2014 Volume 234 Issue 3 Pages 169-174
2014 Volume 234 Issue 3 Pages 169-174
Dietary changes resulting from the post-World War II occupation of Okinawa by the US military have been largely deleterious, resulting in a marked increase of obesity among Okinawan residents. In this study, we examined the association between BMI and the risk of developing breast cancer according to the menstruation status and age, and the correlation between BMI and expression of estrogen receptor (ER). Breast cancer cases were 3,431 females without any personal or family history of breast cancer. Control subjects were 5,575 women drawn from the clinical files of Nahanishi Clinic. We found that women, who were overweight or obese, regardless of menopausal stage, had a higher risk of breast cancer compared to women with normal weight and this difference was statistically significant (p < 0.001, respectively). This risk was especially apparent in older (> 40 years) overweight or obese women. The women who were overweight or obese during postmenopausal ages were at higher risk of ER-positive breast cancer compared to women with normal weight. Results of our present study clearly indicate that increased BMI was associated with increased risk of developing breast cancer in Okinawan women, regardless of menopausal status. In addition, there was statistically significant correlation between BMI and ER expression in the postmenopausal period. Given the obesity epidemic associated with the extreme sociological and dietary changes brought about by the post-war occupation of Okinawa, the present study provides essential guidelines on the management, treatment and future breast cancer risk in Okinawa.
Breast cancer is the most common cancer in women worldwide (Tamaki et al. 2011, 2012; Youl et al. 2011). In Japan, the most predominant cancer in women at this juncture is that of the breast with incident rates increasing (Matsuda et al. 2012). This continuous increase of breast cancer incidence in Japan has resulted in widespread public health concern, with much attention being devoted to the importance of body mass index (BMI) and more specifically obesity as one of the most important risk factors (Harris et al. 2011a).
Obesity is a growing health problem globally (Berg et al. 2005) and its prevalence among the younger generations has increased continuously in Japan (Matsushita et al. 2008). Of note, this trend has been especially marked among individuals living in Okinawa compared to individuals living in mainland Japan (Matsushita et al. 2008). In Okinawa, the longevity advantage has been well documented (Matsushita et al. 2008) in older generations. This advantage is attributed to lifestyle, in particular, diet rather than ethnicity. The traditional diet of Okinawa consists of foods low in calories but rich in nutritional value, particularly in terms of vitamins, minerals, and phytonutrients in the form of antioxidants and flavonoids (Suzuki et al. 2001; Willcox et al. 2007) and importantly delicious in flavor. However, the post-World-War-II US military occupation of Okinawa had largely deleterious health effects, with Okinawan people developing higher rates of obesity corresponding to these post-war years (Todoriki et al. 2004; Willcox 2005; Tamaki et al. 2013) and a loss of the previous longevity advantage associated with the Okinawan lifestyle (Todoriki et al. 2004; Willcox 2005; Tamaki et al. 2013). The main change in this period, and simplest and most plausible explanation for this change was the introduction of an US lifestyle and diet to the Okinawan people. The US diet of the 1950s characterized by historically unprecedented amounts of readily available junk foods characteristically high in sugars and fats with minimal nutrition, combined with a low physical activity of US lifestyle might have contributed to the current high prevalence of overweight and/or obese individuals in Okinawa (Matsushita et al. 2008).
Importantly BMI is known to have a multifaceted mechanistic connection with breast cancer risk, although limited evidence suggests the risks associated with an increased BMI may be dependent upon menopausal status (Harris et al. 2011b). The majority of studies report an increased risk of higher BMI in both pre and post-menopausal breast cancers (Cauley et al. 1989; Sonnenschein et al. 1999; Key et al. 2003; Barlow et al. 2006; Tian et al. 2007), while one study suggests an inverse association between BMI in early adulthood and breast cancer incidence (Harris et al. 2011b). Despite the studies above, to the best of our knowledge, no studies have reported on the correlation between BMI and breast cancer risk for Okinawan people and in particular increased risks associated with the marked increases in BMI since US military occupation. Therefore, we examined the correlation between BMI and breast cancer of both premenopausal and postmenopausal women. To try and develop some mechanistic insight, we examined interactions between BMI and expression of estrogen receptor (ER), as these have been previously suggested to be associated in breast cancer patients (Feigelson et al. 2006; Millikan et al. 2008; Kwan et al. 2009; Suzuki et al. 2011; Sueta et al. 2012).
