2014 年 232 巻 3 号 p. 195-199
2014 年 232 巻 3 号 p. 195-199
Trunk instability is one of main problems in survivors following stroke. We investigated the effects of weight-shift training (WST) on an unstable surface in sitting position on trunk control, proprioception, and balance in individuals with chronic hemiparetic stroke. Eighteen participants with chronic hemiparetic stroke were recruited and were allocated to either WST or control group. The WST group received a weight-shift training program for 30 min and then received a conventional exercise program for 30 min, while the control group received conventional exercise program for 60 min, five times a week for four weeks for both groups. In this randomized control study, we used three outcome measures: trunk reposition error (TRE), Trunk Impairment Scale (TIS), and Timed Up and Go (TUG) test. TRE was measured by each participant’s reposition error to the target angle during his/her active trunk movement. TIS and TUG were examined for trunk control abilities and dynamic balance abilities, respectively. After training, TRE showed significantly greater improvement in the WST group (mean change, 1.67 ± 1.45˚) than the control group (mean change, 0.08 ± 1.05˚). The TIS score was significantly higher in the WST group (mean change, 2.33 ± 1.50) than the control group (mean change, 0.13 ± 0.83). The TUG test also showed a significant improvement in the WST group (mean change, 5.03 ± 1.88 sec) than the control group (mean change, 2.59 ± 1.86 sec). Our findings indicate that weight-shift training is beneficial for improving trunk control and proprioception in patients with chronic hemiparetic stroke.
Trunk control needs to be preceded in order to control distal limb movements and is correlated with functional movements (Davies 1990; Verheyden et al. 2006). Trunk control is the ability to maintain the upright posture of the body, to adjust weight shifting, and to perform selective movements in the trunk to maintain the center of mass within the base of support (Verheyden et al. 2004). All of these functions require proper sensorimotor ability of the trunk (Ryerson et al. 2008).
Stroke is one of the major causes that induce impaired trunk control, including weight shifting and equilibrium reaction (Goldie et al. 1996; Laufer et al. 2000; Dault et al. 2003). Stroke patients have decreased trunk control ability in all planes, more so in the frontal plane (Rode et al. 1997; de Haart et al. 2004). Studies reported that stroke patients have decreased trunk muscle strength compared to healthy controls (Tanaka et al. 1997, 1998), and that chronic stroke patients have a greater reposition error than healthy participants when their trunk proprioception was measured (Ryerson et al. 2008). For these reasons stroke patients have decreased weight-shift ability (Mudie et al. 2002) and trunk control (Verheyden et al. 2005) and therefore weight-shifting and balance are considered fundamental for functional activities (Howe et al. 2005).
According to several studies, trunk control ability can be improved by performing specific exercise training (Howe et al. 2005; Verheyden et al. 2007; Saeys et al. 2012). A study by Verheyden et al. (2009) showed that 10 hours of additional trunk exercises improved the ability to control the trunk in subacute stroke patients, and reaching exercises performed while seated were reported to improve sitting balance, peak vertical force on the paretic foot, and gait speed in chronic hemiplegic patients (Dean et al. 2007). Ryerson et al. (2008) stated that proprioceptive training is essential to improve trunk control and balance, and Eils and Rosenbaum (2001) suggested that exercising on an unstable surface is effective in improving body position awareness. One study reported that trunk exercises on a physio ball are effective in improving trunk control and functional balance in acute stroke patients (Karthikbabu et al. 2011a).
However, there are no existing studies on the effect of trunk control training on proprioception for stroke patients. In addition, the carry-over effect of trunk control training on mobility is insufficient. Also, most studies on trunk control training in stroke patients are based on acute stroke patients, and studies on chronic stroke lack in quantity (Karthikbabu et al. 2011b). Therefore, this study is designed to investigate the effects of weight-shift training on an unstable surface in sitting position on trunk control, proprioception, and dynamic balance during gait in patients with chronic stroke.
