2013 Volume 231 Issue 4 Pages 257-263
2013 Volume 231 Issue 4 Pages 257-263
Elevated alanine aminotransferase (ALT) in serum, relevant to nonalcoholic fatty liver disease, has been often reported from Asian countries and the U.S., and it may be associated with lifestyle behavior. To clarify whether specific dietary behavior is associated with hepatocellular injury, we explored liver markers and dietary lifestyles (e.g., breakfast-skipping, eating for lunch, and snacking) in 1,809 male employees, aged 19-59 years, belonging to a health insurance union of automobile dealerships in Japan. ALT, γ-glutamyltransferase, and asparate aminotransferase (AST) were positively correlated with age and body mass index (BMI) (P < 0.0001). Odds ratios (ORs) of instant noodle ingestion for lunch to ALT elevation (> 30 IU/L), after adjusting for possible confounders including age, BMI, and drinking, were 1.33 (95% confidence interval, 1.01-1.75) at 1-2 times/week and 1.47 (1.07-2.01) at ≥ 3 times/week, compared to those who seldom ate instant noodles. Likewise, the OR of the ingestion at ≥ 3 times/week to γ-glutamyltransferase elevation (> 50 IU/L) was 1.42 (1.02-1.99), but the OR to elevated AST (> 30 IU/L) was not statistically significant. Habitual ethanol intake was significantly associated with hepatocellular injury, though the threshold of daily ethanol intake differed among liver markers. Despite the low OR, habitual instant noodle ingestion for lunch is associated with ALT elevation. Since the average content of saturated fatty acids in instant noodles is considerably high among cereal foods in Japan, workers with this habit should be advised to avoid having unbalanced diets.
The elevated activity of serum alanine aminotransferase (ALT) triggers the diagnosis of nonalcoholic fatty liver disease (NAFLD), and the NAFLD can affect the onset of type 2 diabetes mellitus, liver cirrhosis, and coronary heart disease (Clark et al. 2002; Korenblat et al. 2008; Targher et al. 2010; Cohen et al. 2011). In our experience of occupational health, busy workers with elevated ALT and γ-glutamyltransferase (GGT) often have been diagnosed with fatty liver, but not viral hepatitis, by physicians using abdominal ultrasonography, though they do not seem to have been exposed occupationally or environmentally to hepatotoxic chemicals such as carbon tetrachloride and perfluorinated chemicals. Apart from such diseases, ALT elevation has been reported from Asian countries and the U.S. (Clark et al. 2003; Lee et al. 2010; Zhang et al. 2011a). In China, elevated ALT frequently occurs in male peasants and small businessmen with increased income (Zhang et al. 2011b). Among American taxi drivers, long driving was associated with elevated ALT (Lippmann et al. 2011). For the prevention of liver injury in workers, it is crucial to clarify the causal factors.
The associations of ALT elevation with dietary behavior and exercise, along with age and body mass index (BMI), have been scrutinized (Solga et al. 2004; Oh et al. 2006; Lee et al. 2011; Park et al. 2011; Finelli and Tarantino 2012; Keating et al. 2012; Tarantino and Finelli 2013), but little is known about the specific cause of the elevation. In Japanese workers, although dinner menu items are changeable day by day, lunch menu patterns (e.g., box lunch, meals at restaurants, instant noodles like cup ramen, and rice-balls) seem to be generally unchanged; in this sense, it may be easy to explore lunch menu patterns of them. Accordingly, we formulated a hypothesis about dietary behavior that habitual ingestion of a certain lunch menu might lead to hepatocellular injury in Japanese workers and drew up a project designed to test it.
In February-March 2012, a self-reported questionnaire was distributed to approximately 2,200 male employees belonging to a health insurance union of motor vehicle dealerships in northeast Japan, including salesmen, mechanics, and office clerks, but excluding the managerial class. Of them, 1,857 men consented to our proposal and returned the forms to the occupational health nurse of the union (response rate, 84%). Forty-eight respondents were excluded: those who did not undergo the mandatory health checkup, conducted under the Industrial Safety and Health Law in Japan, in April-July 2012; those who suffered from stroke, ischemic heart disease, chronic renal failure, alcoholic dependency diagnosed by a psychiatrist, liver cirrhosis, or cancer; those whose serological tests for hepatitis B or C infection were positive; and finally, those whose reported questionnaire forms contained imperfect information. The study population consisted of 1,809 men aged 19-29 years (31.3%), 30-39 years (39.1%), 40-49 years (19.1%), and 50-59 years (10.5%). This study was conducted in accordance with the Declaration of Helsinki of 1964 as revised in 2000, after our study protocol was approved by the Ethical Review Committee of the Akita University Graduate School of Medicine.
