2013 年 230 巻 2 号 p. 97-102
2013 年 230 巻 2 号 p. 97-102
Lipoprotein-associated phospholipase A2 (Lp-PLA2) is an enzyme that hydrolyzes oxidized phospholipids to generate bioactive proatherogenic products. Nonculprit lesions have been assumed to contribute to the pathogenesis of recurrent acute coronary syndrome (ACS). The role of LP-PLA2 in the progression of nonculprit coronary lesions after successful percutaneous coronary intervention (PCI) remains unclear. Our study included 123 patients with ACS who underwent initial PCI and a long-term follow-up (mean interval, one year) with coronary angiography. Among them, 19 patients were diagnosed as the progression of nonculprit lesions, based on the presence of at least one of the following factors: (1) ≥ 10% reduction in the diameter of a preexisting ≥ 50% stenosis; (2) ≥ 30% reduction in the diameter of a < 50% stenosis; and (3) early-onset stenosis with ≥ 30% reduction in the diameter of a segment that was normal on the primary angiogram. Blood sampling was drawn from all patients at 12-14 hours after PCI. The ACS patients with progression had higher total cholesterol (4.47 ± 1.02 mmol/L vs. 3.59 ± 0.57 mmol/L, P < 0.05), higher levels of Lp-PLA2 activity (14.39 ± 6.13 nmol/min/ml vs. 8.86 ± 3.14 nmol/min/ml, P < 0.001) and a higher proportion of multi-vessel disease than those without progression. Multivariate logistic regression analysis showed that Lp-PLA2 activity (β = 0.024, P = 0.005) was an independent predictor for rapid progression of nonculprit coronary lesions. In conclusion, elevated Lp-PLA2 activity is associated with rapid progression of nonculprit coronary lesions in ACS patients who underwent PCI.
Percutaneous coronary intervention (PCI) has now become an effective reperfusion and widespread treatment for the culprit lesions in patients with acute coronary syndromes (ACS). Although PCI can be used successfully for all coronary stenoses, a substantial proportion of cases had unanticipated and recurrent major adverse cardiovascular events associated with untreated/nonculprit coronary lesions (Stone et al. 2011). Studies have reported that one or more angiographically nonculprit coronary artery stenoses were involved in the higher incidence of heart failure, recurrent ACS and need for further revascularization (Goldstein et al. 2000; Lee et al. 2004; Kim et al. 2006). Thus, the characteristic assessment of nonculprit coronary artery lesions after primary PCI could improve risk stratification and detect residual myocardial ischemia. Efforts to detect the nonculprit lesions have been ongoing and measurements of levels of biomarkers have become important tools in the early identification of nonculprit plaque.
Lipoprotein-associated phospholipase A2 (Lp-PLA2), known as a novel inflammatory marker, was involved in bioactive lipid formation and the pathogenesis of atherosclerosis as well as coronary artery disease (CAD) (Kim et al. 2008). Clinical studies demonstrated that Lp-PLA2 was present in thin-cap fibroatheromas and necrophages of human ruptured plaques and colocalized with macrophages (Häkkinen et al. 1999; Kolodgie et al. 2006). However, the potential role of Lp-PLA2 in the formation of atherosclerotic lesions and the anti- or pro-atherogenic characteristic of this enzyme in humans remains to be established (McConnell and Hoefner 2006). In addition, several clinical studies have investigated the influence of Lp-PLA2 on angiographically proven CAD, but the results are not conclusive (Caslake et al. 2000; Khuseyinova et al. 2005; Brilakis et al. 2005; Winkler et al. 2005).
Previous studies have shown that inflammation plays a pivotal role in the development of atherosclerosis and inflammatory factors such as C-reactive protein (CRP) are involved in the progression of nonculprit lesions (Nakachi et al. 2008; Otake et al. 2008). To the best of our knowledge, no studies have explored the relationship between activity of Lp-PLA2 and rapid angiographic progression of nonculprit lesions in patients after PCI. In the present study, the progression of nonculprit lesion was diagnosed according to the previous studies (Zouridakis et al. 2001; Nakachi et al. 2008). We measured plasma Lp-PLA2 activity in ACS patients who underwent successful initial PCI for a clearly identified culprit lesions. We also tried to correlate Lp-PLA2 with anthropometric parameters and the progression of nonculprit lesions.
