2013 Volume 230 Issue 3 Pages 129-132
2013 Volume 230 Issue 3 Pages 129-132
Reflux gastroesophagitis is a common postgastrectomy complication after proximal gastrectomy, and conservative treatments including protease inhibitors and proton pump inhibitors are effective in most patients. Here we report a patient with severe reflux gastroesophagitis after proximal gastrectomy, in whom surgical treatment of duodenal switch was effective. An 80-year-old man complained of intractable heartburn, anorexia, and body weight loss after having undergone proximal gastrectomy, with reconstruction by esophagogastrostomy with valvuloplasty and pyloroplasty, for early gastric cancer 14 months before referral to our department. Oral administration of protease inhibitors and proton pump inhibitors was ineffective. Laboratory evaluation showed poor nutritional status. On endoscopic examination, we noted the redness, bleeding, and multiple erosions in the esophagus and the gastric remnant. He was diagnosed to have severe gastroesophagitis due to reflux of duodenal juice into the gastric remnant and esophagus. We performed duodenal switch to divert duodenal juice from the gastric remnant and esophagus; the duodenum was transected 2 cm distal to the pylorus, the duodenal distal end was closed, and a 50-cm Roux limb from the proximal jejunum was anastomosed to the proximal end of the duodenum. The heartburn disappeared postoperatively, and endoscopic examination revealed marked improvement of the reflux gastroesophagitis. One year postoperatively, the patient is free from symptoms including heartburn. His body weight increased, and laboratory data showed improvement in nutritional status. In conclusion, the duodenal switch may be surgical treatment of choice for intractable reflux gastroesophagitis after proximal gastrectomy.
Reflux gastroesophagitis is a common postgastrectomy complication. Proximal gastrectomy (PG) is performed in selected patients with early gastric cancer located in the upper portion, and reflux esophagitis is estimated to occur in 10-30% of patients undergoing PG (Ishii et al. 2006). The rate of occurrence of reflux esophagitis after PG is believed to be higher than that after total and distal gastrectomies (Ishii et al. 2006). While conservative treatments including protease inhibitors and proton pump inhibitors are effective in most patients with reflux esophagitis after PG, a few patients may require surgery. We report a patient with intractable reflux gastroesophagitis after PG in whom a duodenal switch was effective.
A 80-year-old man was referred to our department for surgical treatment of intractable heartburn and anorexia after having undergone PG for early gastric cancer at another hospital 14 months before referral to our department. Reconstruction of the alimentary tract was by esophagogastrostomy with valvuloplasty and pyloroplasty (Matsushiro et al. 1986). The remnant stomach was vagally-denervated because of perigastric lymph node dissection. Preoperatively he did not have symptoms suggestive of gastroesophageal reflux disease, and preoperative gastroduodenal ensdoscopy did not reveal inflammation in the esophagus and stomach. Heartburn developed postoperatively and persisted, and a diagnosis of severe bile reflux esophagitis was made. Oral administration of protease inhibitors and proton pump inhibitors did not relieve his symptoms. Over the next year, he complained of anorexia and his body weight decreased from 50 to 40 kg. Laboratory evaluation showed poor nutritional status with albumin of 3.4 g/dL, hemoglobin of 10.0 g/dL, and total lymphocyte count of 680 /µL. A barium meal study revealed a marked reflux of barium into the esophagus, and the size of the gastric remnant was estimated as almost 1/2 of the original stomach (Fig. 1). On endoscopy at our institution, we noted the redness, bleeding, and multiple erosions in the esophagus, and he was diagnosed to have Grade C reflux esophagitis by the Los Angeles classification (Fig. 2A). There were similar findings in the gastric remnant (Fig. 2B). Mean intragastric and intraesophageal pH was 7.42 and 7.81, respectively, on 24-hour pH measurement. On computed tomography (CT), circumferential thickening of the esophageal wall was present close to the anastomosis. Staples used for the esophagogastrostomy in the previous operation were identified behind the heart in the thoracic cavity. There were no findings suggestive of recurrence or metastases of the gastric cancer.
Because of intractable symptoms, severe body weight loss, and reflux of duodenal juice containing bile and pancreatic juice into the esophagus, operative intervention was necessary. We decided to perform duodenal switch to divert duodenal juice from the gastric remnant. After laparotomy with upper midline incision in about 20 cm length, the duodenum was transected 2 cm distal to the pylorus, and the duodenal distal end was closed without transecting right gastric and gastroepiploic arteries. A 50-cm Roux limb from the proximal jejunum was anastomosed end-to-end to the proximal end of the duodenum (Fig. 3). Operative time was 192 minutes, and intraoperative blood loss was 370 g. The heartburn disappeared, and endoscopic examination performed 17 days after the operation revealed marked improvement of the reflux gastroesophagitis (Fig. 2C and D). Although return of gastric emptying was delayed for 7-10 days, he discharged 42 days postoperatively. One year postoperatively, the patient is free from symptoms including heartburn, and there were no findings suggestive of inflammation in the gastric remnant and esophagus on endoscopic examination. His body weight increased from 40 to 42 kg, and laboratory data showed increase in albumin of 3.8 g/dL, hemoglobin of 10.8 g/dL, and total lymphocyte count of 1,140 /µL.
