Abstract
Air pollution in Japan caused respiratory disease, such as chronic bronchitis and asthma, in many individuals in the 1960s. Although air pollution has decreased, many victims of air pollution-related respiratory disease are limited in their activities of daily living because of respiratory symptoms. The purpose of this study was to evaluate the efficacy of pulmonary rehabilitation in victims of air pollution-related chronic bronchitis or asthma. Subjects were enrolled in a 12-week (2-week inpatient followed by 10-week outpatient) pulmonary rehabilitation program. The program comprised conditioning, strength training, endurance training, and patient education. We assessed the Modified Medical Research Council (MMRC) dyspnea grade, pulmonary function, peripheral muscle force, incremental shuttle walk distance (ISWD), and physical activity at baseline and immediately after the program. Twenty-nine subjects (mean age 74.2 ± 10.1 years, 11 males) completed the program, including 11 subjects with COPD and 18 subjects with asthma. Following rehabilitation, the participants (n = 29) showed significant improvements in MMRC dyspnea grade, vital capacity % predicted, quadriceps force and ISWD (all P < 0.05). Sub-group analyses revealed that all these variables were significantly improved in subjects with asthma. In contrast, subjects with COPD showed significant improvements only in quadriceps force and ISWD (both P < 0.05). Thus, pulmonary rehabilitation is an effective method of improving exercise capacity and dyspnea in officially acknowledged victims of air pollution-related asthma. In conclusion, we recommend that patients with chronic bronchitis or asthma, resulting from exposure to air pollution, are referred for pulmonary rehabilitation.
Introduction
In Japan, air pollution with industrially produced toxic substances worsened during the high economic growth in the 1950s, resulting in increased rates of respiratory diseases such as chronic bronchitis and asthma. Victims of air pollution-related respiratory disease have been officially acknowledged by the Japanese government to suffer damage to their health, and the prevention of such health damage is now ensured with the Basic Law for Environmental Pollution Control (1967) and the Pollution-Related Health Damage Compensation Law (1973). The percentage of victims of air pollution-related respiratory disease ≥ 60 years accounted for 43% at the end of March 2013. The study conducted by the Ministry of Environment of Japan in 2004 found that the activities of daily living (ADL) of officially acknowledged victims of air pollution-related respiratory disease are limited by respiratory symptoms that worsen with aging.
Pulmonary rehabilitation is well recognized as an effective intervention for patients with chronic obstructive pulmonary disease (COPD) (Ries et al. 2007; Spruit et al. 2013). The benefits of pulmonary rehabilitation include reduced dyspnea, increased exercise capacity, increased skeletal muscle function, improved performance of ADL, and health-related quality of life (HRQOL), decreased hospitalization for COPD exacerbations, and reduced anxiety and depression. Pulmonary rehabilitation has also been reported to be beneficial in patients with interstitial lung disease and asthma (Holland et al. 2008; Kozu et al. 2011; Turner et al. 2011; Spruit et al. 2013). Ochmann et al. (2012) reported that pulmonary rehabilitation improved muscle strength and exercise capacity in patients with occupation-related respiratory disease. However, the effects of pulmonary rehabilitation in officially acknowledged victims of air pollution-related respiratory disease are currently unclear. As the main symptom experienced by these patients is dyspnea, similar to that of COPD patients, pulmonary rehabilitation may be a useful treatment modality in this population.
The aim of this study was to evaluate the efficacy of pulmonary rehabilitation in officially acknowledged victims of air pollution-related respiratory disease.
Materials and Methods
Study Design and Subjects
This was a prospective single-group intervention study. The subjects were officially acknowledged victims of air pollution-related respiratory disease who gave informed consent for participation in the study. Registered victims all met the following criteria as determined by the Public Relief Systems of Kurashiki and Kitakyushu cities, in accordance with the Basic Law for Environmental Pollution Control (1967) and the Pollution-Related Health Damage Compensation Law (1973): (1) they resided or had spent time undertaking activities in an area specified as having significant air pollution (Table 1), and (2) they had been diagnosed with chronic bronchitis or asthma by a respiratory physician. Most subjects were diagnosed with respiratory disease more than 40 years ago. The exclusion criteria were: exacerbation of respiratory symptoms within the previous 4 weeks, inability to perform exercise testing or training, neuromuscular disease, and cognitive impairment rendering them unable to complete the questionnaires. This study was approved by the Human Ethics Review Committee of Nagasaki University Graduate School of Biomedical Science.

