2014 Volume 234 Issue 3 Pages 189-195
2014 Volume 234 Issue 3 Pages 189-195
Pain that occurs after a stroke lowers the quality of life. Such post-stroke pain is caused in part by the brain lesion itself, called central post-stroke pain. We investigated the analgesic effects of transcranial direct current stimulation (tDCS) in stroke patients through quantitative sensory testing. Fourteen participants with central post-stroke pain (7 female and 7 male subjects) were recruited and were allocated to either tDCS (n = 7) or sham-tDCS (n = 7) group. Their ages ranged from 45 to 55 years. tDCS was administered for 20 min at a 2-mA current intensity, with anodal stimulations were performed at primary motor cortex. The sham-tDCS group was stimulated 30-second current carrying time. Both group interventions were given for 3 days per week, for a period of 3 weeks. Subjective pain was measured using the visual analogue scale (VAS) of 0 to 10. Sensations of cold and warmth, and pain from cold and heat were quantified to examine analgesic effects. The sham-tDCS group showed no statistically significant differences in time. In contrast, tDCS group showed decreased VAS scores and skin temperature (p < 0.05). The threshold temperatures for the sense of cold and pain from cold increased (p < 0.05), and those for the sense of warmth and pain from heat decreased (p < 0.05). Our findings indicate that tDCS improved sensory identification and exerted analgesic effects in the stroke patients with central post-stroke pain.
Cerebrovascular disorders could result in central post-stroke pain (CPSP) that manifests burning pain, throbbing pain, aching pain, slashing pain, allodynia, and hyperalgesia continuously or intermittently in the affected side (Misra et al. 2008; Pickering et al. 2009). The incidence rate of CPSP is 8% to 35% of stroke patients (Hansson 2004). It occurs within 6 months after a stroke, and in the early stage, occurs in an area of hypoesthesia (Bowsher 1996).
Pain is largely spontaneous or evoked and worsens with diverse stimuli such as movement, touching, changes in temperature, or stress (Kumar et al. 2009). In addition, CPSP patients undergo dysesthesia such as allodynia (triggered by weak stimuli that do not cause pain in normal people), hyperalgesia (high-intensity pain easily brought about by weak stimuli), and spontaneous pain generated without outside stimuli (Boivie et al. 1989; Hansson 2004). Such changes in pain restrict motor function and physical therapy, leading to loss of motivation and negatively affecting patient quality of life. Therefore, active measures are needed.
Treatment is aimed at alleviating rather than completely relieving pain. Antidepressants and anticonvulsants can adjust hypersthenia of the nerves but do not selectively act on damaged nerves, and adverse effects, such as drowsiness, inertia, and dizziness can occur. Nonmedication treatments such as spinal cord stimulation, dorsal rhizotomy, and deep brain stimulation have been performed, but they require invasive surgical operation and patients are predisposed to complications due to long-term use of electrodes (Bae et al. 2010). Therefore, methods for relieving pain through noninvasive modulation are being sought.
Central pain occurs when the spinothalamic tract, thalamus, or tractus thalamocorticalis is damaged. Consequently, somatic senses are not normally delivered to the cerebral sensory cortex and are perceived as dysesthesia or pain (Nicholson 2004; Frese et al. 2006). Here, electrical stimulation to the cerebral motor cortex acts on the thalamus and is therefore presented as a treatment method for controlling abnormal excitation (Velasco et al. 2009). Bottom-up adjustment for activating the motor cortex is known to adjust pain perception through indirect effects on pain-adjustment regions such as the thalamic nuclei (Fregni et al. 2006a).