Some mechanics of our subjects had underwent the specific health examination for organic solvent workers under the Industrial Safety and Health Law annually, and such workers had neither symptoms/signs of solvent poisoning nor abnormal findings in urinalysis. Nonetheless, the job category was scored as “mechanic” = 1 and “other worker” = 0.
Exposure and outcome variablesBreakfast, lunch, snack, and dinner, as well as smoking and drinking habits, regular exercise, job stress, and sleep duration, were inquired via the questionnaire on lifestyle behavior. Habits of breakfast-skipping, snacking during work hours, and dinner time irregularity were scored as “absence” = 0 and “presence” = 1. What each subject ate at lunch time on workdays, e.g., a home-made or takeout box lunch, meals at restaurants, instant noodles, rice-balls (onigiri, i.e., a ball of cooked rice usually formed by hand), etc., was also asked by a method of multiple responses. In addition, one more question about how often each ate instant noodles in a week was posed to the subjects who indicated that they did consume such noodles for lunch. Nocturnal sleep duration (min) was computed as the difference between bedtime and wake time on workdays. The weekly amount of each type of alcoholic beverage consumed was also asked as described previously (Dakeishi et al. 2004, 2006); e.g., “How many 180 ml-cups (or 1,800 ml-bottles) of sake do you drink in a week?” and “How many 350 ml-cans (500 ml-cans, or 633 ml-bottles) of beer do you drink in a week?” Types of alcoholic beverages listed were sake, beer, shochu (a Japanese distilled alcoholic beverage primarily made from barley or sweet potatoes), whisky, wine, and others (e.g., plum wine, brandy, gin, or vodka). A total of 100% ethanol equivalent dose (g/day) was calculated for each subject. Smoking habit was scored as “nonsmoker” = 0 and “smoker” = 1. Regular exercise was defined as at least one 30-min session at least once per week. The responses of exercise and job stress were scored as “absence” = 0 or “presence” = 1.
Data on liver markers, i.e., serum ALT, asparate aminotransferase (AST), and GGT, along with BMI (kg/m2), were obtained for each subject from the annual health checkup record. ALT, AST, and GGT were measured by the Akita Foundation for Healthcare (normal values were below 30 IU/L for ALT and AST, and below 50 IU/L for GGT), according to the principles recommended by the Japan Society of Clinical Chemistry (Kawai 1993). Based on a conventional value reported by Prati et al. (2002), an ALT level of 30 IU/L was adopted as an upper limit of normal value.
Concerning exposures to perfluorinated chemicals, medians and 95% confidence intervals (CIs) of serum perfluorooctanoic acid (PFOA) and perfluorooctane sulfate (PFOS) concentrations in 35 male employees, aged 21-63 years, of this union with ALT of median 34 (95% CI, 11.5-78) IU/L in 2010, measured by the Research Institute for Environmental Sciences and Public Health of Iwate Prefecture (Harada et al. 2004, 2007; Jin et al. 2007), were 2.32 (95% CI, 1.06-5.07) ng/ml and 7.03 (3.34-37.15) ng/ml, respectively, and there were no significant relationships between ALT and either PFOA or PFOS (P > 0.05). The PFOA and PFOS levels in the 35 men were about a half of those in 1,076 American men from 1999-2000 and 2003-2004 National Health and Nutrition Examination Survey (Lin et al. 2010), but were somewhat higher than those in 343 pregnant women in Hokkaido, Japan (Okada et al. 2012).
Statistical analysisSince ALT, AST, GGT, and daily ethanol intake did not show a normal distribution, they were logarithmically transformed in using simple regression analysis, and the median, minimum and maximum, but not mean ± standard deviation (s.d.), were employed in the tables. The significance of the differences in liver markers between mechanics and other workers was analyzed by the Mann-Whitney U test. Multiple logistic regression analysis was used to calculate odds ratio (OR) and 95% CI of lifestyle behavior (sleep duration, breakfast-skipping, snacking, irregularity of dinner time, smoking, daily ethanol intake, and regular exercise), lunch menu (box lunch, meals at restaurants, instant noodles, and rice-balls), and job category and stress, along with compulsory variables (age and BMI), to elevated ALT, AST or GGT. Concerning daily ethanol intake, since subgroups who consumed an empirical range of ethanol (i.e., 0, 0.1-30.0, 30.1-60.0, 60.1-90.0, and > 90.0 g/day) had been utilized in the preceding alcohol research (Bellentani et al. 1997; Dakeishi et al. 2006), we employed this categorization. All analyses, with two-sided P values, were performed using the SPBS Ver. 9.65 (Murata and Yano 2002), and the significance level was set at P < 0.05.