Our study is comprised of 123 patients (36 females, 62.7 ± 8.3 years of age) with ACS who underwent with primary PCI from January 2008 to December 2009 in Affiliated Hospital of Medical College, Qingdao University. Patients were included if they fulfilled acute ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI) or unstable angina. All participants received secondary coronary angiography at the mean one-year angiographic follow-up. All participants had completed a questionnaire on present condition, family and medical histories of cardiovascular risk factors and complications, clinical examination and ECG recording. Informed consent was obtained from all patients based on a protocol approved by the Ethics Committee of Affiliated Hospital of Medical College, Qingdao University.
Clinical and biological assessmentThe details of age, gender and the weight and height were obtained, with the body mass index (BMI) calculated as the body weight in kilograms divided by the height in meters squared. Waist circumference was measured at the level of the umbilicus, systolic and diastolic blood pressures were obtained with a mercury sphygmomanometer using auscultory methods. Furthermore, fasting blood sample was collected from all patients 12-14 hours after PCI to determine the triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-c), high-density lipoprotein cholesterol (HDL-c), creatinine (Cr), blood urea nitrogen (BUN), fasting blood glucose (FBG), and uric acid (UA). The normal ranges of values that are currently being used in our hospital laboratory for various parameters were: triglycerides 0.50-1.80 mmol/L, total cholesterol 3.23-6.47 mmol/L, low-density lipoprotein cholesterol 0.00-3.37 mmol/L, high-density lipoprotein cholesterol 0.90-1.68 mmol/L, creatinine 53.0-115.0 umol/L, urea nitrogen1.70-8.30 mmol/L, fasting blood glucose 3.9-6.1 mmol/L and uric acid 119-417 µmol/L. Blood samples were obtained in EDTA collection tubes at the time of PCI, centrifuged at room temperature (1,500 × g) for 15 min, and stored at −80°C, until Lp-PLA2 activity was measured. The total plasma Lp-PLA2 activity was measured using a PAF Acetylhydrolase enzyme immunoassay (EIA) kit (Catalogue No. 760901, Cayman chemical Company, USA). The ranges of Lp-PLA2 activity were 0.02-0.2 nmol/min/ ml.
Angiographic analysisCoronary angiography was performed in all patients (immediately after admission in STEMI and within 24 h after admission in NSTEMI or unstable angina) and confirmed the presence of at least 1 culprit coronary lesion. All patients underwent primary coronary angiography and/or PCI with standard techniques and a transfemoral approach at admission, and follow-up diagnostic angiography (second coronary angiography) was performed at a median follow-up of one year for all participants. Diagnostic and follow-up images of coronary tree were obtained in routine standardized projections with a Bicor-Plus system (SIEMENS) and recorded as appropriate. Similar to the previous research (Bertrand et al. 1993), quantitative angiographic measurements were performed to evaluate the images of coronary tree by one experienced interventional cardiologist. We derived the reference diameter and minimal lumen diameter (in millimeters) of each lesion at the dilated site. The percent reduction of stenosis diameter was calculated at the most severe lesion after initial angioplasty immediately and at follow-up angioplasty. The late loss (minimal lumen diameter immediately after PCI minus minimal lumen diameter at follow-up angioplasty) was measured for nonculprit lesions. Nonculprit vessels with < 50% visible diameter stenosis and nontarget lesions of culprit vessels with < 50% visible diameter stenosis were investigated.
Criteria of progression of nonculprit lesionsNonculprit lesion progression was diagnosed as previously reported (Zouridakis et al. 2001; Nakachi et al. 2008) at least one of the following factors were present: (1) ≥ 10% reduction in the diameter of a preexisting ≥ 50% stenosis; (2) ≥ 30% reduction in the diameter of a < 50% stenosis; and (3) early onset stenosis with a ≥ 30% reduction in the diameter of a segment that was normal on the primary angiogram.
Statistical analysisStatistical analyses were performed with SPSS 15.0 (SPSS Inc., Chicago, Illinois) software. Data are presented as mean ± s.d. for continuous variables and as proportions for categorical variables. After testing for normal distribution of variables, student’s 2-tail t-test was used for continuous variables to assess differences between groups. Categorical variables were compared using the chi-square test (Fisher’s exact text was used when applicable). The correlations between two variables were assessed by Pearson correlation analysis. Multiple linear regression analysis was used to evaluate the contribution of independent factors. A two-tailed P value < 0.05 was considered statistically significant.