This study was conducted based upon Nahanishi Clinic Data Base System, Nahanishi Clinic, Okinawa, Japan. Table 1 summarizes the relevant information of the patients enrolled in our present study. This was a single institution study drawn from patients who visited the Nahanishi Clinic between May 1996 and March 2013. Case subjects were 3,431 female breast cancer patients without any personal or family breast cancer history. Control subjects were 5,575 women who visited the clinic but did not have detectable breast cancer; namely, the control subjects were defined as those who visited the clinic for breast cancer screening or non-malignant breast cancer growths. The median ages were 53 years old (20-99) of breast cancer group and 44 years old (20-90) of control group. The study protocol was approved by the Ethics Committee at Nahanishi Clinic Okinawa, Naha, Japan (NNCEC2013005). Results of their weights and heights were self-reported. As a relative indicator of body weight, BMI was calculated as weight in kilograms divided by the square of the height in meters (kg/m2). Based on the criteria of World Health Organization classification, 18.5 < BMI was defined as underweight, 25 ≤ BMI < 30 as overweight and 30 ≤ BMI as obese. The presence of ER was determined by distinctive nuclear immunoreactivity and the scores were graded from 0 to 8 using the Allred score, with positive case defined as the score of more than 3 (Allred et al. 1998). We had incomplete information regarding menstruation status (8,163 out of 9,006 subjects) and ER status (3,049 out of 3,431 breast cancer patients) leaving us with variable numbers when examining these factors in relation to breast cancer risk. We also examined the correlation between BMI and ER expression during premenopausal and postmenopausal status in 3,049 patients. Statistical analyses were performed using StatMate IV for Windows (ATMS, Tokyo, Japan). Breast cancer risk and ER expression were estimated by computation of the odds ratios and their 95% confidence intervals (CIs). Odds ratios were considered significant when 1.0 was not included in the 95% CI. Results were considered significant at P < 0.05. In all odds ratios calculations women falling in the normal BMI range of 18.5-25 were used as the reference grouping.
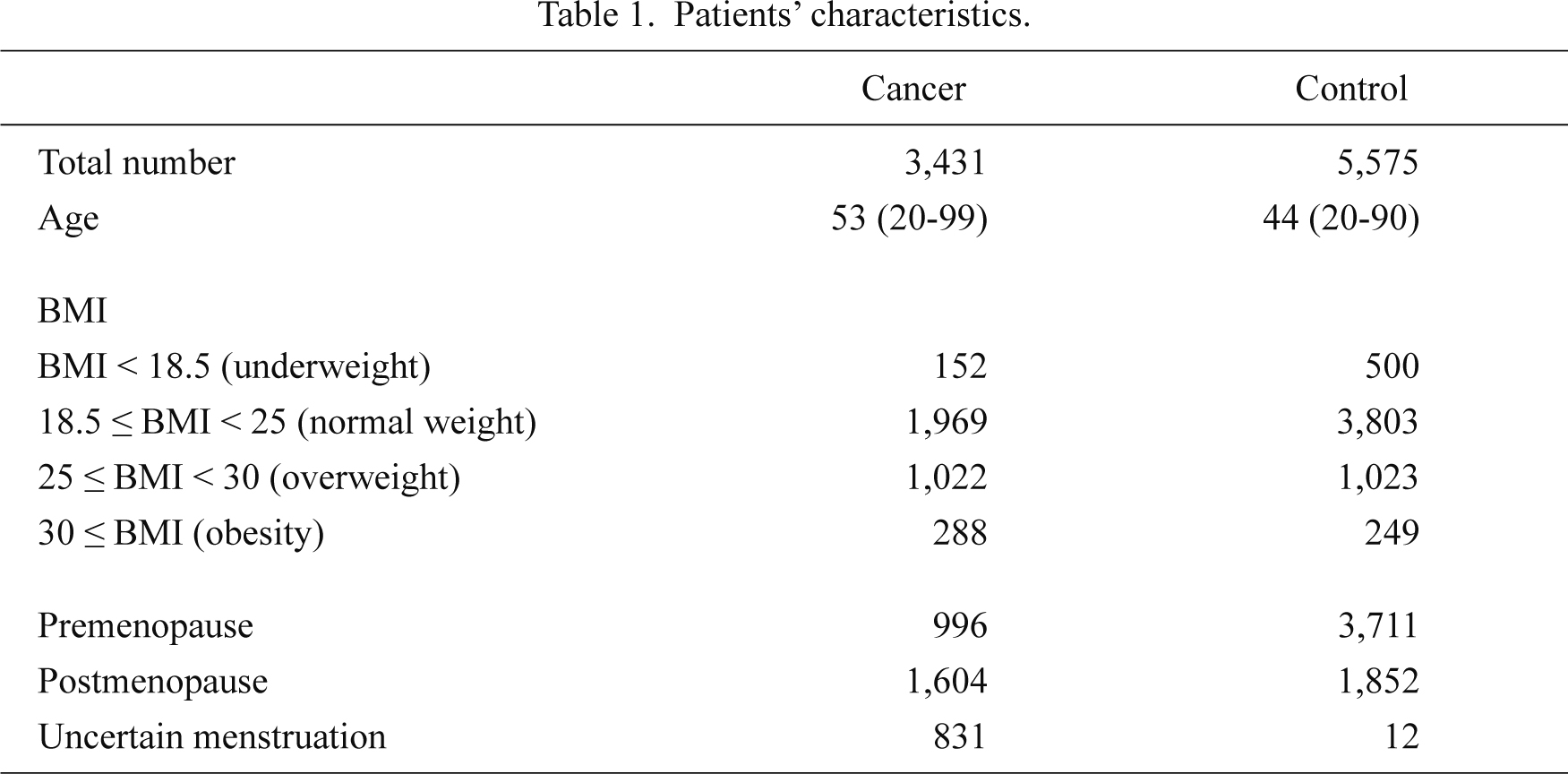
Patients’ characteristics.