Baseline characteristics of 1,809 workmen are shown in Table 1. Proportions of abnormal liver markers among them were 28.2% for ALT (> 30 IU/L), 14.2% for AST (> 30 IU/L), and 24.0% for GGT (> 50 IU/L). As exemplified in Fig. 1, log-transformed ALT, AST, and GGT levels of the workmen were positively related to age and BMI (these Pearson product-moment correlation coefficients were between 0.122 and 0.520, P < 0.0001), indicating that age and BMI are inevitable confounders for assessment of liver markers in humans (Prati et al. 2002; Clark et al. 2003; Solga et al. 2004). Also, ALT, AST, and GGT levels of the 934 mechanics (median, 21, 21, and 25 IU/L, respectively) were lower than those of the 875 other workmen (23, 22, and 35 IU/L) (P < 0.0001, P = 0.0454, and P < 0.0001, respectively). Of the workmen, 525 ate instant noodles 1 to 2 times/week and 443 did three or more times/week.
The associations between each lifestyle behavior and elevated ALT, AST, and GGT after adjusting for the two compulsory confounders are shown in Table 2. Elevated ALT was associated positively with instant noodle ingestion and ethanol intake of more than 90 g/day and negatively with mechanics. AST elevation was associated positively with ethanol intake of more than 30 g/day, sleep duration, and regular exercise, and negatively with snacking. Likewise, elevated GGT was related positively to meals at restaurants, instant noodles, rice-balls, ethanol intake, sleep duration, and smoking, and negatively to mechanics and snacking.
Table 3 represents associations of lifestyle behavior with elevated ALT, AST, and GGT with adjustment for all parameters including age and BMI. All results, excluding the ORs of meals at restaurants and smoking to GGT elevation, were similar to those of Table 2. In addition, ORs of instant noodle ingestion at 1 to 2 times/week and at three or more times/week to elevated ALT were significantly high, as compared to the men who seldom ate instant noodles (Table 4). Likewise, the OR of instant noodle ingestion at three or more times/week to elevated GGT was 1.422 (95% CI, 1.018-1.985).
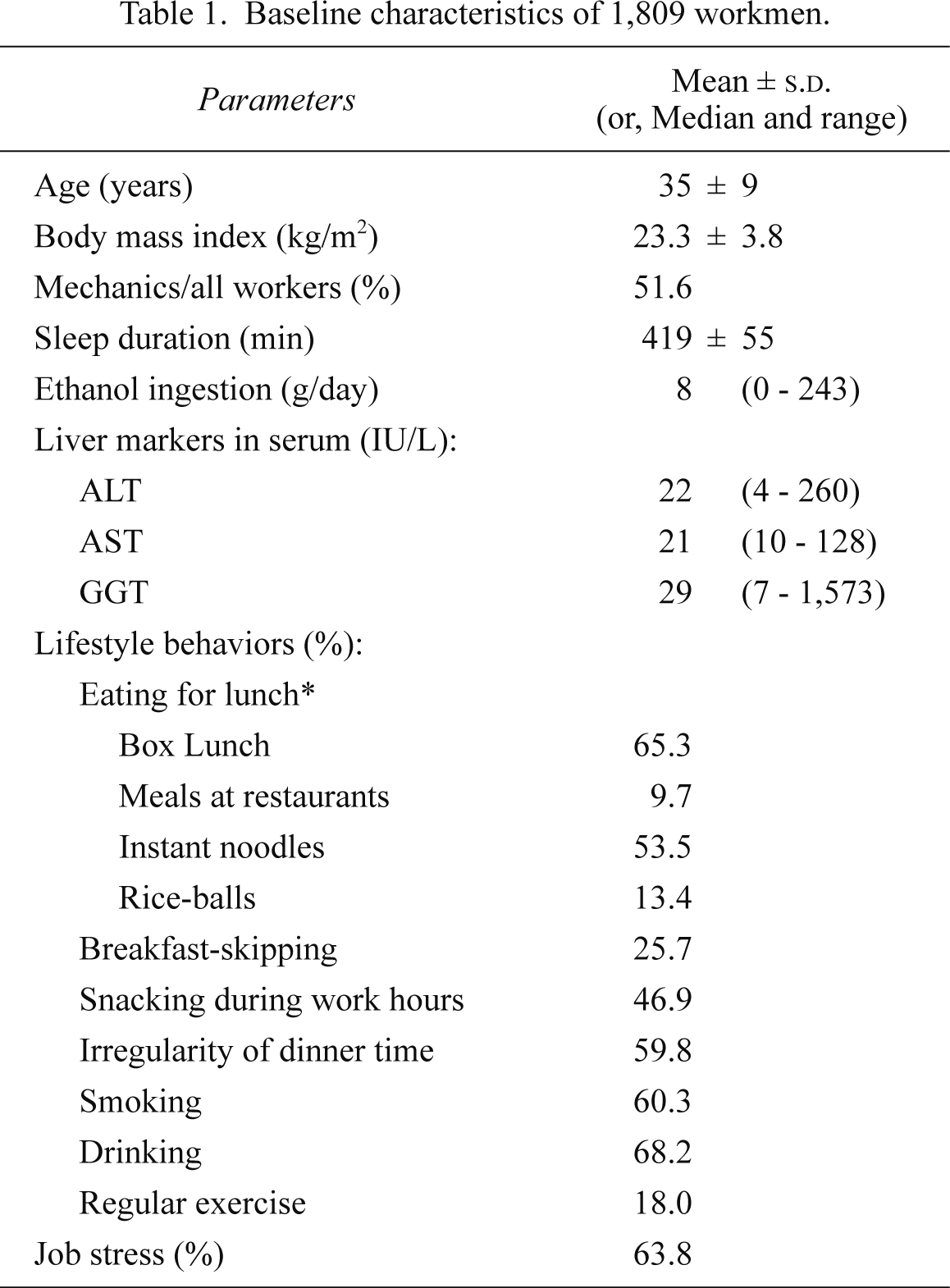
Baseline characteristics of 1,809 workmen.
ALT, alanine aminotransferases; AST, asparate aminotransferase; GGT, γ-glutamyltransferase; SD, standard deviation; range, (minimum - maximum).
*Multiple responses.

Effects of age and body mass index (BMI) on liver markers.