During a follow-up period of mean one year, the secondary coronary angiograms showed that 19 of 123 patients (15.4%) had rapid progression of nonculprit lesions; there were 10 patients (8.13%) required a new revascularization procedure with a nonculprit restenosis of at least 70%. ACS patients were further divided into two subgroups according to the presence or absence of progression of nonculprit lesions. The progression group consisted of 19 patients while the non-progression group consisted of 104 patients. The progression was defined as that at least one lesion showed progression.
Baseline characteristicsThe baseline clinical and biochemical characteristics of the patients with ACS on admission are summarized in Table 1. There were no statistical differences in age, sex, BMI, systolic blood pressure, diastolic blood pressure, fasting blood glucose, insulin, triglycerides, LDL-c, HDL-c and uric acid between two subgroups (P > 0.05 for all). However, when compared with patients without progression, total cholesterol was significantly increased in patients with progression (4.47 ± 1.02 mmol/L vs. 3.59 ± 0.57 mmol/L, P < 0.05). The levels of Lp-PLA2 activity were significantly higher in ACS patients with progression than those without progression (14.39 ± 6.13 nmol/min/ml vs. 8.86 ± 3.14 nmol/min/ml, P < 0.001).

Baseline clinical and biochemical characteristics of the ACS patients.
Data are means ± SEM. *P < 0.05, **P < 0.001 compared to ACS without progression.
BMI, body mass index; Cr, creatinine; DBP, diastolic blood pressure; HDL-c, high-density lipoprotein cholesterol; LDL-c, low-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TG, triglycerides; UA, uric acid.
The patients’ angiographic and procedural characteristics of primary PCI and follow-up phase are presented in Table 2 and Fig. 1. At primary PCI, the degree of significant multi-vessel coronary arteries disease (defined as ≥ 2-vessel disease with diameter stenosis ≥ 50%) was higher in the progression group than in the non-progression group (P < 0.001). At follow-up PCI, the mean minimal lumen diameter of nonculprit stenosis was significantly reduced in patients with progression than those without progression (0.31 ± 0.30 mm vs. 0.49 ± 0.32 mm, P < 0.05). The percent of stenosis diameter was increased from 12% to 45% in the nonculprit progressing lesions with reaching statistical significance. The late loss in minimal lumen diameter was also significantly greater at nonculprit lesions in the progression group when compared to the group without progression (0.68 ± 0.60 mm vs. 0.39 ± 0.78 mm, P < 0.05).
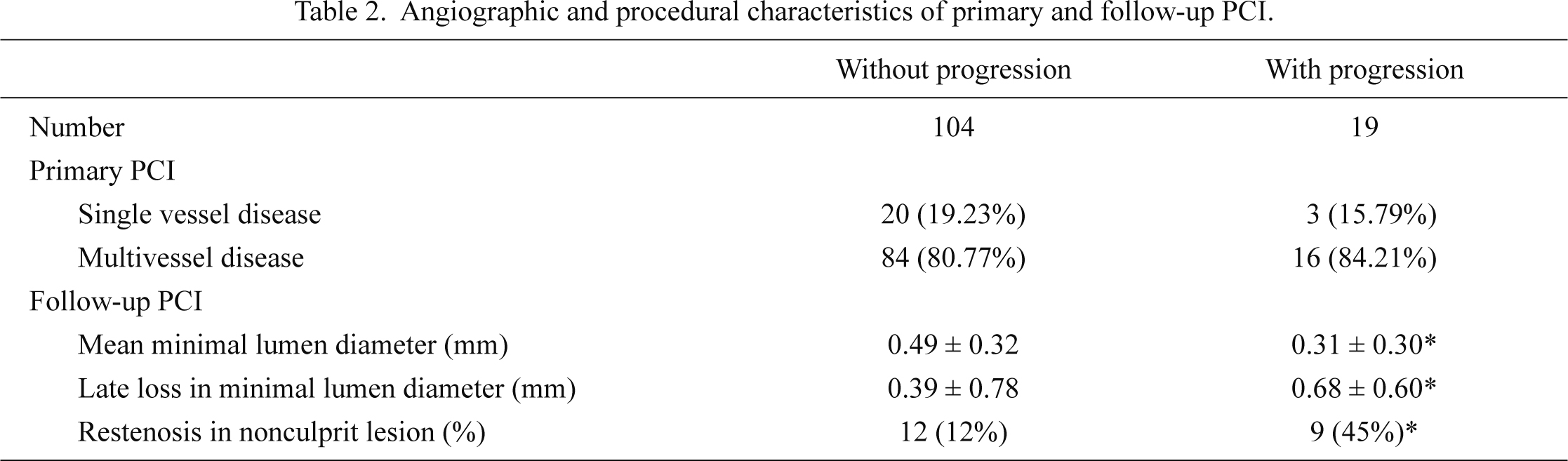
Angiographic and procedural characteristics of primary and follow-up PCI.
