values were obtained using an automated BP measuring device and IDWG and ultrafiltration volume were recorded at each session and the means for the 9 sessions of each period were used for analysis. Thirst scores were measured during the last 3 sessions of each period using a Likert scale questionnaire (never = 1; almost always = 5). Hypotensive episodes, nursing interventions and intradialytic symptoms were recorded as a total number of events during each period. A hypotensive episode during dialysis was defined as a rapid drop in BP accompanied by symptoms requiring nursing interventions or as a 30 mmHg or greater decrease in systolic BP. The quality of life was assessed at the end of each period using the Kidney Disease Quality Of Life-Short Form (KDQOL-SF) questionnaire. Two patients who did not complete the questionnaire were excluded from the quality of life analysis. Baseline comorbidity was calculated using the Charlson comorbidity index (Hemmelgarn et al. 2003).
Statistical analysisThe Mann-Whitney test and the Chi-Square test were used to compare continuous and categorical variables, respectively, between groups A and B. The Wilcoxon signed rank test and McNemar’s test were used to compare continuous and categorical variables, respectively, between the standard and individualized periods within each group. A P value of < 0.05 was considered statistically significant. All data were analyzed using SPSS for Windows (SPSS Inc, Chicago, IL, USA).
Baseline demographic characteristics of the study population are shown in Table 1. Comparing with equal sodium group, the patients in higher serum sodium group were younger and the average pre-HD serum sodium concentration was higher. Pre-HD BP levels and the number of antihypertensive drugs were also higher, although statistically insignificant. Six patients (46.2%) in higher serum sodium group and 1 patient (20%) in equal sodium group were on diuretics. All patients with diuretics treatment had daily residual urine output less than 300 ml. There were no significant differences in sex, HD duration, IDWG, Kt/V and Charlson comorbidity index between the groups.
Pre-HD serum sodium levels remained constant during the entire study period in both groups (Table 2). Patients in higher serum sodium group had more IDWG and ultrafiltration volumes during the individualized period than during the standard period. As a result of the sodium alignment, the dialysate sodium concentration increased from 136 to 138 mmol/L in 4 patients, from 138 to 140 mmol/L in 2 patients, and from 136 to 140 mmol/L in 7 patients, all in higher serum sodium group. In other words, the dialysate sodium concentration increased by 2 mmol/L in 6 patients and by 4 mmol/L in 7 patients. There were no significant differences in thirst scores for higher serum sodium group taken as a whole. However, when stratified analyses were performed based on the degree of increase in dialysate sodium concentration, patients whose dialysate sodium was increased by 4 mmol/L had higher thirst scores during the individualized period than during the standard period (7.6 ± 1.5 vs. 6.4 ± 1.5, P = 0.038). There were no significant differences in BP, KDQOL-SF scores and intradialytic complications between the 2 periods in higher serum sodium group (Table 3, 4). All patients in equal sodium group were dialyzed without altering the dialysate prescription throughout the study period and significant differences were not observed in any parameters.