The liver markers were measured in 1,809 workmen: serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), and γ-glutamyltransferase (GGT). These markers were logarithmically transformed (i.e., log10[ALT], log10[AST], and log10[GGT]), and results of linear regression showed that the markers had significant relations to age and BMI (P < 0.0001).

Odds ratios of each lifestyle behavior to liver markers in 1,809 workmen with adjustment for age and body mass index.
See Table 1 regarding the above abbreviations.
*Multiple responses.

Odds ratios of lifestyle behavior to liver markers in 1,809 workmen with adjustment for all parameters including age and body mass index.
See Table 1 regarding the above abbreviations.
*Multiple responses.

Odds ratios of habitual instant noodle ingestion to liver markers in 1,809 workmen after adjusting for other parameters including age and body mass index.
See Table 1 regarding the above abbreviations.
The principal finding of our study was that habitual ingestion of instant noodles was associated with elevated ALT and GGT in Japanese workmen without obvious hepatotoxic exposures, and these risk ratios seemed to raise with the increased frequency of instant noodle ingestion. Such dietary habits had continued over long periods prior to their health checkups in 2012. These workmen did not always have enough time for lunch because they were usually busy with customers, who might walk into the showroom at any moment. As a result, food readily to eat was very convenient for them. Therefore, this may be the first report suggesting that one cause of elevated ALT is habitual ingestion of instant noodles.
Two explanations for the significant link between habitual instant noodle ingestion and ALT elevation are possible. Busy workers with heavy instant noodle ingestion habits, as well as young Korean men with higher income and education levels who preferred the noodle-bread dietary pattern showing greater intake of noodles and bread (Lee et al. 2011), may have had extremely unbalanced diets. Such habitual ingestion can lead to excessive intake of fats and energy (Park et al. 2011), because the average content of saturated fatty acids was 7.31-8.72 g per 100 g instant noodles and was the highest among cereal foods in Japan (Ministry of Education, Culture, Sports, Science and Technology 2005). In consequence, hepatic over-accumulation of saturated fatty acids, triggering hepatocellular apoptosis (Alkhouri et al. 2009), may result in ALT elevation; in fact, higher triglycerides were associated with elevated ALT in NAFLD patients and non-NAFLD subjects (Hou et al. 2011).