Gender, age, diagnosis, and use of long-term oxygen therapy (LTOT) were recorded for all subjects at baseline. Height, weight, dyspnea, pulmonary function, peripheral muscle force, exercise capacity, ADL, HRQOL, depression, and physical activity were assessed at baseline and immediately after a 12-week pulmonary rehabilitation program.
Body mass index was calculated from the height and weight. Dyspnea was evaluated using the Modified Medical Research Council (MMRC) dyspnea scale, which grades the severity of dyspnea during daily living from grade 0 to grade 4 (Mahler and Wells 1988).
Pulmonary function was evaluated using an electronic spirometer (FUDAC 70; Fukuda Sangyo Inc., Chiba, Japan). Forced expiratory volume in one second (FEV1), vital capacity (VC), and forced vital capacity (FVC) were measured in accordance with the recommended guidelines (American Thoracic Society 1995) and were repeated until at least three reproducible forced expiratory curves had been obtained. Results are expressed as percentages of predicted normal values, using data published by the Japanese Respiratory Society.
Handgrip force (HF) was measured twice in the dominant hand while standing, using a hand dynamometer (GRIP-D; OG Giken Corp., Okayama, Japan). The maximum force was recorded. Quadriceps force (QF) was measured as the peak force recorded during a maximal isometric knee extension maneuver with the hip and knee in 90° flexion using a hand-held dynamometer with a fixing belt (μ-Tas F-1; Anima Corp., Tokyo, Japan). The maximum value of three attempts on the dominant side was recorded. HF and QF were also calculated as percentages of the predicted values corrected for gender, age, height, and weight (The National Isometric Muscle Strength Database 1996).
Exercise capacity was assessed by the distance walked in the incremental shuttle walk test (ISWT), performed according to published standards (Singh et al. 1992). The test was performed twice and the maximum value was recorded.
ADL scores were evaluated using the Nagasaki University Respiratory Activities of Daily Living questionnaire (Takigawa et al. 2007). This questionnaire consists of 10 items, plus a score for walking distance. Each item rates movement speed, dyspnea, and flow rate of inspired oxygen from 0 to 3, and the continuous walking distance is scored from 0 to 10. The maximum total score is 100 points.
HRQOL was evaluated using the Japanese version of the St. George’s Respiratory Questionnaire (SGRQ) (Jones et al. 1992), which is a self-complete questionnaire. Depression was assessed using the Japanese version of the Center for Epidemiologic Studies Depression (CES-D) questionnaire (Radloff 1977). This questionnaire consists of 20 items with a maximum total score of 60 points, and a score of 16 points or greater was considered to indicate depression (Iwata et al. 1995).
Physical activity was evaluated using a uniaxial accelerometer (Lifecorder GS; Suzuken Corp., Nagoya, Japan). The accelerometer was worn around the waist from the time of rising in the morning until going to sleep at night (excluding bathing time). The energy expenditure and number of steps were recorded for 7 days at baseline and after pulmonary rehabilitation.
Pulmonary Rehabilitation Program
The pulmonary rehabilitation program included each patient’s usual medical care, oxygen therapy as required, dietary instruction, and patient education in parallel with exercise training. Physical function and health status were evaluated at baseline, and the program was tailored according to the needs of each patient. Exercise training consisted of: (1) conditioning (breathing training, relaxation, and stretches); (2) strength training (upper limb and lower limb); (3) endurance training (ground-based and treadmill walking, cycling); and (4) patient education (management of continued home exercise, performance of ADL, and self-management of exacerbations). For walking training, the initial intensity was prescribed at 60-80% of the maximum speed achieved in the ISWT. Subjects underwent inpatient rehabilitation (60 min of exercise training twice a day, 6 days per week, for 2 weeks) followed by outpatient rehabilitation (1-2 times per week for 10 weeks). They were instructed to follow a home program during outpatient rehabilitation that included conditioning, strength training, and ground-based walking.
Statistical Analysis
The Shapiro-Wilk test was used to examine the distribution of the data. Data that did not conform to a normal distribution were analyzed using nonparametric tests. Data were compared with respect to the baseline characteristics between subjects with chronic bronchitis and subjects with asthma, using unpaired t-tests, the Mann-Whitney U test and chi-square test. Pre- and post-pulmonary rehabilitation data were compared using paired t-tests, Wilcoxon signed-rank test and chi-square test. Statistical significance was defined at P < 0.05. All analyses were performed using IBM SPSS Statistics 18.0 for Windows (IBM SPSS, Tokyo, Japan).