Recently, transcranial direct current stimulation (tDCS) has been used as a central neurostimulation technique, as it has been presented as an effective and safe noninvasive brain stimulation method (Kim et al. 2012). tDCS releases a weak current to the scalp and selectively triggers changes in neuron excitation in the local brain regions (Nitsche and Paulus 2000; Liebetanz et al. 2002), it affects the activity of sodium and calcium ion channels, adjusting the potential level of the neural network, and changes the activity of the local brain neurons in the relevant region (Nitsche and Paulus 2000; Liebetanz et al. 2002; Nitsche et al. 2003). Nonetheless, most research on tDCS thus far has been concerned with changing the excitability of the cerebral cortex, thereby affecting and adjusting movement, sensation, cognition, and exercise rehabilitation (Webster et al. 2006; Antal et al. 2007). Some reports describe the application of tDCS for pain resulting from a peripheral lesion (Boggio et al. 2009) or central pain due to spinal cord injury (Fregni et al. 2006a). However, research on CPSP is lacking.
Accordingly, this study examined the analgesic effect of cerebral cortex stimulation using tDCS in CPSP patients.
The study subjects consisted of 14 patients with central pain who had experienced a stroke and were able to verbally communicate (Mini-Mental State Examination-Korean version score, 25 points or higher). From among patients who complained of dysesthesia, hyperpathia, and allodynia, those with visual analogue scale (VAS) scores of 3 points or higher were diagnosed with CPSP. Those who had other verified causes of pain, such as reflex sympathetic dystrophy, radiculopathy of the cervical spine, or cancerous pain, or those who had a history of depression or drug abuse were excluded from this study (Greenspan et al. 2004). The 14 subjects were randomly and equally divided into a sham-tDCS group and a tDCS group. This study was approved by the institutional review board (IRB) of Dongshin University (IRB No. BM-004-01). The subjects received sufficient information from the researcher about the content and procedures of the study. They voluntarily consented to participate in this study (Fig. 1).
This study used a direct current stimulator (Phoresor II Auto Model PM850; USA) to assess the analgesic effect of tDCS on central pain, and sponge electrodes (5 × 7 cm2) were attached to the scalp. According to the international 10-20 system, the anode was attached to C 3 or C 4, the primary motor cortex (M 1) (Fig. 2). The hemisphere of stimulation was based on the hemiplegic side. When the right side was paralyzed, C 3 was stimulated, and when the left side was paralyzed, C 4 was stimulated. The cathode was placed over the contralateral supraorbital area. The intensity and current flow time were set at 2 mA and 20 minutes, respectively. tDCS was conducted three times per week for 3 weeks (Fregni et al. 2006a). In the sham-tDCS group, the same montage was used as in the tDCS group. However, the current was applied only for 30 seconds, which successfully prevented the participants from distinguishing it from active tDCS (Gandiga et al. 2006).
Flowchart of participants of the study.
tDCS, transcranial direct current stimulation; VAS, visual analogue scale.
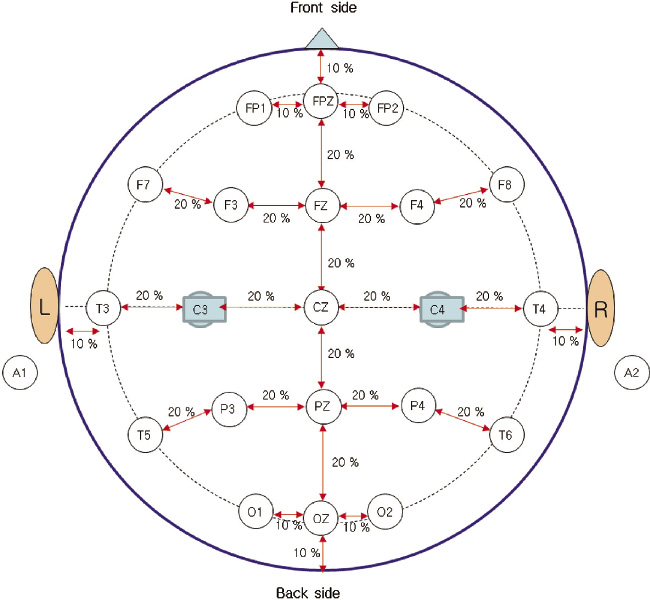
International 10/20 system of electrode placement.
The anode was attached to C 3 or C 4, the primary motor cortex (M 1).
