2013 年 230 巻 2 号 p. 83-86
2013 年 230 巻 2 号 p. 83-86
Low back pain (LBP) is one of the most common symptoms in outpatient clinics, and abdominal aortic aneurysm (AAA) is one of the causes of LBP. In the present study, we examined the prevalence of chronic LBP in patients with aortic aneurysm. The study included 23 patients with AAA and 23 patients with thoracic aortic aneurysm (TAA); all of them visited a regional center hospital in Akita, Japan. A total of 207 hypertension patients were also enrolled as a control. Chronic LBP was defined in patients who visited the orthopedic outpatient clinic for the LBP treatment for more than three months. The prevalence of chronic LBP in the AAA group (52.2%) was significantly higher than that in the TAA (17.4%, P < 0.05) or hypertension patients (11.6%, P < 0.01). The rate of a trigger point (TP) injection was significantly higher in the AAA group or the TAA group than that in hypertension patients (P < 0.01, P < 0.05), but there was no significant difference between the AAA and TAA groups. The TP injection represents an injection of local anesthesia to the low back muscles. We also evaluated the involvement of various factors in LBP caused by AAA, such as age, gender, blood pressure, the existence of dissection, and the maximum diameter of AAA, but none of them showed significant relationship to LBP. The prevalence of LBP is high in AAA patients, and doctors who treat chronic LBP should be aware of AAA as a potential cause of LBP.
Low back pain (LBP) is one of the most common symptoms reported in outpatient clinics, with various causes being suggested for LBP. Although most causes originate from the lumbar region or muscles around it, the cause in about 8% of patients with LBP is due to non-mechanical spinal conditions or visceral disease, such as kidney urological diseases and gynecological diseases (Javik and Deyo 2002). Abdominal aortic aneurysm (AAA), which is defined as an aortic artery diameter exceeding 3.0 cm, is one of the causes of LBP (Javik and Deyo 2002).
Patients with acute aortic dissection or ruptured AAA develop sudden and strong LBP or gripe. These diseases need to be diagnosed early because of their high risk for survival. However, the correct diagnosis is sometimes delayed because of the misdiagnosis of lumbar or muscular diseases when symptoms do not include gripe (Kanjanauthai and Kanluen 2009). Therefore, care must be taken when assessing AAA as one of diseases that develops LBP.
While classically reported symptoms associated with AAA include back and abdominal pain, 75% of patients with AAA are asymptomatic at the time of diagnosis (Edwards and Weiner 2003). Although the Japanese Orthopedic Association Clinical Practice Guidelines for the Management of Low Back Pain state that an aneurysm is one of the important causes of LBP (The Japanese Orthopedic Association 2012), its prevalence remains unclear. Several reports on AAA patients, not acute aortic dissection or ruptured AAA patients, exhibiting chronic LBP with an eroding vertebral body have shown that the erosion of an aneurysm into the vertebral body caused pain even in the absence of rupture (Prete et al. 1980; Nakagawa et al. 1990; Diekerhof et al. 2002). However, AAA causing chronic LBP without vertebral body erosion has also been observed, and it has been suggested that chronic LBP secondary to AAA may be due to the aneurysm itself (Mechelli et al. 2008). As such, the cause of LBP in AAA patients has not been clarified, and no report has examined the relationship between AAA and LBP.
The prevalence of LBP in aneurysm patients remains unknown. The aim of this study was to examine the prevalence and cause of chronic LBP in AAA patients.
This study included 46 consecutive patients with thoracic aortic aneurysm (TAA) or AAA, all of whom visited a regional center hospital in Akita, Japan between April 2002 and August 2012. All patients were found by internal medicine doctors using computed tomography (CT) when they were being examined for acute aortic dissection or other internal organ diseases; namely, the patients were not examined by orthopedic doctors who suspected the LBP origin. We defined TAA and AAA as an aortic artery diameter exceeding 4.5 cm and 3.0 cm, respectively. There were 26 males and 20 females, with a mean age of 77.6 years (49 to 94). We did not include patients who were evaluated by CT only prior to death due to acute aortic dissection or ruptured AAA and only after surgery for an aortic aneurysm. We divided patients into 2 groups, one with AAA patients (AAA group) and the other without AAA patients (TAA group). The TAA group included 23 patients consisting of 11 males and 12 females with a mean age of 78.2 years (49 to 94), and the AAA group included 23 patients consisting of 15 males and 8 females with a mean age of 77.0 years (61 to 92) (Table 1). Forty-two patients (91.3%) were treated with hypotensive drugs.