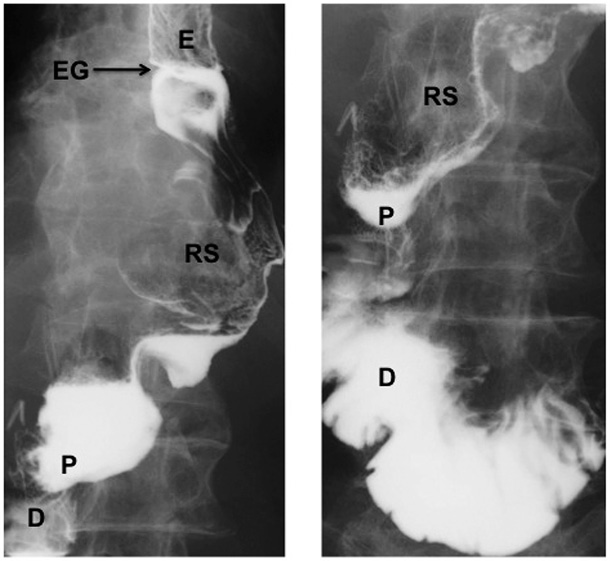
Barium meal study before duodenal switch.
Barium meal study revealed a marked reflux of barium into the esophagus, and the size of the gastric remnant was estimated as almost 1/2 of the original stomach. E: esophagus, EG: esophagogastrostomy, RS: residual stomach, P: pylorus, D: duodenum.
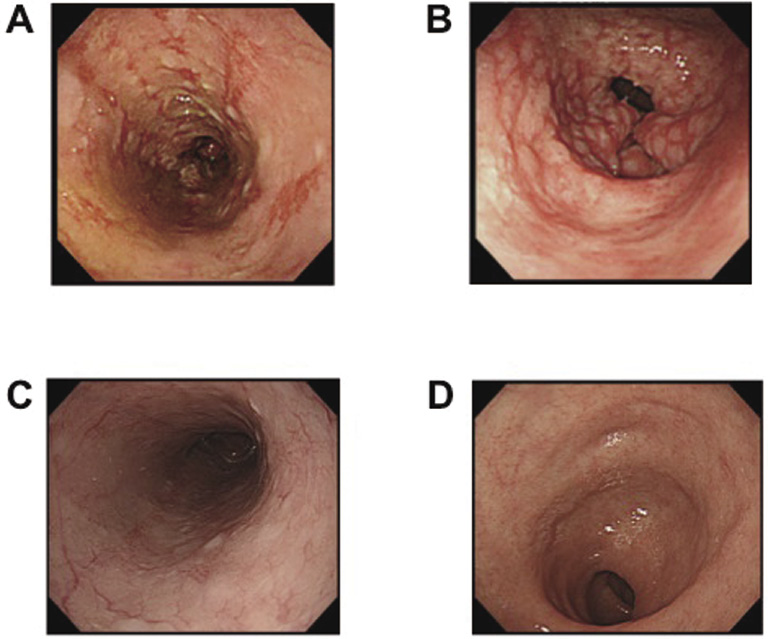
Upper gastrointestinal endoscopic findings.
Preoperative endoscopic examination revealed redness, bleeding, and erosions in the esophagus (A) and stomach (B). Inflammation improved markedly after duodenal switch in the esophagus (C) and stomach (D).
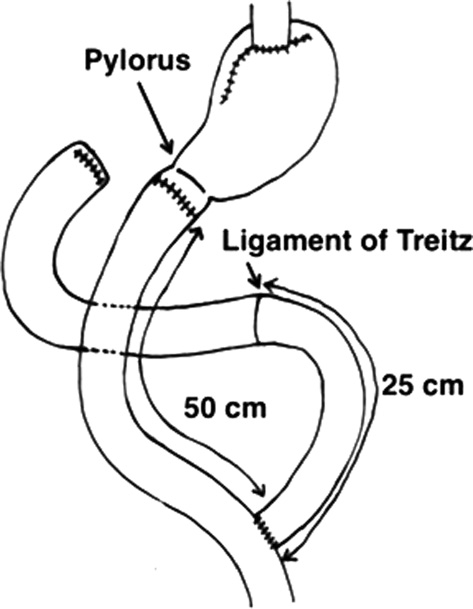
Schema of duodenal switch procedure after PG.
The duodenum was transected 2 cm distal to the pylorus, and the duodenal distal end was closed. A 50-cm Roux limb from the proximal jejunum was anastomosed end-to-end to the proximal end of the duodenum.
The excessive reflux of duodenal content into the stomach has been referred to as “duodenogastric reflux (DGR).” DGR is most of the time secondary to previously performed gastric surgery in which the pylorus was removed or rendered dysfunctional, while DGR without previous gastric surgery is called primary DGR (Klinger et al. 1999; Strignano et al. 2007). DGR is considered to be responsible for persistent symptoms after cholecystectomy (Wilson et al. 1995), and thus very important as a cause of postoperative symptoms.