Subjective pain: VAS was used to estimate pain intensity. The patients marked the pain intensity they felt on a stick without gradations. The distance from the starting point to the point marked by the patient was converted into a score. Zero points were given when there was no pain, and 10 points were given when pain was unbearable (Bijur et al. 2001).
Skin temperature: Skin temperature was measured before the treatment, right after the treatment, 1 week after the treatment, and 3 weeks after the treatment, using a surface thermometer (TES 1300, TES Co. Ltd., Taiwan). Skin temperature may be affected by the physical environment and skin condition; therefore, to maintain the same environment, the experiment was conducted in a test room where the temperature was maintained at 26°C. External factors were excluded, and measurement precision was ensured by making the patients comply with pre-experimental precautions for 6 hours before the measurement. Changes in temperature were measured at the representative area of complaint and on the contralateral side in each patient. That is, the temperature difference between the opposite side and the area with pain was calculated. Only cases in which the difference was 0.5°C or higher, were included in the analysis (Lee et al. 2001).
Quantitative sensory: For quantitative sensory measurement, a thermal sensory analyzer (TSA-II, MEDOC Co. Ltd., Israel) was used. Mean values were derived for the thresholds for cold sensation, warm sensation, cold pain, and heat pain in the areas where patients mainly complained of pain. A thermode (15 × 23 mm) was attached to the thenar area of the hand, and the reference temperature was set at 30°C. When the temperature increased or decreased by 1°C per second, the subjects were instructed to press the button when they felt a cold sensation, warm sensation, cold pain, or heat pain. The temperature at that moment was measured using a computer, and the direction of the current was changed so that the temperature of the thermode returned to the reference temperature. The temperature ranged from 0°C to 50°C, and the thresholds for cold sensation, warm sensation, cold pain, and heat pain were recorded. The thresholds for cold and warm sensations were tested four times, and the mean values were used for the analysis. Four to six seconds of rest time was allowed. The thresholds for cold and heat pain were tested three times, and a rest time of 10 seconds was allowed. The mean values were used for the analysis. When the subjects did not feel a cold sensation or cold pain even at 0°C, the values were determined to be 0°C; and when they did not feel a warm sensation or heat pain even at 50°C, the values were determined to be 50°C (Shin et al. 2000).
Statistical analysisIn this study, the mean and standard deviation were derived from the data using SPSS version 18.0 for Windows. According to a normality test of the results, all the variables were normally distributed. A repeated analysis of variance was conducted to test the significance of the changes in the measured values for each group. A post hoc test was performed for multiple comparisons, and all statistical significance levels were set at α = 0.05.
Among the 14 subjects, seven were female and seven were male. Their ages ranged from 45 to 55 years. The mean prevalence period was 14.6 months. Six and eight patients had paralysis on the right and left sides, respectively. Eight patients had a cerebral infarction, and six patients had a cerebral hemorrhage. Seven patients had a lesion in the thalamus (50%); three (21.4%), in the basal ganglia; and two (14.3%), in the brain stem. One patient (7.1%) had a middle cerebral arterial injury, and another patient had multiple injuries (7.1%) (Table 1).
Pain has complex aspects, but only one main aspect was recorded. Most (7/14, 50%) of the patients complained of tingling sensation, while four (28.6%) complained of a burning sensation, two (14.3%) complained of an aching sensation, and one (7.1%) complained of numbness (Table 1). With regard to pain area, most (5/14, 35.7%) of the patients had pain in the body and face, and two (14.3%) had pain in the face alone, three (21.4%) had pain in the body excluding the face, three (21.4%) had pain in the upper limbs, and one (7.1%) had pain in the lower limbs (Table 1).
The VAS pain score according to tDCS was 4.28 before the treatment and 4.14 three weeks after the treatment in the sham-tDCS group (no significant difference). In the tDCS group, the score was 4.29 prior to the treatment and 3.14 three weeks after the treatment, indicating a significant difference (p < 0.05). The difference in body heat between the pain and contralateral areas did not change significantly after the treatment (from 0.94 before the treatment to 0.82) in the sham-tDCS group but changed significantly after the treatment (from 0.96 prior to the treatment to 0.49) in the tDCS group (p < 0.05), showing an analgesic effect (Table 2).