Eighteen patients with chronic hemiparetic stroke were recruited for this study and were assigned to either the weight-shift training (WST) (nine patients) or the control (nine patients) groups from K Rehabilitation Center. In order to rule out the possibility of natural recovery, the inclusion criteria for subjects were as follows: those who were diagnosed with first onset of unilateral hemisphere stroke more than six months ago, those who had no neglect of paretic limbs, could sit independently for 30 seconds on a stable surface, were medically stable, had no peripheral neuritis, had no musculoskeletal problems such as low back pain or arthritis affecting motor performance, and were able to understand and follow simple verbal instructions (Karthikbabu et al. 2011a). Due to a change of address, one participant in the control group withdrew from the study before the posttest. Table 1 shows a list of the general characteristics of subjects in the WST and control groups. After being informed about the study, all subjects agreed to participate and signed a consent form. The study was approved by the Institutional Review Board of Sahmyook University.
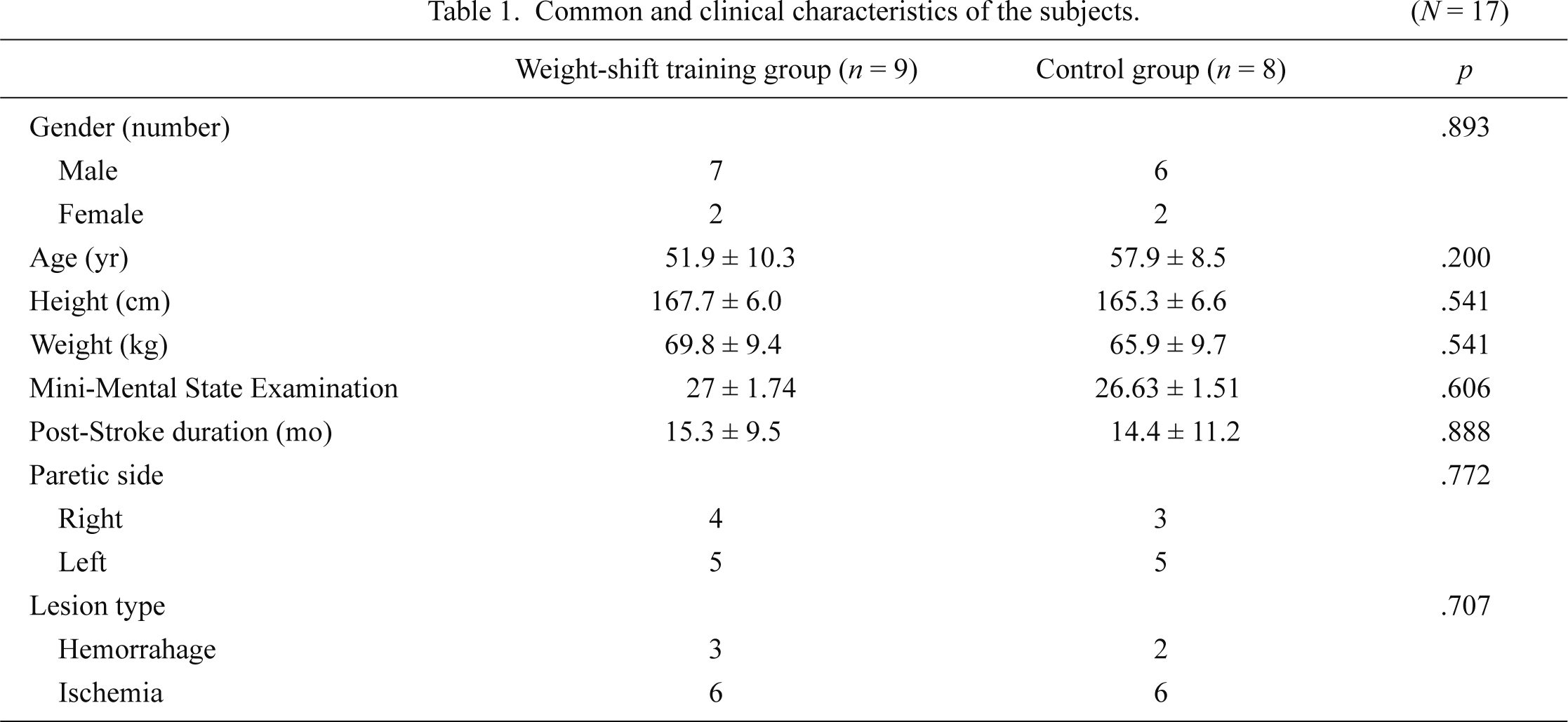
Common and clinical characteristics of the subjects.