As a non-aneurysmal control group, the study included 207 consecutive patients with hypertension (HT group) without TAA and AAA, confirmed by CT and followed by doctors of internal medicine in our hospital between July 2002 and August 2012. There were 111 males and 96 females, with a mean age of 75.7 years (45 to 94) (Table 1).
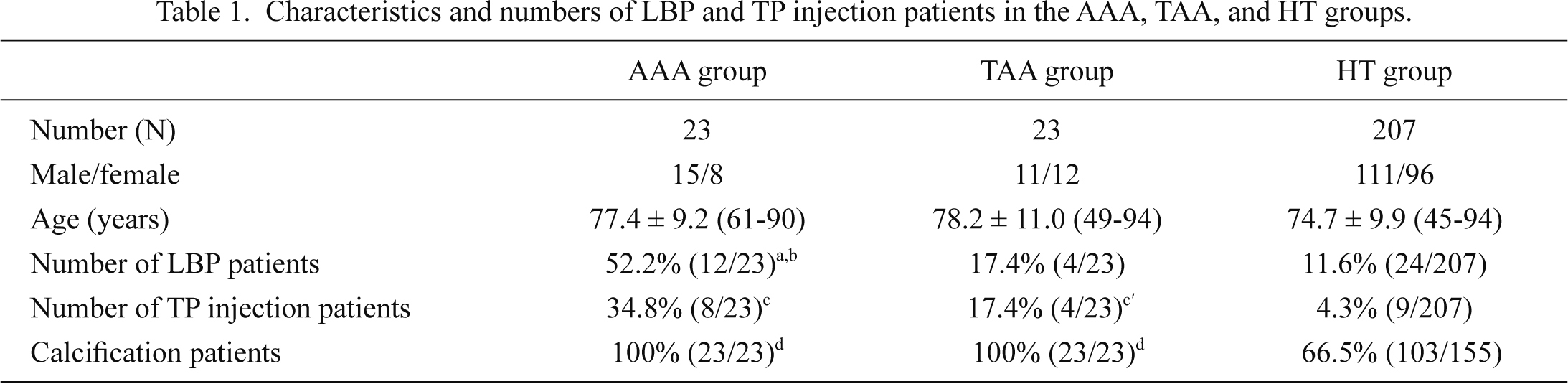
Characteristics and numbers of LBP and TP injection patients in the AAA, TAA, and HT groups.
Values are expressed as the number of patients or mean ± s.d. with the ranges in parentheses.
aP < 0.05 vs. the TAA group.
bP < 0.01 vs. the HT group.
cP < 0.01 and c′P < 0.05 vs. the HT group.
dP < 0.05 vs. the HT group.
Because chronic LBP is defined as LBP that continues for more than three months, we selected patients who visited our orthopedic outpatient clinic for the treatment of LBP for more than three months from the most recent CT evaluation of aortic aneurysm (Chou et al. 2007). We excluded patients with obvious spinal disorders, such as those with spinal compression fractures, lumbar herniated intervertebral discs, spinal canal stenosis, spondylolisthesis, tumors, and infection. We also excluded patients who could not walk by themselves, because burden on the waist was different between the patients who could walk and those who could not walk.
Assessment of chronic LBP and its factorsWe compared the prevalence of chronic LBP between the AAA group and the TAA or HT control group. We also compared the rate of patients who underwent a trigger point (TP) injection for LBP among the three groups. The TP injection is one of LBP treatments, and an injection of local anesthesia to the low back muscles to relieve LBP is often performed in LBP patients. We compared the prevalence of abdominal aortic calcification among the three groups and the prevalence of chronic LBP between calcification and non-calcification patients in the HT group because atherosclerosis of the lumbar arteries causing circulatory disturbances to the lumbar muscles and discs may cause LBP (Kaupplia and Tallroth 1993; Kaupplia et al. 1997; Kurunlahti et al. 1999). We also evaluated various suspected factors that may be related to chronic LBP caused by AAA, such as age, gender, systolic pressure, diastolic pressure, the existence of dissection, the maximum diameter of AAA including the dissection space, and the diameter of AAA excluding the dissection space (Fig. 1). We used the average data from 5 measurements of systolic and diastolic pressures from the most recent CT evaluation of the aortic aneurysm at the outpatient clinic.