Results
Fifty-three officially acknowledged victims of air pollution-related respiratory disease consented to participate in the study (Fig. 1). Twenty-nine of these subjects (55%) completed all 12 weeks of the pulmonary rehabilitation program, and were assessed immediately after the program. Of these 29 subjects, 11 had COPD and 18 had asthma. The characteristics of the 29 subjects are shown in Table 2. At baseline, 73% of subjects experienced significant dyspnea during daily life (i.e. MMRC grade 2, 3, or 4). Both HF and QF were impaired when compared to predicted normal values, and the rate of depression was high (66%). Comparison of baseline measures in subjects with COPD and those with asthma identified significantly higher ISWD and more preserved QF (% predicted values) in those with COPD (Table 2).
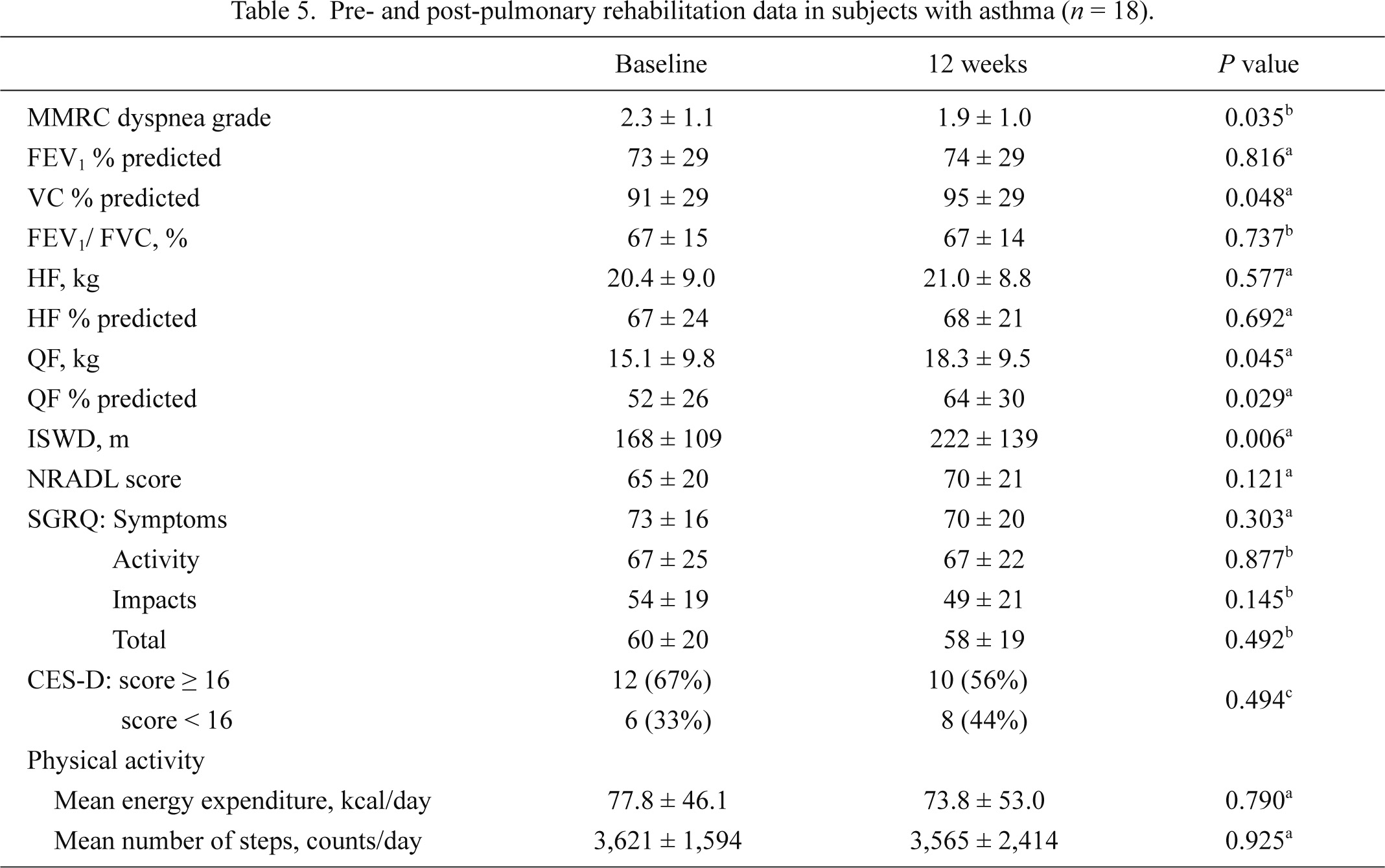
Pre- and post-pulmonary rehabilitation data are shown in Table 3 and Figs. 2 and 3. For the total subjects (n = 29), following pulmonary rehabilitation, there was a significant decrease in the MMRC dyspnea grade (P = 0.008) and a significant increase in percentage predicted VC (P < 0.05), QF (P < 0.05), and ISWD (P < 0.01). There were no significant changes in HF, ADL score, HRQOL score, or depression. Pre- and post-pulmonary rehabilitation data were also compared separately in subjects with chronic bronchitis (Table 4) and in those with asthma (Table 5). In subjects with asthma (n = 18), the measures that significantly improved following rehabilitation were MMRC grade, VC (% predicted), QF and ISWD (Table 5). In contrast, in those with COPD (n = 11), there was a trend towards an improvement in dyspnea (MMRC grade 1.9 ± 0.9 vs. 1.6 ± 0.6 [pre- vs. post-rehabilitation, P = 0.083]); however, only the improvements in QF (% predicted) and ISWD reached significance (Table 4).