Data are means ± SEM. *P < 0.05 compared to ACS without progression.
PCI, percutaneous coronary intervention.
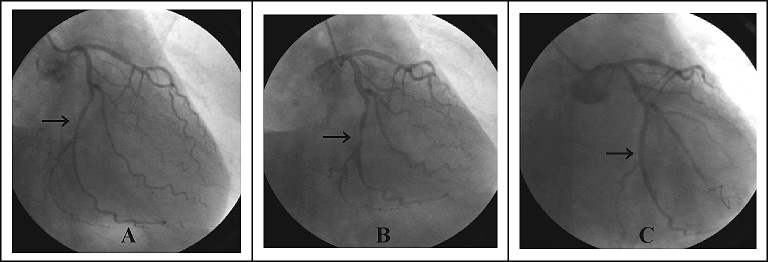
Coronary angiography characterization of one nonculprit lesion in left circumflex artery.
A: The left circumflex artery’ angiographic characteristics at primary PCI. An arrow indicates a nonculprit lesion in left circumflex artery. B: Secondary angiography showed almost total occlusion of a nonculprit lesion at one-year follow-up. C: One stent was implanted with successful additional revascularization.
In order to identify a parameter that reflects Lp-PLA2 activity, linear regression analysis was performed to examine the relationship of Lp-PLA2 activity and other biomarkers in patients with ACS. Lp-PLA2 activity correlated significantly with age (r = 0.658, P = 0.044), diastolic blood pressure (r = 0.800, P = 0.025), BMI (r = 0.951, P = 0.009) and triglycerides (r = 0.845, P = 0.020). Furthermore, multivariate logistic regression analysis was used to investigate the influence of Lp-PLA2 and conventional risk factors on progression of nonculprit lesions. Lp-PLA2 activity (β = 0.024, P = 0.005) was identified as one independent predictor for the progression of nonculprit lesions in patients with ACS after adjustment for age, gender, hypertension, dyslipidemia and glucose.
In the present study, we demonstrated that a large cohort of patients underwent primary PCI (in 15.4% of patients) for culprit lesions had nontarget lesion progression within the first post-procedure year of follow-up. Furthermore, a total of 10 (at least 1 lesion with ≥ 50% stenosis) of these patients went through additional revascularization. Another striking finding was that high levels of Lp-PLA2 activity were associated with rapid angiographic progression of nonculprit lesions after initial PCI in the setting of ACS.
Growing lines of evidence have shown that one or more angiographically nonculprit stenoses were involved in the higher incidence of heart failure, recurrent ACS and need for further revascularization (Goldstein et al. 2000; Lee et al. 2004; Kim et al. 2006). Sorajja et al. (2007) indicated that revascularization of nonculprit stenoses can improve survival within the first month after the acute myocardial infarction. In patients with angina pectoris, Kaski et al. (1995) revealed that 24% of patients had angiographic progression at a median follow-up of 8 months and 28% of culprit lesions progressed while 9% of nonculprit lesions progressed. Of those patients, 57% suffered acute coronary events with lesion progression. In a retrospective cohort study, Glaser et al. (2005) found that approximately 6% of PCI patients had clinical plaque progression needing for nontarget lesion PCI within one year. In our study, of 19 patients (15.4%) who had nontarget lesions progression within the primary PCI procedure 1 year, 10 patients (8.13%) were related to nonculprit vessels requiring PCI of a new stenotic lesion. The discrepancy between the studies may be explained by differences in the use of statin, β-blockers and antiplatelet agents in patients with original PCI (Glaser et al. 2005).
Several studies have investigated that inflammation may play a crucial role in progressive instability in other areas of the coronary artery after initial PCI, but data from these observations were conflicting. Caslake et al. (2000) reported that plasma Lp-PLA2 levels were significantly elevated in patients with CAD and appeared to be an independent predictor of angiographically proven CAD. In line with the results of Khuseyinova et al. (2005), Brilakis et al. (2005) found that higher quartile of Lp-PLA2 was associated with the presence of CAD events. On the contrary, the Ludwigshafen Risk and Cardiovascular Health Study found that Lp-PLA2 activity was not an indicator of the systemic inflammation in subjects with ACS (Winkler et al. 2005). In the current study, we found that Lp-PLA2 activity was elevated in ACS patients with nonculprit progression. Furthermore, in multiple stepwise regression analysis, Lp-PLA2 activity was identified as the independent factor that influences rapid progression of nonculprit lesions after PCI, even adjustment for age, gender and traditional cardiovascular risk factors. Our results extended potential role for Lp-PLA2 activity in patients with angiographically proven CAD who underwent PCI for culprit lesions.