In the quantitative sensory test using the TSA-II thermal sensory analyzer, the threshold for cold sensation did not significantly change from before to 3 weeks after the treatment in the sham-tDCS group (from 24.71 to 25.09) but changed significantly in the tDCS group (from 25.50 to 26.26) (p < 0.05). Within the same period, the threshold for the warm sensation did not change significantly in the sham-tDCS group (from 37.36 to 36.99) but changed significantly in the tDCS group (from 38.19 to 35.93) (p < 0.05). The threshold for cold pain did not change significantly in the sham-tDCS group (from 13.57 to 13.80) but changed significantly in the tDCS group (from 12.24 to 14.03) (p < 0.001). The threshold for heat pain did not change significantly in the sham-tDCS group (from 48.01 to 48.16) nor in the tDCS group (from 48.07 to 47.7) (p > 0.05) (Table 2).
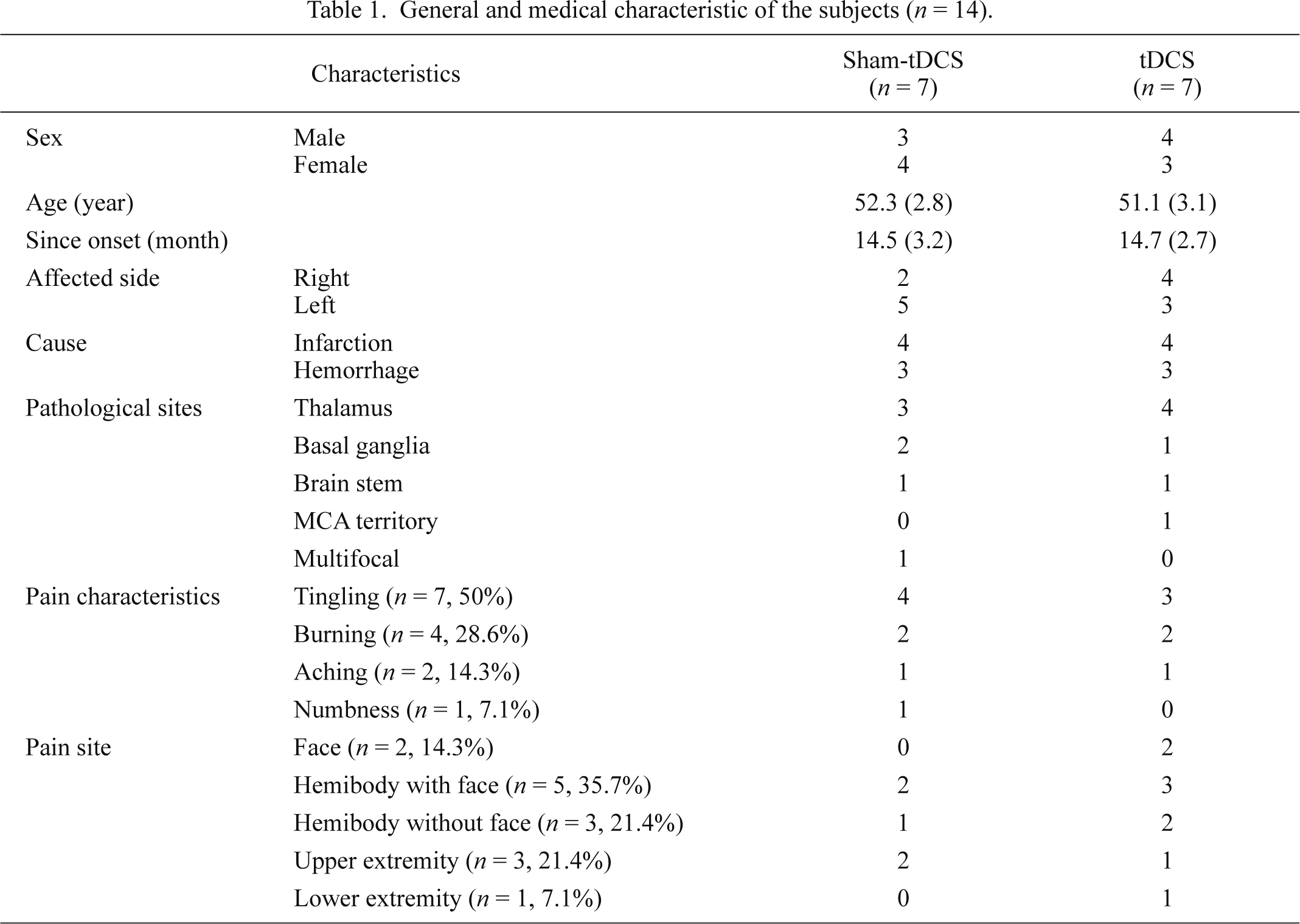
General and medical characteristic of the subjects (n = 14).