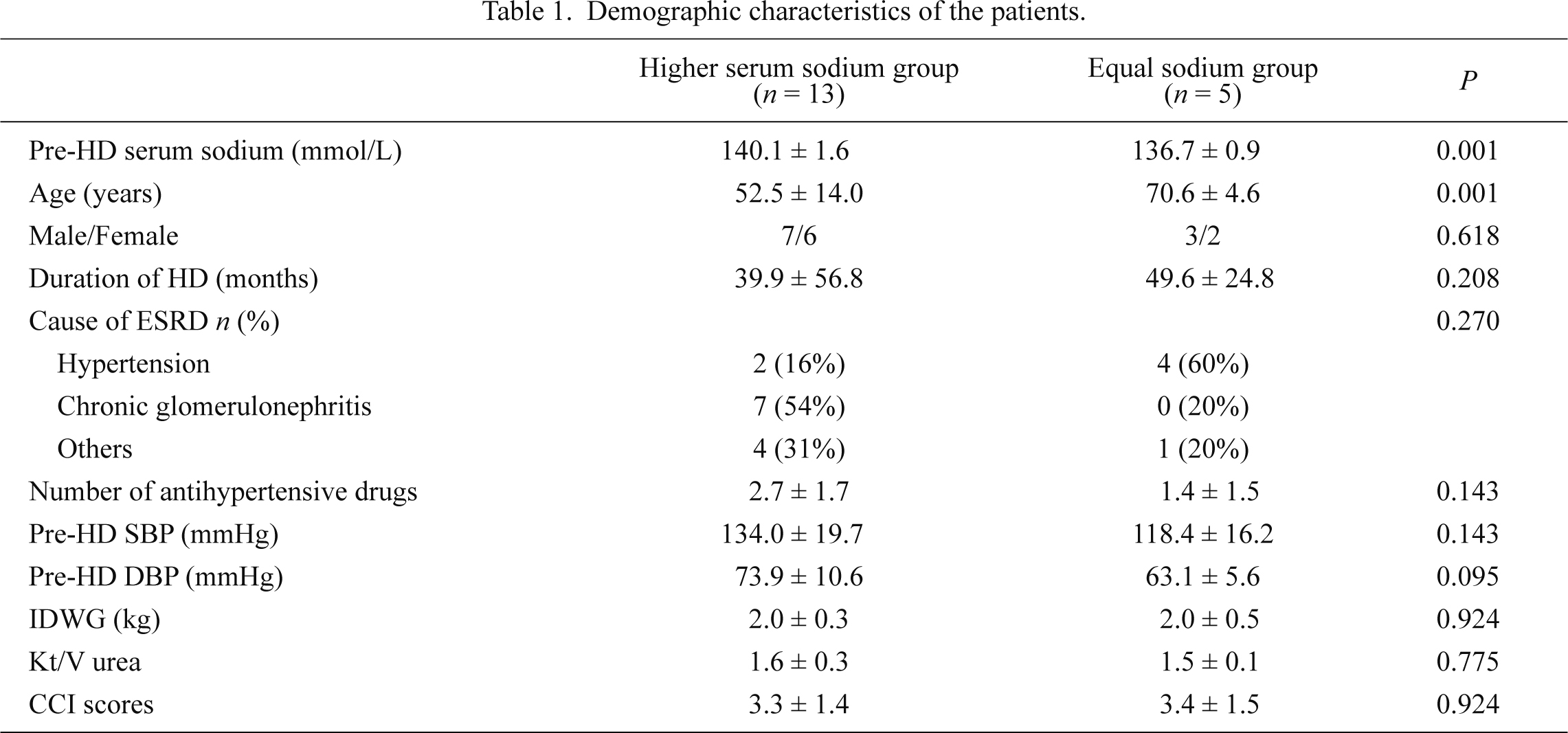
Demographic characteristics of the patients.
Values are expressed as mean ± s.d., or number (percent).
CCI, Charlson comorbitidy index; HD, hemodialysis; ESRD, end stage renal disease; SBP, systolic blood pressure; DBP, diastolic blood pressure; IDWG, interdialytic weight gain.

Changes in serum sodium, dialysis parameters and thirst after sodium alignment.
Values are expressed as mean ± s.d.
UF, ultrafiltration; other abbreviations as in Table 1.
aSignificantly different from level before sodium alignment at P < 0.05.
bThirst scores in 7 patients whose dialysate sodium increased by 4 mmol/L was significantly higher during the individualized period than during the standard period (7.6 ± 1.5 vs. 6.4 ± 1.5, P = 0.038).

Changes in KDQOL-SF scores after sodium alignment.
Values are expressed as mean ± s.d.
aSignificantly different from level before sodium alignment at P < 0.05.
bTwo patients who did not complete the KDQOL-SF questionnaire were excluded.
