2015 Volume 235 Issue 2 Pages 145-149
2015 Volume 235 Issue 2 Pages 145-149
The perinatal mortality rate in Japan has recently been at the lowest level in the world. However, the perinatal mortality rate of Shiga prefecture has been continuously higher than the Japanese average. The reason for this has not yet been explained. The perinatal mortality rate comprises both stillbirths and neonatal deaths. As stillbirths were almost double neonatal deaths, we focused on the stillbirths to determine how they might be prevented. All of the stillbirth certificates in Shiga Prefecture during 2007-2011 were inspected. On the basis of that information, we designed the original questionnaire and sent it to each obstetrician submitting a death certificate to obtain further information associated with the stillbirth. Reviewing retrospectively returned questionnaires by a peer-review team, we evaluated the possibility of preventing stillbirth along with recommendations for prevention. There were 252 stillbirths among 66,682 deliveries in Shiga during this period. We were able to analyze 188 stillbirths (75%). The audit conference judged that 47 cases of them (25%) were determined to have had some possibility of prevention with seven cases (4%) having strong possibility. We identified major causes of preventable stillbirths, including substandard obstetrical management, delayed referral of high-risk women from primary obstetrical clinics to higher perinatal centers, and delayed visits of pregnant women with decreased fetal movements to clinics or hospitals. Based on the results of this study, we conclude that education for pregnant women is required as well as the necessity of improving obstetric care to prevent stillbirths.
The perinatal mortality comprises both stillbirths after 22 gestational weeks and neonatal deaths up to 7 days after birth. Although the perinatal mortality rate in Japan is the lowest level in the world (World Health Organization 2012), it can vary more than twice as much from region to region. Shiga is a prefecture with one of the highest fertility rates in Japan, yet the perinatal mortality rate in Shiga prefecture has been continuously higher than the Japanese average in this last decade (Ministry of Health, Labor and Welfare 2012). For understanding these differences and considering the improvement of the regional perinatal health care, a population-based study is indispensable. Focusing on stillbirths, the primary component of perinatal mortality, we analyzed regional stillbirths based upon stillbirth certificates retrospectively. Firstly, we investigated stillbirth backgrounds in our region. Secondly, we classified the possibilities of preventable stillbirths and collected some recommendations for prevention.
There are about 13,000 deliveries per year in Shiga, 65% of them in 30 primary obstetric clinics (defined as “clinics”) and the remaining 35% in eleven hospitals (defined as “hospitals”) including seven general hospitals, two secondary and two tertiary perinatal centers.
We organized a peer-review team consisting of six obstetricians and six neonatologists from a primary obstetric clinic, general hospitals, and perinatal centers to analyze objectively perinatal death cases in Shiga prefecture since 2012. The 252 stillbirths after 22 gestational weeks among 66,682 deliveries in Shiga during 2007-2011 were registered by the National Vital Statistics in Japan.
All of the stillbirth certificates were inspected directly with permission of the Ministry of Health, Labor and Welfare in Japan. On the basis of that information, we designed an original detailed questionnaire and sent it to each obstetrician submitting the stillbirth certificate. The questionnaires filled out by the obstetrician were returned and reviewed retrospectively by the peer-review team. Analyzing them, backgrounds of the stillbirths including location, primary cause and circumstances were traced. In addition, we classified them based on the possibilities of prevention into three grades and we determined the recommendations for preventable stillbirths. The statistical significance of the differences was assessed with a chi-square test.
This study is approved by the Institutional Review Board, Shiga University of Medical Science.
We could analyze 75% (188/252) of stillbirths including 23 cases of other prefectures’ institutions, but were unable to analyze the remaining 25% of the stillbirths because the questionnaires were not returned. Among the 188 stillbirths, 106 cases were initially submitted by hospital, and 82 cases were submitted by primary clinics. However, out of the 106 stillbirths submitted by hospitals, 38 cases were reclassified as follows: 25 cases were non-emergency maternal transfer to hospitals after being diagnosed at primary clinics, twelve were transfer-related due to diagnosis of stillbirth on the way to the hospital during maternal emergency transfer or a short time after arrival, and one was a home birth. Thus, the 25 cases were included with the stillbirths diagnosed at primary clinics; namely, the total number of stillbirths submitted by primary clinics was increased to 107 (Fig. 1). In contrast, the number submitted by hospitals was decreased to 68 cases.