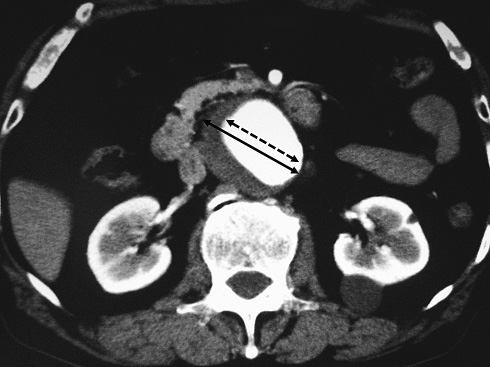
CT imaging of a patient with AAA.
White area of AAA is an intravascular space and black area is a dissection space. A symmetrical arrow indicates the maximum diameter of AAA, and a symmetrical dotted arrow indicates the diameter of AAA excluding the dissection space.
All values are expressed as the mean ± s.d. A one-factor analysis of variance (ANOVA) was used to test for significance. The difference in age between the AAA group and the TAA group or the HT group was compared using the Kruskal-Wallis rank-sum test for multiple comparisons. The Mantel-Haenszel χ2 test was used to compare gender among the three groups. This statistics method was also used to compare the prevalence of chronic LBP, rate of patients receiving the TP injection, the prevalence of abdominal aortic calcification, and the prevalence of chronic LBP between calcification and non-calcification patients. Multivariate logistic regression analysis was used to examine the factors of chronic LBP caused by AAA. P values less than 0.05 were considered significant.
There was no significant difference in age or gender among the AAA, TAA, and HT groups. There was no case of an eroding vertebral body at the CT examination.
The prevalence of chronic LBP in the AAA group was significantly higher than that in the TAA and HT groups (Table 1, P < 0.05, P < 0.01). The percentage of patients undergoing TP injection in the AAA and TAA groups was significantly higher than that in the HT group (P < 0.01, P < 0.05), but there was no significant difference between the AAA and TAA groups. The prevalence of abdominal aortic calcification in the HT group was significantly lower than that in the AAA and TAA groups (Table 1, P < 0.05, P < 0.05), but there was no significant difference between the AAA and TAA groups. There was no significant difference in the prevalence of chronic LBP between calcification and non-calcification patients in the HT group. Multivariate logistic regression analysis indicate that none of factors is related to chronic LBP caused by AAA (Table 2)
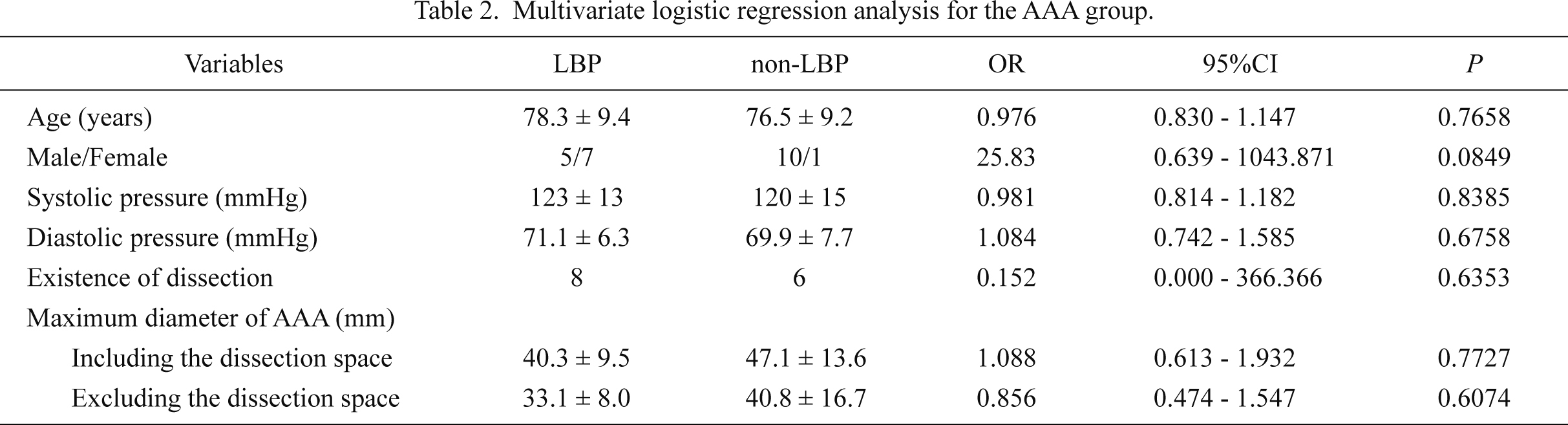
Multivariate logistic regression analysis for the AAA group.