Another possibility is that some components of instant noodles might affect the liver. Instant noodles contain various kinds of food additives, e.g., acidity regulators, antioxidants, preservatives, colorant, and flavor enhancers (Codex Alimentarius Commission 2006), as well as other ingredients in the soup. In animal experiments, some food additives such as sodium nitrite, p-tert-butylcatechol, and sodium glutamate have hepatotoxicity (Asahina et al. 1971; Dunnick 2002; Collison et al. 2009). Additionally, food additives and ingredients of instant noodles can be converted into other chemicals, such as monochloropropanediol or acryl amide, after cooking or long-term preservation (Gotoh et al. 2006; Xu et al. 2013). Thus, habitual instant noodle ingestion may be said to constitute long-term exposure to food additives at lower levels; whereas, it would be difficult to confirm the effects of such chemicals on hepatocellular injury because of the uncertainties of accumulation in the liver of humans, but not animals.
Snacking habit attenuated the risk of elevated AST and GGT (Table 3), probably implying that it prevented workers from overeating dinner. By contrast, eating rice-balls and meals at restaurants was associated with elevated GGT, while these had no close relations to ALT or AST. Rice-ball ingestion may in part have corresponded to instant noodle ingestion, inasmuch as 192 (79.3%) of the workers eating rice-balls ate instant noodles (but none of them had a home-made box lunch). Actually, such noodle soup is often consumed as a substitute for miso soup, or even beverages for young Japanese workers. With regard to meals at restaurants, some workers may have consumed fast food because of their limited lunch time. Nonetheless, these two lunch items would be explained by the finding that higher carbohydrate intake was associated with higher odds of hepatic inflammation (Solga et al. 2004). Since certain dietary behavior, as well as physical activity patterns (Finelli and Tarantino 2012; Keating et al. 2012), can affect the liver both beneficially and adversely, clinical physicians and occupational health nurses should pay special attention to dietary lifestyles of patients with elevated ALT.
Overdrinking affected liver markers, as shown in Tables 3. The effect of daily ethanol intake is in accordance with a study using the benchmark dose levels (BMDLs, almost corresponding to the threshold when an effect starts to emerge) calculated from different data of the same health insurance union in 2002 (Dakeishi et al. 2004); i.e., the BMDLs of daily ethanol intake were 94 g/day for ALT, 52 g/day for AST, and 36 g/day for GGT. In this sense, ALT appears to be less sensitive to ethanol intake but also to be more specific to habitual ingestion of instant noodles than GGT and AST. Likewise, the influence of sleep duration on GGT was observed in the present and past studies (Hsieh et al. 2011). Taken together, daily ethanol intake and sleep duration, in addition to age and BMI in Fig. 1, are considered to be essential confounders in evaluating liver enzyme activities.
There may have been some limitations in the current study. Since abdominal ultrasonography was not conducted in the mandatory health checkups, we could not confirm whether our subjects had NAFLD. However, we focused on the impacts of dietary behavior on liver enzymes, but not such diseases, among the 1,809 male employees of the same occupational setting. Of course, none of them seemed to have been exposed to hepatotoxic substances including PFOA and PFOS occupationally or environmentally; that is, ALT, AST, and GGT levels of the car mechanics were lower than those of the other workmen. Although a self-reported questionnaire might introduce bias, alcohol data in this study showed a consistency with our past study (Dakeishi et al. 2004) as mentioned above, and lunch menu items, about which approximately 5% of the subjects were directly asked by the occupational health nurse 5 months after the mandatory health checkup in 2012, remained unchangeable. Finally, various lifestyle behaviors such as breakfast-skipping, snacking, irregularity of dinner time, sleep duration, and drinking and smoking habits, as well as age and BMI, were considered in the data analysis. Thus, it is suggested that our data were not heavily influenced by selection bias, measurement bias or confounders.
In conclusion, habitual ingestion of instant noodles may induce elevated ALT despite the low risk ratio. Busy workers with this habit should be advised to avoid having unbalanced diets, e.g., to reduce the frequency of instant noodle ingestion. On the other hand, since many instant noodles are consumed in China, Indonesia, Japan, Vietnam, Korea, India, and Thailand, as well as in the United States (World Instant Noodles Association 2013), detailed information on instant noodles and the food additives must be made public. Not doing this may lead to instant noodles containing unacceptable chemicals like benzopyrene (Food and Drug Administration, Philippines 2012), being sold at convenience stores.
This study was supported partly by a Grant-in-Aid for Scientific Research (C) from the Japan Society for the Promotion of Science. The authors thank Ms. Yumiko Kato at the health insurance union of motor vehicle dealerships, for her assistance in data collection.
The authors declare no conflict of interest.