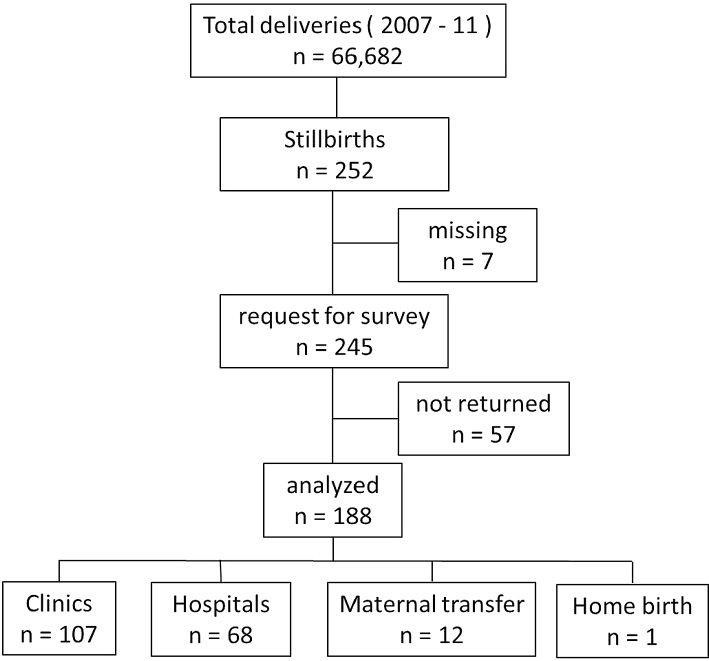
Overview flowchart of this study.
The primary causes of 188 stillbirths at diagnosed places are listed in Table 1, based on the modified category as previously described (Kodama et al. 2007). Fetal growth restriction was defined as weights under the 10th percentile of the Japanese standard curves diagnosed by ultrasound or postmortem examination. Autopsy of the fetus was performed in five cases (2.7%) of the 188 cases. We were able to classify explainable causes of 70% (132/188) but were unable to identify 30% (56/188) due to lack of sufficient information to explain as primary causes. Umbilical cord-related problems constituted the most common explainable cause of stillbirths both in hospitals and clinics. Placental abruption was the most common cause in the transfer-related group, which was the second most in all. Umbilical cord-related problems in clinics were significantly higher than in hospitals, whereas congenital anomalies in hospitals were significantly higher than in clinics. There were four and two stillbirths associated with maternal thyroid disease and type 2 diabetes mellitus, respectively. However, these six cases were not classified as explainable cases, because these maternal diseases were not severe.
Among causes of stillbirths except for prematurity (Table 1), placental abruption was associated with a higher proportion of stillbirths after 27 weeks’ gestation (19 cases among 130 cases; 14.6%), compared to one stillbirth among 58 cases (1.7%) before 27 weeks’ gestation. The difference was statistically significant (95%CI, 5.9%-19.8%; P = 0.008). Placental abruption was also responsible for 15 stillbirths among 98 cases (15.3%) after 31 weeks’ gestation and 5 stillbirths among 90 cases (5.6%) before 31 weeks’ gestation (95%CI, 1.2%-18.3%; P = 0.03).

Causes of stillbirths with locations Causes of stillbirths in relation to locations and gestational age.
Locations are the places where fetal demise was diagnosed primarily.
There were 131 stillbirths diagnosed at outpatient departments (OPD) in hospitals and clinics. They were classified according to the reasons for visiting OPD (Table 2). Maternal perception of decreased or loss of fetal movements was the most common reason (47: 13 in hospitals and 34 in clinics; 36%) for visiting the OPD, and regular visit was the second most common reason (26: 5 in hospitals and 21 in clinics; 20%). There was no significant difference between hospitals and clinics in these two reasons.

Main reasons for visiting outpatient departments.
The audit conference classified all stillbirths according to the possibilities of the prevention into three groups; easily avoidable, somewhat avoidable and unavoidable. We classified the following cases as unavoidable. Unavoidable cases constituted pregnant women who regularly visited an obstetrician as well as ones who went immediately after perception of fetal movement loss or unusual abdominal pain. Also pregnant women with maternal complications of pregnancy that were not severe and were well controlled by the obstetrician and ones with standard diagnosis or medical management in obstetric care were assessed unavoidable. In addition, high-risk pregnant women in clinics who were transferred timely to higher perinatal centers were classified as such. The cases except for these unavoidable ones were classified as somewhat or easily avoidable according to our assessment of the possibility of their prevention.
We concluded that 68% (127/188) of stillbirths could not have been avoided. On the other hand, 25% (47/188) of them were determined to have been somewhat avoidable and 4% (7/188) easily avoidable. With the remaining seven cases, the possibilities of prevention were unable to be estimated due to lack of sufficient information.
RecommendationsWe concurrently determined recommendations for preventing stillbirth in each of what we had determined to be avoidable cases to assess the degree of their possible prevention (Table 3). Recommendations were classified into those for obstetricians and those for pregnant women. The most common ones for obstetricians were related to the improvement of diagnosis or medical management for pathological conditions of mother or fetus. There were 22 stillbirths related to substandard maternal management including with managing cervical incompetence and threatened premature labor, and also related to failure of antenatal diagnosis of fetal anomalies and heart rate monitoring of fetus.
The next most common recommendations for obstetricians suggested earlier maternal referral from clinics to higher perinatal centers. We had twelve stillbirths due to delay in maternal referral or transfer in spite of the necessity of maternal or neonatal intensive care, including fetal growth restriction, premature labor, multiple pregnancy, and hydrops fetalis.
