2013 年 230 巻 2 号 p. 123-127
2013 年 230 巻 2 号 p. 123-127
Juvenile xanthogranuloma (JXG) is a benign manifestation of non-Langerhans cell histiocytosis characterized by yellowish cutaneous nodules. Its occurrence in the larynx is very rare, but laryngeal JXG may cause severe respiratory distress. We report a patient with isolated laryngeal JXG treated by laryngomicrosurgery, and this is the first report of JXG extending to vocal fold. A 3-year-old girl presented with hoarseness and inspiration stridor. A bulky tumor was found in right glottic to subglottic region. Subtotal resection of the tumor was carried out by laryngomicrosurgery, and airway distress was diminished after the operation. In pathological examination, the resected specimen showed proliferation of histiocytic cells and spindle cells with Touton giant cells that are characterized by polynuclei or wreath nuclei and are known to appear in JXG but not in LCH. Immunohistochemistry of histiocytic cell markers demonstrated positivity for CD68, lysozyme, alpha1-anti-chymotrypsin, factor XIIIa and vimentin, and negativity for CD1a and S-100, leading to diagnosis of JXG, but not LCH. The patient was thus expected with benign prognosis, and additional resection of the tumor including vocal fold was not indicated in the initial treatment. Six weeks later, the JXG recurred and a second procedure using CO2 laser was needed. The tumor did not re-grow thereafter, and there was no residual voice handicap. Because of its favorable prognosis and tendency for spontaneous regression, JXG in the larynx needs to be considered carefully with regard to whether reduction surgery and/or tracheotomy are necessary, and thus precise diagnosis is required.
Most cases of airway distress in infants and young children are due to inflammatory diseases such as croup and bronchial asthma. However, tumors or tumor-like legions may be responsible for laryngeal narrowing in small minority of patients, and because they are usually treated initially as inflammatory diseases, their diagnosis is sometimes delayed. Endoscopic examination of the larynx should therefore be carried out in the early period when airway narrowing is suspected and the possibility of a laryngeal tumor should be considered in the differential diagnosis. Juvenile xanthogranuloma (JXG) is a manifestation of non-Langerhans cell histiocytosis characterized by yellowish cutaneous nodules. The diagnosis of the JXG is made on the basis of clinical features, pathological findings, and immunological examinations (Dehner 2003). Among histiocytic disorders, making a distinction between JXG and Langerhans cell histiocytosis (LCH) is often important clinically because the prognosis of LCH is worse than that of JXG, and this can usually be accomplished reliably on the basis of histology especially by immunohistochemistry using histiocytic cell markers (Somorai et al. 2007). JXG appears in children under 2 years old and shows a tendency to enlarge locally in the early period of the disease (Freyer et al. 1996). Among tumors affecting the larynx, JXG is quite rare, and only five cases have been reported in the English literature (Benjamin et al. 1995; Thevasagayam et al. 2001; Sahhar et al. 2003; Somorai et al. 2007; Wang et al. 2010). Especially, vocal fold involvement by JXG has not been reported. Here we describe an unusual case of JXG in the larynx of a 3-year-old child who presented with glottic and subglottic narrowing, which was investigated by endoscopy at an early stage and treated twice by laryngomicrosurgery.
A 3-year-old girl presented with a 2-week history of hoarseness and inspiration stridor. At the age of one year, she had undergone surgery for cleft palate under general anesthesia using endotracheal intubation. Endoscopic examination demonstrated a bulky mass with a smooth surface in the right vocal fold to subglottic region. She was initially diagnosed as having an inflammatory condition with laryngeal granuloma, and was treated with systemic corticosteroid and antibiotic agents for one week. However the area of the mass enlarged, causing narrowing of the glottic space (Fig. 1A). CT examination confirmed that the framework of the larynx was not affected.
Subtotal resection of the right glottic mass was performed by laryngomicrosurgery to determine the diagnosis and relieve the airway distress. At beginning of the surgery, the saturation ratio of arterial oxygen was normal and mask ventilation was possible, thus an oral endotracheal intubation was carefully performed for the general anesthesia under the preparation of a tracheotomy. A reddish, smooth-surfaced, soft and fragile mass was found to extend from the edge of the right vocal fold to the subglottic lateral wall (Fig. 1B). The mass was reduced piecemeal using a knife and sharp forceps taking care to preserve the vocal ligament (Fig. 1C) under a tentative intraoperative diagnosis of histiocytosis based on the histology of the frozen section. A small amount of bleeding was seen during the reduction surgery, and therefore tracheotomy was avoided. Pathological examination of the resected specimens demonstrated proliferation of histiocytic cells and spindle cells in a subepithelial stroma with many giant cells possessing wreaths of nuclei, i.e. so-called Touton giant cells (Figs. 2A and B). For the differential diagnosis among the histiocytic diseases, immunohistochemistry using histiocytic cell markers was carried out. The tumor cells were positive for CD68 (Fig. 2C), lysozyme, alpha1-anti-chymotrypsin, factor XIIIa (Fig. 2D) and vimentin, but negative for CD45, CD1a (Fig. 2E), and S100 (Fig. 2F). Immunohistochemistry for the cancer suppressor gene p53 showed negativity, and a cell proliferation marker Ki-67 showed 18% of labeling ratio in the tumor. On the basis of the pathological findings and clinical manifestations, a diagnosis of solitary JXG in the larynx was made.