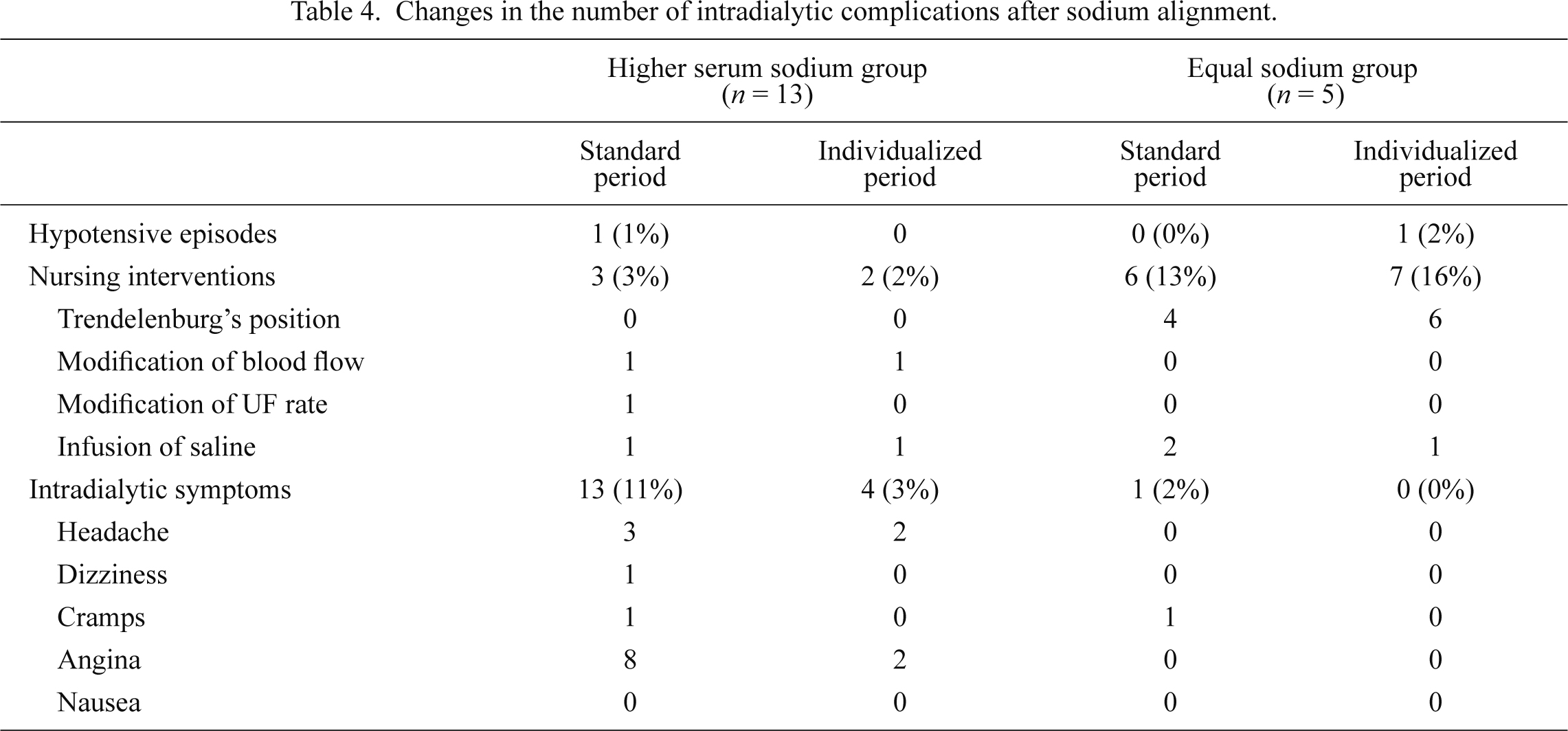
Changes in the number of intradialytic complications after sodium alignment.
Values are expressed as number (percent).
UF, ultrafiltration.
aSignificantly different from level before sodium alignment at P < 0.05.