Additionally, we had 42 recommendations for pregnant women, the number of which was almost the same as ones for obstetricians. The most common ones for pregnant women were that they needed to be apprised of the urgency of earlier visits in the advent of their recognition of the decreased fetal movements (DFM), as there were 32 stillbirths related to such delays in visitation to OPD after maternal perception of DFM.

Recommendations of stillbirth prevention for obstetricians or pregnant women.
FGR, fatal growth restriction; PROM, premature rupture of the membrane; PIH, pregnancy-induced hypertension.
In this study, we ascertained two important issues. Firstly, we investigated stillbirth backgrounds in our region. Next, we found that some of these could have possibly been prevented and we decided upon some recommendations for future prevention of such cases.
Investigating stillbirth backgrounds in our region, we found a significantly higher proportion of umbilical cord-related problems in clinics than in hospitals resulting from the diagnosis of overcoiled cords without unified criteria. As the overcoiled cord-related problem is associated with fetal demise, an antenatal measuring umbilical cord coil index is recommended (Machin et al. 2000; Baergen 2007). Although overcoiled cords comprised about half of umbilical cord-related problems in clinics, umbilical cord coil indexes were not measured in any stillbirths. It was very difficult to identify umbilical cord related problems as a primary cause of stillbirth, because autopsy of the fetus was performed only in 2.6% of the stillbirths in our region. If there was no other cause other than umbilical cord related problems in the returned questionnaires submitted by the primary obstetricians, the peer-review team had to identify it as the cause of stillbirth. As a result, the number of umbilical cord-related problems in clinics was possibly overestimated. In addition, the result that the ratio of placental abruption before 37 weeks increased with gestational age was consistent with a previous study (Ananth and Wilcox 2001). Our result also indicated that DFM was the most common reason for visiting OPD, which is consistent with previous studies (Olesen and Svare 2004; Sinha et al. 2007). Excessive delay in maternal reporting of DFM is associated with stillbirths (Grant et al. 1989; Frøen et al. 2001). There were quite a few stillbirths with delayed reporting (> 48 hours) of DFM in this study. It might be effective that all pregnant women should be informed about the association between DFM and stillbirth in clinics or hospitals during early pregnancy to recognize the importance of DFM. The hypothesis that an earlier maternal report would prevent stillbirths needs further study.
The next important issue in this study is preventing stillbirths. We showed two points in terms of prevention. One is the possibility of preventing stillbirths. In this study, 4% of stillbirths were judged to be easily preventable and 24% of them were somewhat preventable. The proportion of preventable stillbirths in our study seems to be different from another study which reported that 11% of them were preventable (Sameshima et al. 2008). As we classified preventable stillbirths into three grades according to their relative possibility, it is difficult to compare the proportion of preventable stillbirths between these two studies. Secondly, in terms of prevention in our study, we were able to suggest some recommendations for finding possible ways to reduce stillbirths. We categorized them according to our assessment of their degrees of possibility. As we found some cases in clinics with substandard obstetrical care, lack of recognition of fetal growth restriction, and subsequent delay in referral to higher perinatal center, we were able to make specific recommendations for the respective obstetricians in these clinics. In addition, we concluded with recommendations for pregnant women including earlier visitation upon perception of DFM or unusual abdominal pain, and receiving obstetrical care in pregnancy. The target of these recommendations was for pregnant women and the public in addition to obstetricians. We indicated that specific directions would be needed not only for obstetrical care providers but also for care receivers to prevent stillbirths. Improvement of obstetrical care and educating pregnant women might improve perinatal outcome. Also, as 0.18% (123/66,682) of total deliveries were assessed as unpreventable stillbirths, we discussed that the risk of unavoidable stillbirth should be informed to those who fully expect a normal delivery.
Our study has a limitation in that the surveillance did not cover all stillbirths in our regional population. As some of the questionnaires were not returned, we failed to analyze 25% (64/252) of stillbirths in our region, which is higher than another population-based study (Kodama et al. 2007). In addition, the study design, methodological point of view and the recommendations in our study are underqualified for the epidemiological prospective study, because this is a retrospective population-based study. But, nonetheless, we believe that specific recommendations for obstetricians and pregnant women would be useful to prevent stillbirths.
We showed stillbirth backgrounds and recommendations for preventing stillbirths on the basis of our regional study. Although we could not identify the factors of higher perinatal mortality rate in Shiga prefecture than the Japanese average, this study indicates that there is the possibility to reduce the number of stillbirths in our region. We have concluded that education for pregnant women and the public is required as well as improving obstetric care to prevent stillbirths. This study might contribute to the improvement of perinatal outcome not only in our region but also other areas.
This study was supported by a grant No. 23590594 from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
We would like to express the appreciation to the peer-review team members: Masafumi Koshiyama MD, Yukiyasu Sato MD, Kenji Nakamura MD, Daisuke Fujisawa MD, Takahide Yanagi MD, Shoji Kaku MD, Kashirou Nishizawa MD, Masahito Yamamoto MD, Yoshihiko Hayashi MD, Asuka Higuchi MD, Tsutomu Asano MD and Tetsuya Nomura MD.
The authors declare no conflict of interest.