Severe gastroesophagitis in our patient was considered to be associated with DGR due to pyloroplasty, and resection of the esophageal sphincter in PG further caused reflux of duodenal content into the esophagus. In theory, protease inhibitors can be effective in neutralizing activity of protease activity in duodenal content. In patients in whom gastric acid secretion is preserved because of large size of the gastric remnant, reflux of gastric acid could be another cause of the esophagitis, and proton pump inhibitors are usually effective in those patients (Ishii et al. 2006; Takahashi et al. 2008). In our patient, the gastric remnant was small, and the esophagitis was considered to be secondary to alkaline reflux and not associated with reflux of gastric acid. In deed, neither proton pump inhibitors nor protease inhibitors were effective. In Gastric Cancer Treatment Guidelines in Japan (2010), PG is indicated for patients with early gastric cancer located at the upper thirds of the stomach. We believe that PG should be performed when the gastric remnant is estimated to be greater than 2/3 of the original stomach and thus esophagogastromy is feasible. If the gastric remnant is considered less than 2/3 of the original stomach after PG, then reconstruction should be performed not by esophagogastrostomy but rather by interposition of a jejunal limb or inverted U-shaped jejunal pouch. Valvuloplasty and pyloroplasty after PG was proposed by Matsushiro et al. (1986) in an attempt to prevent reflux of intraluminal contents from the stomach into the esophagus. Although satisfactory clinical results have been reported after this procedure (Imaoka et al. 1991), the created valve did not function well in our patient.
A previous report suggested the following criteria of operative intervention for postgastrectomy intractable reflux esophagitis: 1) symptoms persistent for more than 6 months, and 2) patients having no evidence of recurrence of the gastric cancer (Ishii et al. 2006). Our patient fulfilled these criteria and also had serious body weight loss with anemia and hypoalbuminemia. Two procedures should be considered for intractable reflux esophagitis after PG. One procedure involves resection of the gastric remnant and reconstruction either with a Roux-en-Y anastomosis or an interposition of the jejunal segment, while the second procedure is designed to divert the pancreatobiliary secretions from the remnant stomach and esophagus. It was obvious from findings on CT that resection of the gastric remnant would require thoracotomy, which must be invasive for 80-year-old patient. Therefore, we decided to perform duodenal switch (DeMeester et al. 1987) as a surgical treatment for pathologic DGR.
A couple of studies reported the efficacy of duodenal switch for DGR secondary to gastric surgery, but these reports does not include patients after PG (DeMeester et al. 1987; Strignano et al. 2007). Roux-en-Y anastomosis is also effective to divert duodenal content after distal gastrectomy with Billorth-II anastomosis or vagotomy + pyloroplasty, or in patients with complex peptic esophagitis (Davidson and Hersh 1980; Cabrol et al. 1990; Fékété et al. 1997; Topart and Vandenbroucke 2001; Zobolas et al. 2006). Several other operations have been reported to divert duodenal juice for intractable reflux esophagitis after distal or total gastrectomy (Karaki et al. 1988; Aranow et al. 1995; Strignano et al. 2007). There has been one prior report in Japanese similar to ours performed for the reflux esophagitis after PG; their procedure involved resecting the pylorus (Karaki et al. 1988). Thus we believe this is the first report in which duodenal switch was performed for severe reflux gastroesophagitis after PG.
Duodenal switch after PG should be performed in patients with severe gastroesophagitis due to reflux of duodenal juice whose secretion of gastric acid is not preserved. We assured it based on results of intragastric and intraesophageal pH. Because duodenal switch does not improve gastroesophageal reflux, reflux esophagitis due to gastric acid may be persistent even after duodenal switch in patients with preserved gastric acid. Moreover, there is a risk of stomal ulcer after duodenal switch in patients whose secretion of gastric acid is preserved. In patients with severe reflux gastroesophagitis and preserved gastric acid, duodenal switch with resection of the pylorus might be of help for drainage of gastric acid into the distal portion to the stomach, and surgeons also should consider the use of proton pump inhibitors after duodenal switch.
In our patient, an end-to-end duodenojejunostomy was not difficult. If an end-to-end duodenojejunostomy is hard to do, a side-to-side gastrojejunostomy should be considered as an option. However, we have to take the fact into consideration that ligation and transection of branches of the right gastroepiploic artery, performed as a preparation for a side-to-side gastrojejunostomy, would decrease blood flow to the gastric remnant.
Resection of the gastric remnant and reconstruction with Roux-en-Y anastomosis was effective in relieving symptoms due to reflux esophagitis after PG (Ishii et al. 2006). Although resection of the gastric remnant has the advantage of preventing recurrence of cancer in the residual stomach, it is much more invasive. In contrast, duodenal switch procedure is easy, does not require takedown of the esophagogastrostomy and thus should have less morbidity.
In conclusion, the duodenal switch after PG may be surgical treatment of choice for intractable reflux gastroesophagitis, because this procedure, considered less invasive than resection of the remnant stomach with thoracotomy, relieves the patients’ symptoms.
The authors thank Dr. Michael G. Sarr, Department of Surgery, Mayo Clinic, MN for reviewing this manuscript.
All authors have no conflict of interest.