Six weeks after the initial operation, the JXG recurred (Fig. 3A) and a second laryngomicrosurgical procedure was needed. In the second operation, the resected area was deeper than that in the first operation to avoid the recurrence of the tumor, and therefore the amount of bleeding was increased. Accordingly, we used a CO2 laser to control the bleeding from the tumor and to resect the tumor accurately while preserving the vocal fold ligament (Fig. 3B, C). During six months after the second operation, the JXG regressed spontaneously (Fig. 3D). There was no remnant vocal handicap, and the patient and her family have not reported any voice problems in daily life.
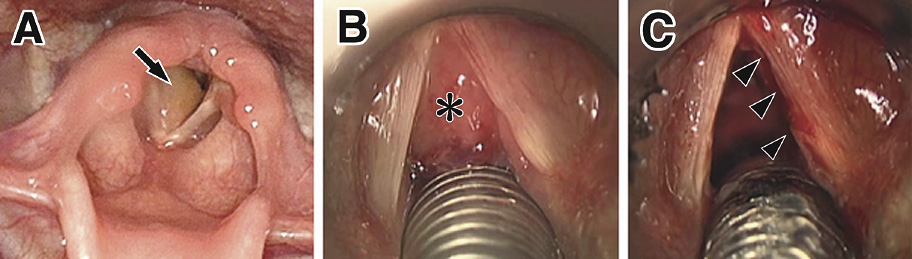
Findings of the larynx before and after the first operation.
A. Preoperative fiberoptic image demonstrates a bulky mass in the right glottic to subglottic region (arrow). Note that the glottic to subglottic space is narrow. B and C. Microscopic images during the first operation. A soft reddish mass occupies the glottic to subglottic space (asterisk in B). After subtotal cold resection, the vocal fold is preserved (arrowhead in C).
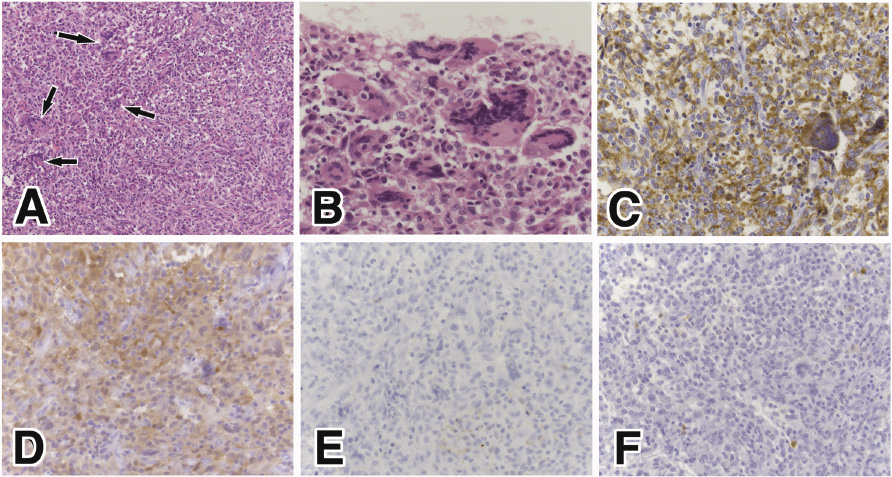
The histological and immunohistochemical findings in the present patient.
A and B. H.E. staining. Note the proliferation of the histiocytic and spindle cells with giant cells (arrows) (low magnification). Giant cells with polynuclei or wreath nuclei, called Touton giant cells, were prominent (high magnification). The Immunohistochemical stainings of the proliferating cells demonstrated positivity for CD68 (C) and Factor XIIIa (D) and negativity for CD1a (E) and S100 protein (F).