Values are expressed as mean ± Standard deviation.
This study was observer-blinded and a pilot randomized controlled trial (RCT) design. The patients included in the study were randomly assigned to the WST or control group by randomly selecting from a sealed envelope for allocation. Subjects in the WST group participated in weight-shift training on an unstable surface using a Balance Pad (Airex®, Aalen, Germany) and Dynamic Ball Cushion (Dynair® ball cushion Deko, TOGU, Germany) for 30 min, five times a week for four weeks while those in the control group participated in a conventional exercise program for the same amount of time. All subjects in this study received a conventional exercise program provided by the rehabilitation hospital for 30 min, five times a week for four weeks. The conventional exercise program was patient-specific and consisted physiotherapy including stretching, strengthening, and stationary bicycle. Therapists combined elements from different neurological treatment concepts, but the main emphasis was on the neurodevelopmental treatment concept and on motor relearning. Data collection included trunk reposition error (TRE), Trunk Impairment Scale (TIS), and the Timed Up and Go (TUG) test before and after the four-week exercise period. Tests were conducted in a quiet and well-organized therapy room and participants were given the standard verbal instructions for the testing procedures.
InterventionSubjects had five minutes of warm up and cool down before and after each section. In this study, WST group was performed in two sitting postures, which was a modified version of the intervention studied and suggested by Verheyden et al. (2009). Two sitting postures were performed on an exercise mat; one with the knees extended and one with the knees flexed on the edge of the testing table. To identify the training protocol for weight shifting, each subject’s range of weight shifting was measured by a piece of graph paper placed behind the participant’s back. Subjects were instructed to sit with their arms folded and to shift their weights from midline to the right and left, as far as they could. When the maximum range of weight shifting was defined on each side of the movement on a stable surface, a bar was placed 2 cm closer to the patient as a target marker for WST program.
The WST group was performed in four conditions. For the first condition weight shift, subjects were instructed to sit on an exercise mat with legs extended, and have a balance pad under their buttocks. The second weight-shift condition was to sit with legs extended, have a balance pad under the buttocks, and a balance cushion under both heels. For the third weight shift condition, subjects were to sit on the edge of a testing table with a balance pad under the buttocks. The fourth weight shift condition was to sit on the edge of a testing table, have a balance pad under the buttocks, and a balance cushion under the feet. Conditions 1 and 2 had a higher level of difficulty, because the subject was to sit with the knees extended, which makes the buttocks the center of gravity. These two conditions often made the subject form a round back, and thus tactile and verbal cues to “straighten your back” were continuously given while the therapist verified to see that the back was straightened. The acromion was the landmark for the weight-shift movement, where a marker was attached on the right and left side. Subjects were instructed to shift their weight and touch the bar placed on both sides by elongating the trunk on the weight shifting side. Subjects were to hold the position for 10 seconds when they reached the target point by shifting weight, and then return to the starting position; this was counted as one trial. Each subject performed three sets of 10 trials, rest for 30-second break between each set, and a 1-minute break between each type of training.
Outcome measureTwo physical therapists with clinical experience in stroke rehabilitation therapy provided the training to the subjects, and two other physical therapists who were not involved in the study evaluated the subjects. Trunk reposition error, TIS, and TUG test were used for the evaluation of trunk control and function. Trunk reposition error was measured for the evaluation of trunk proprioception, and TIS, which evaluates the quality of the upper and lower trunk mobility, was used for trunk control evaluation. TUG test was used to evaluate dynamic balance during gait.
Repositioning error of the trunk was assessed with Dualer IQ™ digital inclinometer (J-TECH medical, Salt Lake City, UT, USA). Subjects were to stay in an upright sitting position on a chair, have their feet resting on the floor with 90° of hip and knee flexion with their back unsupported. They were then positioned into a target angle of trunk side flexion for 5 seconds, and instructed to remember the position. Subjects were asked to actively move to the target position according to their memory. Reposition error, which is the degree of deviation from the target position, was measured five times, and the average value was used for analysis (O’Sullivan et al. 2003).