OR, odds ratio; 95%CI, 95% confidence interval.
OR and 95%CI of Male/female represent values for females.
Values are expressed as the number of patients or mean ± s.d. with the ranges in parentheses.
In this study, the prevalence of chronic LBP and the TP injection in the AAA group were significantly higher than those in the HT group. In addition, the prevalence of chronic LBP in the AAA group was significantly higher than that in the TAA group; therefore, we suggest that the existence of an aortic aneurysm in the abdomen is responsible for chronic LBP. In fact, more than half of the AAA patients underwent treatment for chronic LBP; namely, a high rate of chronic LBP was observed in AAA patients. Therefore, there seems to be some kind of relationship between AAA and chronic LBP. However, we could not distinguish differences in the symptom features of LBP arising from AAA and other LBP in this study. It is also possible that LBP patients not arising from AAA may be included to the AAA group, because we do not know the features of LBP arising from AAA. Although chronic LBP is one of the most frequent symptoms in orthopedic surgery, we should note that LBP patients, especially the elderly, might suffer from AAA.
In this study, none of the patients with AAA exhibiting chronic LBP showed an eroding vertebral body; therefore, there may be other causes of LBP aside from an eroding vertebral body. Possible factors of chronic LBP in patients with AAA include the size of the aortic aneurysm causing direct stress to the surrounding tissues, poor blood pressure control resulting in pressure on the vascular wall, and the existence of AAA dissection. However, these factors did not have any relationship to chronic LBP in this study. In addition, there has been no report on the causes of LBP in AAA patients; therefore, the actual causes of LBP in these patients remain unclear.
Atherosclerosis of the lumbar arteries and middle sacral artery has been reported to cause circulatory disturbances and decreased nutrient supply to the lumbar muscles and discs, which may cause LBP (Kaupplia and Tallroth 1993; Kaupplia et al. 1997; Kurunlahti et al. 1999). The calcification of aneurysms was shown in all AAA patients in this study, and that in the AAA group was seen more often than that in the HT group. Therefore, patients in the AAA group may exhibit calcification of the lumbar arteries and middle sacral artery more than HT patients, which may account for the high rate of LBP in the AAA group. However, LBP has been ascribed to a disturbance in blood supply to the lumbar tissues through collateral circulation from the lower extremities with a circulatory disturbance in the lumbar arteries, and only a circulatory disturbance in the lumbar arteries did not result in LBP (Takeyachi et al. 2006). In the present study, a disturbance in blood supply to the iliac arteries was not detected in all AAA patients, but we could not identify the lumbar arteries and middle sacral artery from the CT images used to evaluate AAA in our hospital. As such, we were unable to determine whether a disturbance in these arteries may have affected LBP; therefore, higher quality images are needed to resolve these theories.
A limitation of this study was the small number of AAA patients who matched the inclusion criteria of this study. Many AAA patients are asymptomatic, and AAA is mostly found by chance in these patients. Therefore, the number of AAA patients who receive medical treatment, but have not undergone surgical treatment, in the outpatient clinic is limited. Although we should set the same observation period for the AAA and TAA groups as that for the control group, it was impossible because of the small number of patients. Non-LBP patients also did not receive lumbar radiographs; therefore, we could not evaluate spinal deformations.
In conclusion, to the best of our knowledge, the present study is the first to examine the prevalence of chronic LBP in AAA patients. The prevalence of LBP is about 50% in AAA patients, and doctors who treat chronic LBP should be aware of AAA as a potential cause of LBP. However, since the pathogenesis of LBP in AAA patients has not yet been clarified, we need to perform further studies with a larger number of AAA patients and more detailed analyses including spinal images.
The authors declare no conflict of interest.