The present study confirmed the results of earlier studies which indicated that HD patients have stable pre-HD serum sodium levels even after manipulation of dialysate sodium (de Paula et al. 2004; Basile et al. 2012). Although some long-term studies have revealed that individual osmolar set-points are influenced by changes in dialysate sodium concentration, they vary by less than 1% (Song et al. 2002; Thein et al. 2007). Therefore, the individualized approach to prescribing dialysate sodium seems to be a reasonable way to avoid salt loading from a high-sodium dialysate and hemodynamic instability from a low-sodium dialysate. de Paula et al. (2004) have reported that individualized prescriptions made by aligning dialysate sodium to serum sodium decreases thirst, IDWG and pre-HD BP in patients with positive sodium gradients. They also described that the decrease in dialysate sodium concentration contributes to better tolerability of dialysis because less fluid needs to be removed (Santos and Peixoto 2008). However, that study did not include intradialytic hypotension-prone patients. A recent small study showed that 4 of 6 patients prone to hypotension requiring an intervention (> 25 % of HD sessions) received more frequent interventions after individualized reduction of dialysate sodium (Arramreddy et al. 2012). Moreover recent analysis of the Dialysis Outcomes and Practice Patterns Study (DOPPS) database has reported that patients with serum sodium levels < 137 mmol/L who were dialyzed with dialysate sodium prescriptions > 140 mmol/L have a lower mortality rate (Hecking et al. 2012). Although low serum sodium concentrations are associated with increased mortality and co-morbid conditions, such as congestive heart failure, higher dialysate sodium prescriptions may have protective effects by providing intradialytic cardiovascular stability (Waikar et al. 2011). Further studies are needed to determine the long-term efficacy and safety of sodium alignment in patients with positive sodium gradients.
In the present study, we found that increasing the dialysate sodium concentration based on serum sodium concentrations exacerbated weight gain and thirst in patients with negative sodium gradients. Extracellular volume expansion is a predominant factor in the pathogenesis of hypertension and left ventricular hypertrophy in the HD patients (Leypoldt et al. 2002). Higher IDWG has been reported to be associated with higher all-cause and cardiovascular death risks in chronic HD patients (Kalantar-Zadeh et al. 2009). The existence of the lag phenomenon between extracellular volume and BP changes may explain our negative findings in BP after only 3 weeks of intervention (Twardowski 2008). Although the number of intradialytic complications in higher serum sodium group was too small to reach statistical significance, the frequency of angina episodes was markedly reduced after sodium alignment as shown in Table 4. The quality of life summary scores also showed a trend of improvement, particularly for mental component summary. While these data suggest that an increase in the dialysate sodium concentration may improve tolerability of dialysis, we should also note that there are many patients with negative sodium gradients without intradialytic symptoms. Indeed, Munoz Mendoza et al. (2011) showed that no significant differences were observed in the frequency of intradialytic hypotension between patients with sodium gradients of ≤ 0 and those with positive sodium gradients. Therefore, it appears that sodium alignment may not be required for all patients with negative sodium gradients. Increasing the dialysate sodium concentration can be harmful to patients with fluid retention and be helpful in patients with frequent intradialytic symptoms.
The primary limitation of this study is the lack of evaluation of sodium balance during dialysis. We used the indirect potentiometric method to analyze sodium levels, which requires the correction for plasma water and the Donnan factor. In general, plasma water correction virtually cancels the Donnan correction and zero sodium gradients can be expected when dialysis fluids are designed to be close to or equal to the plasma concentration (Lomonte and Basile 2011). In addition, given that the patients in equal sodium group did not exhibit significant differences in any parameters, we believe that our method for individualizing and adjusting the dialysate sodium levels was adequate to obtain an isonatremic dialysis. Other limitations of this study include its small sample size, short duration of the intervention, and the lack of measurements of ambulatory BP.
In conclusion, the individualized prescription of dialysate, created by aligning dialysate sodium to pre-HD serum sodium, is of little benefit in hemodynamically stable HD patients with negative sodium gradients. We need to be aware that even a subtle increase in dialysate sodium concentration based on the serum sodium concentration can lead to fluid overload in patients without intradialytic symptoms. The alignment of dialysate and serum sodium concentrations should be considered only in the selected subgroups of patients. Further large-scale studies on the selection of these subgroups and the long-term clinical significance of sodium alignment are warranted.
The authors would like to appreciate Prof. Sehyun Kim at Graduate School of East West Medical Science, Kyung Hee University for permission to use the Korean version of KDQOL-SFTM 1.3.
The authors declare no conflict of interest.