The effects of BMI on breast cancer development risk during premenopausal and postmenopausal periods were assessed using odds ratios. Table 2 summarized the results of the correlation between BMI and breast cancer risk according to the status of menstruation. In premenopausal women being underweight was associated with a statistically significant reduction in odds ratio while being overweight or obese was associated with a statistically significant increase in odds ratio and hence risk of breast cancer. Similar statistically significant patterns were seen in the group of postmenopausal women.

The correlation between BMI and breast cancer risk according to menstruation.
Table 3 summarizes the results of the correlation between BMI and breast cancer risk stratified by the age of the patients. The women who were greater than 40 years in age and were either overweight or obese had a significantly higher risk of breast cancer development compared to the women in a normal weight range. The same tendency was also detected in 30-40-year-old women i.e., the women who were either overweight or obese tended to have higher incidence of breast cancer than those not. There were no statistically significant differences between underweight and non-underweight in any of the age groups.

The correlation between BMI and breast cancer risk according to age.
Table 4 summarizes the results of the correlation between BMI and ER status divided into premenopausal and postmenopausal groups. There were no statistically significant differences between BMI and ER status in the premenopausal period. However, women who were overweight or obese during postmenopausal ages were at higher rates of ER-positive breast cancer when compared to normal weight women (p = 0.002 and p < 0.001, respectively). There was no statistically significant correlation between BMI and ER status in underweight women in premenopausal or postmenopausal women.

The correlation between BMI and ER expression.
We examined the correlation between BMI and breast cancer of both premenopausal and postmenopausal women born, brought up and living in Okinawa. Results of our present study of Okinawan women are quite unique in terms of recent drastic and enormous changes of diet and lifestyle in one single community. To the best of our knowledge, this is the first study to examine whether BMI is associated with risk of breast cancer development or not in this population.