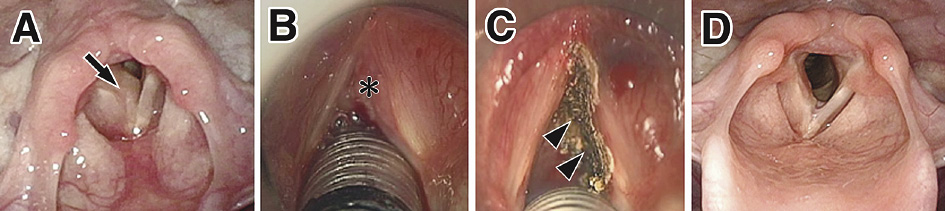
Findings of the larynx before and after the second operation.
A. The tumor has enlarged again (arrow) causing airway distress. B and C. Microscopic images during the second operation. A soft tumor extending from the right glottic to subglottic region (asterisk in B) was removed and ablation was performed using a carbon dioxide laser (arrowheads in C). D. Six months after the second operation, the tumor has not enlarged and the glottic space is preserved.
JXG is a benign form of dendritic cell-related, non-Langerhans histiocytosis and shows varied biological behavior, usually presenting within 2 years after birth and showing spontaneous regression (Somorai et al. 2007). It most commonly presents as a solitary cutaneous mass, but rarely may be systemic, affecting the central nervous system, liver, spleen, deep soft tissues and/or the hematopoietic system, sometimes with a lethal outcome (Freyer et al. 1996). JXG in the larynx is quite rare, and our search of the English literature revealed only 5 such cases (Table 1), in which JXG was localized at the aryepiglottic fold (Benjamin et al. 1995; Wang et al. 2010) or the subglottis (Thevasagayam et al. 2001; Sahhar et al. 2003; Somorai et al. 2007). The present patient of subglottic JXG is the first reported to have extended to the vocal fold.
Among histiocytic disorders, making a distinction between JXG and LCH is often important clinically because the prognosis of LCH is worse than that of JXG, and this can usually be accomplished reliably on the basis of histology (Lazova and Shapiro 1999; Lau et al. 2008). In contrast to LCH, the prognosis of solitary JXG is favorable and spontaneous regression may occur, despite rare cases of relapse (Freyer et al. 1996; Somorai et al. 2007). LCH in children over the age of 5 years tends to appear as an isolated lesion and most of such cases are benign with spontaneous regression. On the other hand, LCH patients who present at a younger age and those with widely disseminated disease and organ dysfunction have the highest mortality (Satter and High 2008). In one large study of 101 children with LCH, the overall survival rate was 71% at 5 years (Alston et al. 2007).
Histologically it is very important to distinguish JXG from LCH for definitive treatment. JXG shows proliferation of histiocytic cells and spindle cells with Tourton giant cells. The nuclei of the infiltrating cells are oval or occasionally slightly indented, and the cytoplasm is finely vacuolated, which express positive immunoactivity for CD68 and Factor XIIIa, further negative for CD1a (Jaffe et al. 2008). By contrast, the histiocytic cells proliferating in LCH possess abundant, pinker or redder cytoplasm and many of the nuclei are obviously indented (Lazova and Shapiro 1999). Touton giant cells have not been documented in any previously established case of LCH. Immunohistochemistry demonstrates positive staining for CD1a, langerin and S-100. These findings are very useful for differential diagnosis (Lau et al. 2008) between JXG and LCH. In the present patient, histiocytic cells and spindle cells were evident in the subepithelial stroma with Touton giant cells that were immunoreactive for CD68 and Factor XIIIa, but negative for CD1a and S-100. Consequently, the final pathological diagnosis was confirmed as JXG. The origin of JXG in still unknown, but as the cells positive immunoreactive for CD68 and Factor XIIIa, but negative for CD1a and S-100, may indicated a dermal-intestinal dendritic cell origin (Somorai et al. 2007).
Diagnosis of tumorous legions in the larynx is sometimes delayed in infants and young children because symptoms such as, stridor and hoarseness are often considered to be due to croup or bronchial asthma in the absence of direct investigation of the larynx. In previously reported patients, the period from initial admission until diagnosis of JXG has varied from 2 weeks (Sahhar et al. 2003) to 9 months (Thevasagayam et al. 2001). In the latter clinical report, the patient was treated for bronchial asthma before a correct diagnosis was established. In the present patient, initial endoscopic examination was carried out in the ENT clinic and revealed the glottic mass but considered as a granuloma with inflammation because her history of endotracheal intubation for general anesthesia. In infants and young children with airway distress, early evaluation using fiberscopy and/or X-ray and CT images of the neck is important for obtaining a correct diagnosis, and furthermore if a mass lesion is detected, histological evaluation is recommended to expedite prompt therapy if necessary.