The mean daily energy expenditure increased after the pulmonary rehabilitation program, but this change was not significant. The mean number of daily steps also did not change significantly.
Discussion
This study aimed to evaluate the effects of pulmonary rehabilitation in officially acknowledged victims of air pollution-related respiratory disease, including the effects on physical activity. The results show that subjects had increased exercise capacity and improved QF after pulmonary rehabilitation. In addition dyspnea decreased significantly in subjects with asthma, and there was a trend towards a reduction in dyspnea in those with chronic bronchitis.
One of the reasons for the decline in exercise capacity in COPD patients is skeletal muscle dysfunction. Inflammatory cytokines (Wouters et al. 2002), malnutrition, and oxidative stress (Rabinovich et al. 2001) may cause systemic inflammation in these patients, resulting in deconditioning (Kim et al. 2008). Exercise training improves deconditioning and increases exercise tolerance in COPD patients by improving skeletal muscle function. In our study population, exertional dyspnea and limitations to ADL were similar to those experienced by COPD patients. Skeletal muscle dysfunction was improved by exercise training, as shown by the increase in QF after the pulmonary rehabilitation program. In addition, ISWD increased by 45 m after pulmonary rehabilitation. In COPD patients, the minimal clinically important difference (MCID) in ISWD was reported to be 47.5 m (Singh et al. 2008). In this study, the improvement in distance walked was close to the MCID. This improvement may have resulted from improved skeletal muscle function.
HRQOL and depression were not significantly improved after pulmonary rehabilitation in this study. It has been shown that patients with COPD have reduced HRQOL accompanied by anxiety and depression due to limitations in daily life and to social isolation (Hayashi et al. 2011; Iguchi et al. 2013). Our patient population had low HRQOL and a high rate of depression. In a previous study of patients with occupation-related respiratory disease, mild or moderate decreases in pulmonary function and exercise tolerance were significantly associated with a poorer psychological status (Ochmann et al. 2012). It was also reported that patients with occupational asthma had a significantly poorer quality of life than other patients with asthma (Dimich-Ward et al. 2007). Chronic disease lasting for over 40 years may result in depression and low HRQOL. We therefore consider that it is important to provide medical care aimed at improving HRQOL and psychological status for officially acknowledged victims of air pollution-related respiratory disease. However, HRQOL and depression did not improve significantly after our pulmonary rehabilitation program, and other treatments may be required to address these issues.
Physical activity did not increase significantly after pulmonary rehabilitation. COPD patients have a low physical activity level compared with healthy subjects (Mador et al. 2011; Vorrink et al. 2011), and the physical activity level is a strong predictor of mortality (Waschki et al. 2011). Few studies have reported on changes in physical activity after pulmonary rehabilitation. Mador et al. (2011) studied 29 COPD patients who attended an 8-week pulmonary rehabilitation program, and found improved exercise capacity, muscle force, and HRQOL after the program, but no change in the physical activity level. Ng et al. (2012) suggested that it may be possible to improve the physical activity level in COPD patients by offering supervised exercise training at least 3 times a week for a minimum of 8 weeks. Another study suggested that improvement in the physical activity level in COPD patients requires changes in behaviors (modification of performance of ADL) and that these require long-term training of at least 3 months duration (Pitta et al. 2008). In this study, however, about 3 months of pulmonary rehabilitation did not result in an increase in physical activity. One reason for this may be that our program offered less frequent training than the programs used in previous studies (Ries et al. 2007; Spruit et al. 2013).