The TIS, which observes the quality of trunk movement, serves as a guide for trunk treatment in stroke patients. The test consists of three subscales: static sitting balance, dynamic sitting balance, and coordination. Each subscale consists of 3 to 10 items. The TIS score ranges from a minimum of 0 to a maximum of 23, with higher scores indicating better trunk performance. The TIS is an excellent and reliable tool for measurement with the ICC for test-retest reliability of r = 0.96, and inter-rater reliability of r = 0.99 (Verheyden et al. 2004; Verheyden and Kersten 2010).
The TUG test examines the postural control that is associated with rising from a chair, turning, and sitting down (Podsiadlo and Richardson 1991). Neurologically intact adults who are independent in balance and mobility skills are able to perform the test in less than 10 seconds. Adults with neurologic pathology who took longer than 30 seconds to complete the test were dependent in most activities of daily living and mobility skills (Faria et al. 2013). The intra-rater (r = 0.99) and inter-rater (r = 0.98) reliabilities demonstrated high reliability (Ng and Hui-Chan 2005).
Data analysisSPSS for Windows version 12.0 (SPSS Inc., Chicago, IL, USA) was used in performance of data analysis. All participants were calculated by G*power 3.1.7 program for power analysis. The Mann Whitney U-test was used for analysis of differences in general characteristics, including age, height, weight, post-disease duration, and scores for dependent variables in the pre-test. Wilcoxon signed-ranks test was used for evaluation of differences within paired scores based on pre-test and post-test in each group. Mann Whitney U-test was used to determine whether a change in score from the pre-test to the post-test of the dependent variables differed significantly between the two groups. The significance level was set to P < 0.05.
The total sample size was eighteen, which was calculated to maintain alpha error probability (0.05), power (0.95), and effect size (1.65) in difference between two independent means. No significant difference was found in general characteristics and pre-test scores between the WST and control groups before treatment (Table 1). After training, the trunk reposition error in the WST group was significantly greater than the control group. The angle difference before and after training was 1.67 ± 1.45° in the WST group and 0.08 ± 1.05° in the control group. The TIS score in the WST group (mean score change, 2.33 ± 1.50) was significantly higher than the control group (mean score change, 0.13 ± 0.83). TUG test scores in the WST group (mean time change, 5.03 ± 1.88) showed a significant decrease compared to the control group (mean time change, 2.59 ± 1.86) (Table 2).
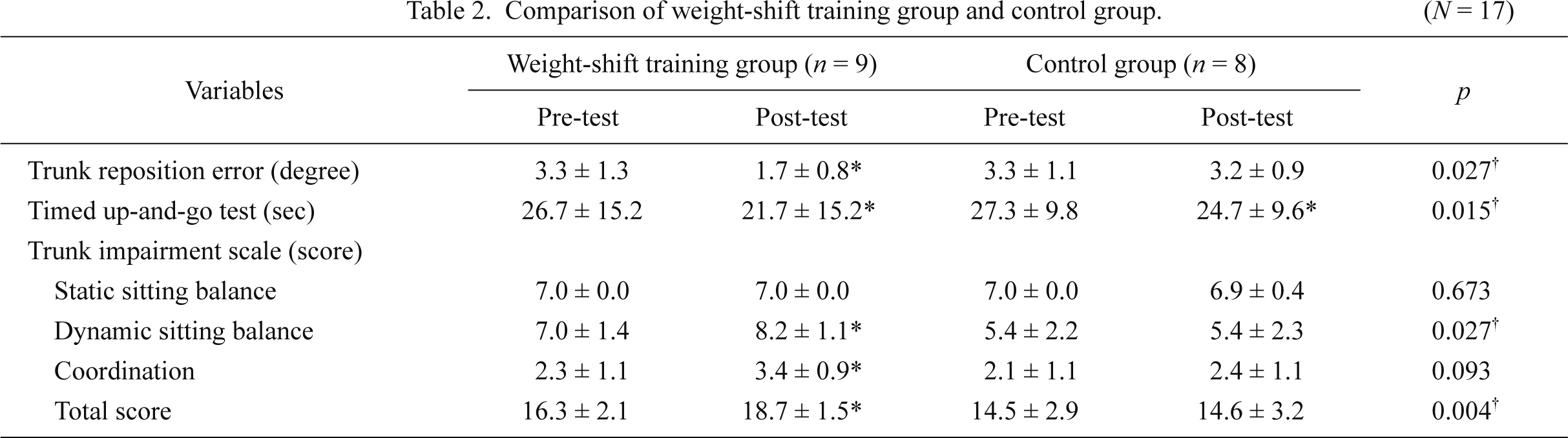
Comparison of weight-shift training group and control group.