Data are expressed as mean (s.d.) values.
MCA, middle cerebral artery.
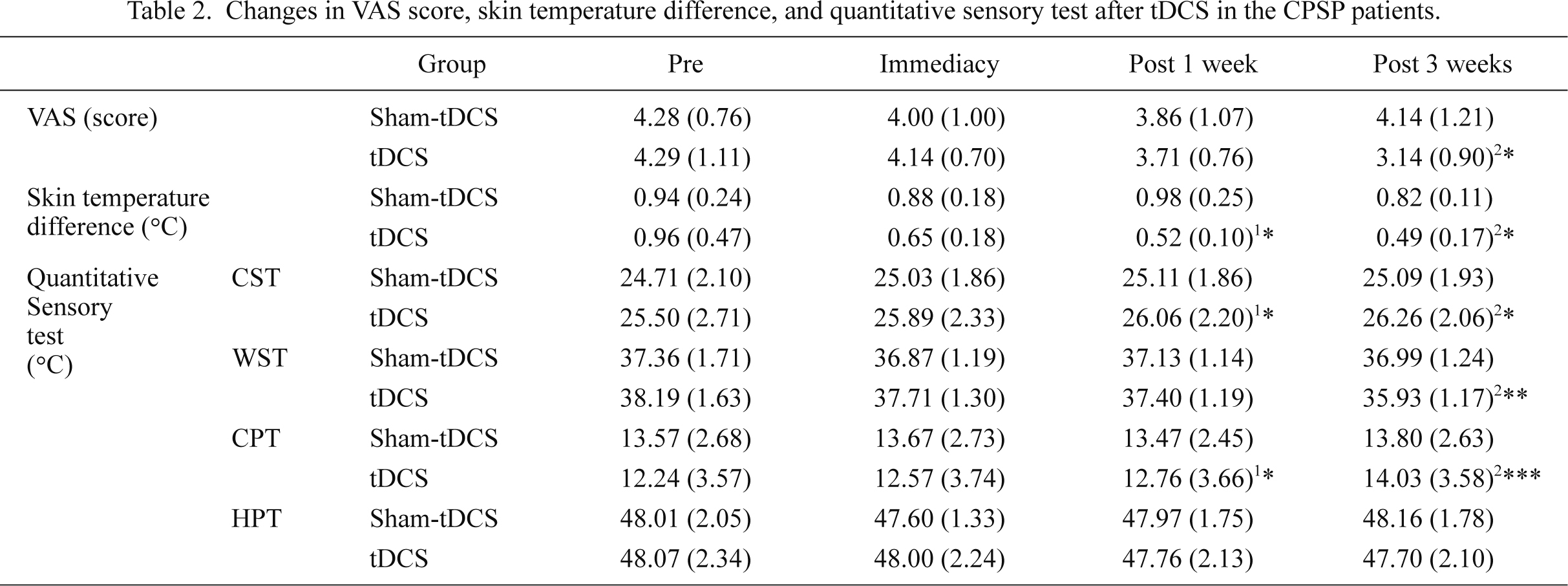
Changes in VAS score, skin temperature difference, and quantitative sensory test after tDCS in the CPSP patients.