Our study has some limitations. First, the number of subjects was small and there was a high attrition rate (45%). One of the reasons for this is that many of the subjects were women, who were unable to participate in the inpatient pulmonary rehabilitation program for social reasons. Therefore, we consider that compliance with pulmonary rehabilitation programs may be poor in such individuals. Second, there was no control group for comparison. Future studies investigating pulmonary rehabilitation programs for officially acknowledged victims of air pollution-related respiratory disease should include a control group.
In this study, officially acknowledged victims of air pollution-related respiratory disease had increased exercise capacity and QF, and decreased dyspnea after participating in a pulmonary rehabilitation program. These results suggest that pulmonary rehabilitation, which is well established as an effective intervention in COPD patients, is also effective in patients with air pollution-related respiratory disease.
In conclusion, we examined the efficacy of pulmonary rehabilitation in 29 officially acknowledged victims of air pollution-related respiratory disease. The subjects participated in a 12-week pulmonary rehabilitation program that was originally developed for COPD patients, and demonstrated improved dyspnea, and increased exercise capacity and QF after the program. These results suggest that pulmonary rehabilitation is an effective intervention for officially acknowledged victims of air pollution-related respiratory disease.
Acknowledgements
This project was funded by the Environmental Restoration and Conservation Agency of Japan and supported by Mizushima-Kyodo Hospital, Misaki Hospital, Komenoyama Hospital, and Nishiyodo Hospital.
We thank all subjects, the technical staff, the administrative support team, and our coworkers for their help with this study. In addition, we are grateful to Sue Jenkins, PhD, Associate Professor at the School of Physiotherapy and Exercise Science, Curtin University for her help in reviewing this manuscript.
Conflict of Interest
The authors declare no conflict of interest.
References
-
American Thoracic Society
(1995) Standardization of Spirometry, 1994 Update. Am. J. Respir. Crit. Care Med., 152, 1107-1136.
-
Dimich-Ward,
H.,
Taliadouros,
V.,
Teschke,
K.,
Chow,
Y.,
Abboud,
R. &
Chan-Yeung,
M.
(2007) Quality of life and employment status of workers with Western red cedar asthma. J. Occup. Environ. Med., 49, 1040-1045.
-
Hayashi,
Y.,
Senjyu,
H.,
Iguchi,
A.,
Iwai,
S.,
Kanada,
R.,
Honda,
S. &
Ozawa,
H.
(2011) Prevalence of depressive symptoms in Japanese male patients with chronic obstructive pulmonary disease. Psychiatry Clin. Neurosci, 65, 82-88.
-
Holland,
A.E.,
Hill,
C.J.,
Conron,
M.,
Munro,
P. &
McDonald,
C.F.
(2008) Short term improvement in exercise capacity and symptoms following exercise training in interstitial lung disease. Thorax, 63, 549-554.
-
Iguchi,
A.,
Senjyu,
H.,
Hayashi,
Y.,
Kanada,
R.,
Iwai,
S.,
Honda,
S.,
Kitagawa,
C.,
Ozawa,
H. &
Rikitomi,
N.
(2013) Relationship between depression in patients with COPD and the percent of predicted FEV1, BODE index, and health-related quality of life. Respir. Care, 58, 334-339.
-
Iwata,
N.,
Roberts,
C.R. &
Kawakami,
N.
(1995) Japan-U.S. comparison of responses to depression scale items among adult workers. Psychiatry Res., 58, 237-245.
-
Jones,
P.W.,
Quirk,
F.H.,
Baveystock,
C.M. &
Littlejohns,
P.
(1992) A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am. Rev. Respir. Dis., 145, 1321-1327.
-
Kim,
H.C.,
Mofarrahi,
M. &
Hussain,
S.N.
(2008) Skeletal muscle dysfunction in patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis., 3, 637-658.
-
Kozu,
R.,
Senjyu,
H.,
Jenkins,
S.C.,
Mukae,
H.,
Sakamoto,
N. &
Kohno,
S.
(2011) Differences in response to pulmonary rehabilitation in idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease. Respiration, 81, 196-205.
-
Mador,
M.J.,
Patel,
A.N. &
Nadler,
J.
(2011) Effects of pulmonary rehabilitation on activity levels in patients with chronic obstructive pulmonary disease. J. Cardiopulm. Rehabil. Prev., 31, 52-59.