Values are expressed as mean ± Standard deviation.
*Significant differences compared to pre-test and post-test in weight-shift training group.
†Significant differences compared to changeable values (from pre-test to post-test) between weight-shift training and control groups.
This study attempted to determine whether weight-shift training on an unstable surface could result in an improved trunk control and proprioception in chronic stroke patients. The study results on the reposition error of the trunk showed a greater improvement in the WST group than in the control group. Trunk control training on an unstable surface was reported to be very effective in increasing proprioceptive inputs to the neuromuscular system (Gruber and Gollhofer 2004). Eils and Rosenbaum (2001) reported that exercising with balance balls improved proprioception, and Kawato et al. (1987) stated that training on an unstable surface improved postural control as subjects corrected errors through feedback. In this study, the improvement in trunk proprioception was considered to be affected by the training that required subjects to maintain balance after shifting weights to the target point. Moreover, a continuous feedback was provided to the subjects so that the markers on the acromion did not recede from the target point. This task-oriented proprioception training may have caused the improvement.
Ryerson et al. (2008) reported a significantly higher reposition error of the trunk in stroke patients when compared to healthy subjects, and that poor proprioception was related to trunk control. Mudie et al. (2002) stated that improved trunk proprioception in stroke patients affect trunk control. In this study, improved results were found in dynamic sitting balance and coordination sections of TIS. The improvement in trunk control shown in this study may be caused by improved trunk proprioception. Karthikbabu et al. (2011a) reported improved trunk control and dynamic balance after training stroke patients on an unstable surface for trunk control. Stabilizing the trunk in response to external perturbations is known as reactive postural control (van Nes et al. 2008), and training on an unstable surface constantly induces reactive postural control in the trunk muscles for balance, making muscle activity and trunk control improvement more effective compared to training on a stable surface (Karthikbabu et al. 2011a). In this study, most of the patients initially experienced difficulty performing the weight-shifting task on an unstable surface, but the distance of weight shifting slowly increased as they adapted to the task. There were no score changes found in static sitting balance subscale, because the subjects in this study were able to maintain independent sitting posture for more than 10 seconds.
Saeys et al. (2012) reported that improved trunk control has a carry over effect on dynamic balance after trunk control training, and that the trunk stability is essential for limb movements. The results of TUG also showed a significant improvement in the WST group compared to the control group in this study. This may indicate that improved trunk control affects dynamic balance in patients with stroke. According to a study on trunk movement during gait in stroke patients, the patients had unstable and asymmetric trunk movements (Tyson 1999), and an improvement in trunk control affected walking speed and symmetry (Karthikbabu et al. 2011b). The significantly improved TUG scores after training in this study may have been affected by improved trunk control that influenced balance during gait.
The results of this study indicated a significant efficacy of weight shifting on an unstable surface in improving trunk proprioception and trunk control in patients with chronic stroke. However, the number of participating subjects was not large enough to generalize the results, and the differences in weight shifting ability between the WST group and the control group were not compared after training. In order to increase our understanding in this area of study, further studies of the effectiveness of weight-shift training on an unstable surface need to be conducted with a larger number of subjects and greater variation with regard to the types of unstable surfaces as therapeutic protocols. The distance of weight shifting and weight distribution also need to be studied to determine whether weight-shifting ability can be improved by training. Future studies could include the use of biofeedback training to objectively train subjects to maintain appropriate posture.
This study was supported by Sahmyook University (2012).
The authors declare no conflict of interest.