The biological mechanisms involving elevated Lp-PLA2 activity in the angiographic progression of nonculprit lesions noted after PCI are not well characterized. Several characteristics of Lp-PLA2 suggest that this enzyme may be independently relevant to the progression of nonculprit lesions in ACS patients underwent PCI. Recent studies have suggested that Lp-PLA2 is a vascular-specific proinflammatory enzyme operated physiologically in the arterial intima and expressed in human and rabbit atherosclerotic plaques (Häkkinen et al. 1999; Toth et al. 2010). In the Ludwigshafen Risk and Cardiovascular Health Study, elevated Lp-PLA2 activity was associated with angiographic CAD independently of established risk factors, especially LDL-c (Winkler et al. 2005). Meanwhile, Lp-PLA2 is preferentially secreted by macrophage and hydrolyzed chemoattractants could contribute to development of atherosclerotic lesions and CAD through inflammatory reactions in the arterial intima (Hatoum et al. 2010). Atherosclerosis is now recognized as manifestations of vascular inflammation and a progressive disease (Ross 1999). The trauma associated with the diagnostic part of the PCI procedure may trigger an inflammatory response (Nakachi et al. 2008).
Additionally, the correlations between Lp-PLA2 activity and anthropometric determinants may be complementary explanations for influence of Lp-PLA2 activity on angiographic progression of nonculprit lesions in this study. Our results demonstrated that there was an association between Lp-PLA2 activity and age, BMI, diastolic blood pressure as well as triglyceride. These anthropometric factors would contribute to an increase in Lp-PLA2 activity was not unexpected due to the interrelationship among age, obesity, high blood pressure and hypertriglyceridemia. Furthermore, these observations were consistent with the adaptative mechanism that Lp-PLA2 activity increased with age and accelerated age-dependent vascular wall damage (Yamada et al. 2000). Obesity may have been responsible for the changes of Lp-PLA2 involved in the progression of nonculprit lesions. Adipose tissue is likely to be infiltrated by macrophages, which is an important cause of the inflammatory state associated with obesity (Rana et al. 2011). As opposed to the findings of Tsimikas et al. (2009), we noted the positive association between Lp-PLA2 activity and hypertension. These findings also differed from the results of Blankenberg et al. (2003), who found that the Lp-PLA2 levels were diminished in cases of CAD patients with hypertension when compared with nonhypertensive patients. Finally, in the present study, triglyceride was also associated with Lp-PLA2 activity, a finding that has been observed previously (Noto et al. 2006).
Some limitations of this study need to be considered. Our results are based on single measurements of circulating Lp-PLA2, which may not reflect the true activity of Lp-PLA2 over time or true expression in atherosclerotic lesions. Thus, further outcome-directed prospective studies would give insight into the significance of Lp-PLA2 activity versus expression in atherosclerotic plaques. Secondly, when the occlusion can be crossed with a guide wire during the initial PCI, the plaques and the vessel wall may be injured and potentially triggered rapid progression of nonculprit lesions. Thirdly, the coronary angiography widely used in clinical practice as diagnostic tool is a “lumenogram” and provides no information regarding phenomena that occur within the vessel wall (Nakachi et al. 2008). In our study, intravascular ultrasonography or angioscopy was not used to assess all branches that are visible angiographically, as they can provide more accurate information regarding atherosclerotic plaques than angiography. Finally, results obtained in further confirmatory studies need to be considered to clarify the validity of Lp-PLA2 in large series of patients undergoing PCI.
In conclusion, the results of this study suggest that about 9% of the nonculprit stenoses may be revascularized at mean follow-up of one year after initial PCI. As an augmented inflammatory response to interventions, elevated Lp-PLA2 activity is a predictive marker and may contribute to the rapid progression of nonculprit lesions in patients with ACS who underwent PCI procure.
This work was supported by the key science and technology program of Shandong Province of China (No.: 2007GG3WZ02055), the natural science foundation of Shandong Province of China (No.: ZR2010HM134) and the national natural science foundation of China (No.: 81070086).
There are no conflict of interest to be declared.