Because of its tendency for local growth in the early period, the JXG in the present patient was treated by reduction surgery twice using direct laryngoscopy, but tracheotomy was not necessary. The reduction surgeries were carried out with preservation of the vocal ligament to prevent any subsequent voice handicap. A tiny remnant web was evident in the glottis, but the hoarseness was improved. Among previously reported patients, two were treated by tracheotomy and local biopsy for diagnosis (Benjamin et al. 1995; Thevasagayam et al. 2001). After the diagnosis of JXG, the tumors regressed spontaneously in both cases during long-term observation of the remnant tumors. Because recurrence of JXG is rare and spontaneous regression can be expected, the four recently reported patients including the present one were managed by laryngomicrosurgery for tumor reduction without tracheotomy, and this strategy had the merit of avoiding complications of pediatric tracheotomy, for example,subglottic stenosis and bleeding with local granulation (Mahadevan et al. 2007). However, in children with severe airway narrowing that makes endotracheal intubation difficult, prompt therapy with tracheotomy should be performed without hesitation. JXG in the larynx needs to be considered carefully with regard to whether reduction surgery and/or tracheotomy are necessary, according to the specific diagnosis.
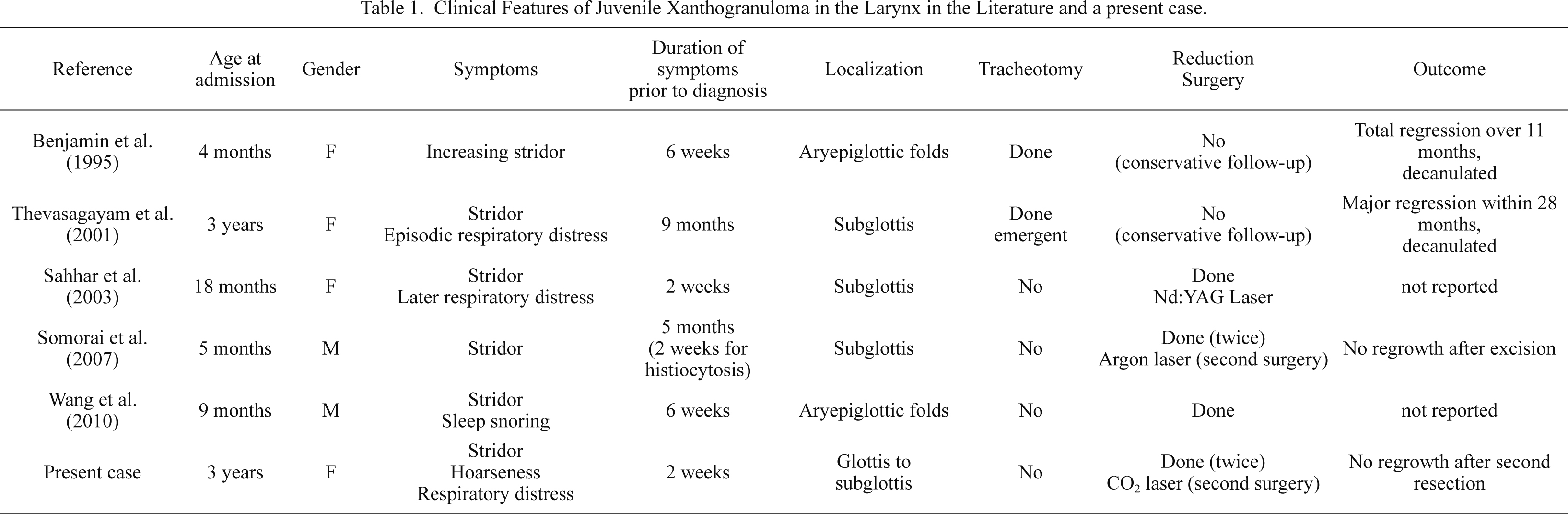
Clinical Features of Juvenile Xanthogranuloma in the Larynx in the Literature and a present case.
We have described the first reported juvenile patient with JXG involving the glottis. Many cases of JXG are benign histiocytosis and usually regress spontaneously. In the present case, no tumor enlargement has been observed after two reduction operations using laryngomicrosurgery. Immunohistochemistry using antibodies against CD1a, Factor XIIIa and S-100 protein is useful for diagnostic distinction of JXG from LCH, which has a poorer prognosis. In view of the benign nature of JXG, tumor reduction without tracheotomy is recommended for resolution of airway distress if endotracheal intubation is possible at surgery.
The authors declare no conflict of interest.