-
Mahler,
D.A. &
Wells,
C.K.
(1988) Evaluation of clinical methods for rating dyspnea. Chest, 93, 580-586.
-
Ng,
C.L.W.,
Mackney,
J.,
Jenkins,
S. &
Hill,
K.
(2012) Does exercise training change physical activity in people with COPD? A systematic review and meta-analysis. Chron. Respir. Dis., 9, 17-26.
-
Ochmann,
U.,
Kotschy-Lang,
N.,
Raab,
W.,
Kellberger,
J.,
Nowak,
D. &
Jorres,
R.A.
(2012) Long-term efficacy of pulmonary rehabilitation in patients with occupational respiratory diseases. Respiration, 84, 396-405.
-
Pitta,
F.,
Troosters,
T.,
Probst,
V.S.,
Langer,
D.,
Decramer,
M. &
Gosselink,
R.
(2008) Are patients with COPD more active after pulmonary rehabilitation? Chest, 134, 273-280.
-
Rabinovich,
R.A.,
Ardite,
E.,
Troosters,
T.,
Carbo,
N.,
Alonso,
J.,
Gonzalez de Suso,
J.M.,
Vilaro,
J.,
Barbera,
J.A.,
Polo,
M.F.,
Argiles,
J.M.,
Fernandez-Checa,
J.C. &
Roca,
J.
(2001) Reduced muscle redox capacity after endurance training in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med., 164, 1114-1118.
-
Radloff,
L.S.
(1977) The CES-D Scale: a self-report depression scale for research in the general population. Appl. Phychol. Meas., 1, 775-777.
-
Ries,
A.L.,
Bauldoff,
G.S.,
Carlin,
B.W.,
Casaburi,
R.,
Emery,
C.F.,
Mahler,
D.A.,
Make,
B.,
Rochester,
C.L.,
Zuwallack,
R. &
Herrerias,
C.
(2007) Pulmonary rehabilitation: Joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest, 131, 4S-42S.
-
Singh,
S.J.,
Jones,
P.W.,
Evans,
R. &
Morgan,
M.D.
(2008) Minimum clinically important improvement for the incremental shuttle walking test. Thorax, 63, 775-777.
-
Singh,
S.J.,
Morgan,
M.D.,
Scott,
S.,
Walters,
D. &
Hardman,
A.E.
(1992) Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax, 47, 1019-1024.
-
Spruit,
M.A.,
Singh,
S.J.,
Garvey,
C.,
ZuWallack,
R.,
Nici,
L.,
Rochester,
C.,
Hill,
K.,
Holland,
A.E.,
Lareau,
S.C.,
Man,
W.D.,
Pitta,
F.,
Sewell,
L.,
Raskin,
J.,
Bourbeau,
J.,
Crouch,
R. et al.
(2013) An official american thoracic society/european respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med., 188, e13-64.
-
Takigawa,
N.,
Tada,
A.,
Soda,
R.,
Takahashi,
S.,
Kawata,
N.,
Shibayama,
T.,
Matsumoto,
H.,
Hamada,
N.,
Hirano,
A.,
Kimura,
G.,
Okada,
C.,
Endo,
S.,
Yamashita,
M.,
Date,
H. &
Takahashi,
K.
(2007) Comprehensive pulmonary rehabilitation according to severity of COPD. Respir. Med., 101, 326-332.
-
The National Isometric Muscle Strength (NIMS) Database Consortium
(1996) Muscular weakness assessment: use of normal isometric strength data. Arch. Phys. Med. Rehabil., 77, 1251-1255.
-
Turner,
S.,
Eastwood,
P.,
Cook,
A. &
Jenkins,
S.
(2011) Improvements in symptoms and quality of life following exercise training in older adults with moderate/severe persistent asthma. Respiration, 81, 302-310.
-
Vorrink,
S.N.,
Kort,
H.S.,
Troosters,
T. &
Lammers,
J.W.
(2011) Level of daily physical activity in individuals with COPD compared with healthy controls. Respir. Res., 12, 33.
-
Waschki,
B.,
Kirsten,
A.,
Holz,
O.,
Muller,
K.C.,
Meyer,
T.,
Watz,
H. &
Magnussen,
H.
(2011) Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest, 140, 331-342.
-
Wouters,
E.F.,
Creutzberg,
E.C. &
Schols,
A.M.
(2002) Systemic effects in COPD. Chest, 121, 127S-130S.