Data are expressed as mean (SD) values.
1pre-post 1 week, 2pre-post 3 week, *p < 0.05, **p < 0.01, ***p < 0.001.
VAS, visual analogue scale; CST, cold sensation threshold; WST, warm sensation threshold; CPT, cold pain threshold; HPT, heat pain threshold.
The International Association for the Study of Pain defined pain from a lesion or functional disability in the central nervous system as central pain (Misra et al. 2008). In 1906, Dejerine and Roussy (1906) described the clinical symptoms of unique central pain in patients with thalamic injury, which sparked interest in thalamic pain syndrome (Boivie et al. 1989). However, the term was replaced with CPSP because its clinical characteristics were not precise and symptoms could be expressed in any region of the central somatic nervous system (Schott 1996).
The pain aspects of CPSP are spontaneous, continuous (Boivie et al. 1989), and diverse, including burning sensations, aching pain, tingling sensations, and laceration pain. CPSP can occur in a relatively small area such as the hands, a wide area (over half of the body), and sometimes in the trunk or the face (Boivie et al. 1989; Kumar et al. 2009). Dejerine and Roussy (1906) confined the lesion that triggers CPSP to the thalamus, but owing to the development of imaging diagnostic technology, diverse central regions were found to be related. Nevertheless, approximately 50% of cases were reported in the thalamus; other areas include the lateral medulla, internal capsule, and postcentral gyrus (Hansson 2004). In the present study, CPSP occurred most often in the thalamus and was also related to the basal ganglia, brain stem, and middle cerebral arteries.
Recently, interest has increased in neuromodulation approaches such as brain stimulation as new therapeutic approaches (Wall and Melzack 2002). Deep brain stimulation shows a high possibility of treatment effect (Wallace et al. 2004). Moreover, Fregni et al. (2006a) proposed that the more noninvasive the stimulation, the more effective it is and that an increase in the local activation of the motor cortex was considerably associated with control of central pain.
tDCS, one of the noninvasive brain stimulation methods, improves motor function in the hands and promotes implicit motor learning and working memory when a cathode is applied to the primary motor sensory and premotor areas. In addition, it ameliorates visuomotor learning when applied to the occipital lobe (Nitsche et al. 2003; Antal et al. 2004). In stroke patients, tDCS enhances aphasia or motor function of the upper and lower extremities (Hesse et al. 2007; Monti et al. 2008). It also improves the perception of pain (Antal et al. 2008) and various symptoms related to chronic pain syndrome (Fregni et al. 2006a, b).
However, no research has suggested the effect of tDCS on central pain in objectified quantitative results. Accordingly, this study intended to examine the analgesic effect of tDCS on CPSP patients.
The diagnosis of central pain is important for diagnostic purposes and therapeutic evaluation, but pain itself is a subjective expression and difficult to objectify. In particular, CPSP is pain in the area of sensory paralysis; and as a result, it is relatively difficult to diagnose (Park et al. 1996). The diagnosis of CPSP is largely based on clinical symptoms, and the elements of diagnosis are contact, movement, pain triggered by heat and coldness, hyperpathia, and changes in skin temperature threshold (Balazy 1992; Schott 1996).
Patients with central pain may undergo body temperature changes, such as skin temperature changes, due to the failure of the autonomic nervous system (Bowsher 1996). Therefore, this study used quantitatively measured skin temperatures for pain diagnosis and treatment (Lee et al. 2001). This study also utilized the VAS to assess the subjective degree of pain. According to the results, the temperature in the painful area in both groups was lower than that in the contralateral side. In the tDCS group, the difference between the two skin areas and the VAS pain score decreased over time after tDCS. This is means that the temperature in the painful area in the CPSP patients decreased (Balazy 1992). The smaller the difference in skin temperature, the lower the level of pain. This can be explained by the mechanisms through which central pain occurs. Owing to the systemic action of the sympathetic nervous system, the activity of the sympathetic nervous system increases, which decreases blood flow and lowers temperature (Sherman et al. 1989). Furthermore, the mechanism of pain in the connection pathway between the sympathetic and pain transmission nerve fibers affects the sympathetic nerve fibers, reducing skin temperature (Balazy 1992).