Results of previous meta-analysis studies suggested that high BMI during premenopausal period may protect against breast cancer development in later life, although the association did not reach statistical significance (Cheraghi et al. 2012). This trend has been also reported in several other studies showing a significant inverse association between body weight and breast cancer incidence in premenopausal women (Harris et al. 2011a, b). In contrast, the same meta-analysis demonstrated that increased BMI during postmenopausal period could significantly increase the risk of breast cancer development (Cheraghi et al. 2012). The increased risk in postmenopausal women associated with being overweight and/or obese is due to the fact that adipose tissue is the major source of estrogen following menopause (Cauley et al. 1989; Key et al. 2003). While the mechanism of protection by obesity in premenopausal women is unknown, the observation that young overweight women are more likely to have anovulatory cycles with less cumulative exposure to endogenous estrogen (Stoll 1994) or the greater clearance of estrogen by the liver in young overweight women (Potischman et al. 1996) resulting in a reduction in circulating hormones have been proposed as potential mechanisms.
Results of our present study demonstrated that the Okinawan women who were overweight and/or obese during premenopausal and postmenopausal ages had a statistically significant higher risk of breast cancer development compared to normal weigh women (BMI 18.5-25). This was particularly true in women who fell into age group greater than 40 years. These results clearly indicate that increased BMI was associated with increased risk of breast cancer in Okinawan women regardless of menopausal status.
This trend was inverted in underweight women who exhibited lower breast cancer risk. Though previous meta-analyses and international evaluation showed that being underweight is a risk factor among premenopausal women (Renehan et al. 2008), in our study being underweight was associated with lower breast cancer risk. However this requires further study to fully understand underlying mechanistic factors.
Many previous studies demonstrated that the association between BMI and risk of postmenopausal breast cancer is stronger for ER-positive breast cancer than ER-negative breast cancer (Feigelson et al. 2006; Suzuki et al. 2011; Sueta et al. 2012). However some previous studies demonstrated that premenopausal ER-negative breast cancer patients were more likely to be overweight and/or obese at diagnosis compared with ER-positive breast cancer patients (Millikan et al. 2008; Kwan et al. 2009). The results of this study demonstrated that there was statistically significant correlation between BMI and ER expression in the postmenopausal, but not premenopausal period.
Residents of the Okinawa archipelago historically have had one of the highest longevity rates in the world, attributable at least in part to a traditional diet that is low in calories but delicious and nutritionally balanced as described above (Suzuki et al. 2001; Todoriki et al. 2004; Willcox 2005; Willcox et al. 2007). However, coincident with the huge socio-cultural changes of the last 70 years, many of which are associated with the post-World-War-II American occupation, Okinawa now has the dubious privilege of having the highest rates of obesity within Japan (Takasu et al. 2007; Matsushita et al. 2008), with obesity currently the most serious public health problem in Okinawan women. It is therefore imperative to have more evidence on whether obesity is associated with increased risks of breast cancer development in these populations (Lee and Yee 1995; Pollack 1998; Yee 1998), and to provide clear information as to the other health hazards of overweight/obesity to women living in Okinawa islands. While the present study aimed to address this issue, it has several limitations. One is the selection bias because this study was conducted in a single institution. Therefore, results obtained in our present study may not represent the features of Okinawa residents as a whole. In addition, the data of environmental factors such as physical status and diabetes history were not necessarily available in this study. Therefore, we could not evaluate the environmental factors, BMI and others and this awaits further investigations for clarification.
In conclusion, this study provides the first evidence to suggest the association between increased breast cancer risk and BMI in an Okinawan population. Given the obesity epidemic associated with the extreme sociological and dietary changes brought about by the post-war occupation of Okinawa, this information provides essential guidelines on the management, treatment and future breast cancer risk in the Okinawan islands.
This work was supported, in part, by a Grant-in-Aid from Kurokawa Cancer Research Foundation. In addition, this work was partly supported by the grants from the Japanese Ministry of Health, Labor and Welfare.
The authors declare no conflict of interest.