The quantitative sensory test was also used, as it is a standard psychophysical test for evaluating the wide-ranging somatosensory perception adjusted by the actions of the small and large fibers, and it is known as a method for determining loss of function of the diverse somatosensory pathways (Rolke et al. 2006; Bachmann et al. 2010b).
The present study used a thermal sensory analyzer for the quantitative sensory measurement, and mean values were calculated for the thresholds for cold sensation, warm sensation, cold pain, and heat pain in the areas where the patients complained of pain. Mark (2009) reported that the threshold temperatures for cold and warm sensations in CPSP patients are approximately 24°C and 38°C, respectively, whereas the threshold temperatures for the cold and warm sensations in healthy people were 30°C and 35°C, respectively. According to the results of the present study, the threshold temperatures for the cold and warm sensations in both groups were similar at 24-25°C and 37-38°C, respectively. This means that CPSP patients may differentiate temperatures when a cold temperature is lowered and when warm sensation is heightened owing to hypoesthesia. The threshold temperature for cold sensation increased significantly after tDCS stimulation over time, and the threshold temperature for warm sensation decreased significantly after tDCS stimulation over time, resulting in improvement of sensory differentiation.
Nociceptors are connected by Aδ and C fibers, and Aδ and C cold nociceptors and Aδ and C heat nociceptors respond when the skin temperature is 10°C or lower and 45°C or higher, respectively (Lindblom 1981; Pertovaara and Kojo 1985). In the present study, the threshold temperatures for cold and heat pain before the treatment in both groups were 12-13°C and 48°C, respectively. Shin et al. (2000) reported that Koreans’ normal threshold temperatures for cold and heat pains were approximately 16-18°C and 45-47°C, respectively. In the present study, cold pain in the CPSP patients greatly differed from that in healthy people, but their heat pain did not differ much. Such results are similar to the study results of a study by Ohara et al. (2004), which indicated that approximately 45% of CPSP patients with cold pain experienced hypoalgesia and approximately 7% of CPSP patients with heat pain underwent hypoalgesia. Because of hypoalgesia, CPSP patients felt cold pain at a lower than normal temperature and felt heat pain at a similar or slightly higher temperature than normal temperature. After tDCS stimulation over time, the threshold temperature of cold pain significantly increased, whereas that of heat pain significantly decreased, resulting in improvement of the hypoalgesia.
Bachmann et al. (2010a) reported that the cathodal stimulation of tDCS causes analgesic effect in healthy individuals. However, this study found that anodal stimulation of tDCS causes analgesic effect. This difference in results may be because analgesic effect in healthy individuals were generated through cathodal stimulation by reducing sensory transmission, but analgesic effect in stroke patients were generated through anodal stimulation by facilitate to areas of the brain involved in the normal sensation.
All the results thus far verified that tDCS had a significant analgesic effect on CPSP. The induction of changes in the electrical characteristics of neurological membranes in stimulated areas (Nitsche et al. 2005), inhibition of ascending pain transmission by the subcortical thalamic nuclei as a result of the local excitability changes, indirect effects in pain control areas due to upregulation from the motor cortex activation (Fregni et al. 2006a), and the adjustment of the abnormal activity of the thalamus through cortico-thalamic fibers (Tsubokawa et al. 1991) suppressed noxious stimuli signal transmission and increased the sensory perception threshold, which led to the analgesic effects. The present study results show that tDCS had a significant analgesic effect on CPSP, but additional research on the mechanisms for controlling pain and diverse conditions, such as the most appropriate polarity, intensity, time, and areas, is considered necessary.
The authors declare no conflict of interest.