2015 Volume 236 Issue 3 Pages 169-174
2015 Volume 236 Issue 3 Pages 169-174
The shortage of medical workforce in rural areas is a global long-standing problem. Due to the severity of shortages in the medical workforce, Mie prefectural government has collaborated with a medical school and the municipal governments to increase the rural medical workforce. Since 2010, this collaboration has led to an annual lecture series on rural practice for medical students. We distributed questionnaires at the beginning and end of the lecture series to examine the effect of this program. The questionnaire consisted of two parts that included an understanding of rural practice and the motivation to work in rural areas. The lecture series significantly improved the responses to the following questions “Rural practice is interesting” (p < 0.001), “Rural practitioners can deliver adequate medical care” (p < 0.01), “Rural practitioners cannot go back to urban areas” (p < 0.001), “I want to be a rural practitioner” (p < 0.001), “Healthcare facilities in rural areas have been developed” (p < 0.001), “Rural practitioners can be a specialist” (p < 0.001), and “Rural residents can be served adequate healthcare service” (p < 0.01). The percentage of students who desired to work in rural areas increased significantly (11.1% vs. 23.9%, p = 0.04). A lecture series on rural practice enhanced the motivation of medical students and their interest in a rural career. While collaboration between the local government and medical school rarely occurs in planning medical education programs, this approach may offer a promising way to foster local health professionals.
The shortage of medical workforce in rural and remote areas has been documented across many countries and represents a global long-standing problem (Rabinowitz et al. 2001; Duplantie et al. 2007; Gum 2007; Henry et al. 2009; Wilson et al. 2009; Isaac et al. 2014; Jamar et al. 2014). Within Japanese society, the shortage of medical workforce in rural areas likewise poses a very serious concern and has led to a variety of medical problems (Nomura et al. 2009; Tani et al. 2009; Toyabe 2009; Takata et al. 2011; Tanihara et al. 2011). While there are fewer physicians in Japan (2.3 per 1,000 population) compared to other developed countries (World Health Organization 2014), the shortage of medical workforce in rural areas is linked to both the lower absolute numbers of physician as well as the mal-distribution of physicians (Koike et al. 2009; Takata et al. 2011).
As the population of Japan continues to age, it is projected that individuals aged > 75 years will comprise approximately 20% of the population in 2030 (Tani et al. 2009). Population aging has already become a more extensive problem in rural areas. Because aging increases the demand for health-care, it is anticipated that in the near future, the shortage of physicians will affect many aspects of the social infrastructure in Japan (Yuji et al. 2012).
Prior studies have offered several strategies to resolve this issue, such as introducing an academic year spent in a rural setting, granting scholarships in return for a contract of service in rural areas and selecting students of rural origin (Rabinowitz 1988; Inoue et al. 1997; Rabinowitz et al. 1999; Sempowski 2004; Halaas et al. 2008; Matsumoto et al. 2008; Barnighausen and Bloom 2009; Isaac et al. 2014; Puddey et al. 2014). However, no single strategy has apparently been successful.
Mie Prefecture, one of 47 prefectures, is a middle-sized jurisdictional subdivision located in central Japan. Due to the severity of shortages in the medical workforce, Mie prefectural government, the municipal governments in Mie and Mie University Faculty of Medicine have made initiatives, including the clinical practices in rural areas, individually. Each institution has made much effort to create plans, recruit the participants and establish the required budget. Although the purpose of each initiative was the same, to acquire the medical workforce, making initiatives individually was not efficient. Therefore, the prefectural government of Mie collaborated with Mie University Faculty of Medicine and the municipal governments in an effort to increase the medical workforce. One of several initiatives implemented through this collaboration is a lecture series on rural practice for first-year medical students. Since 2010, we have led to the annual lecture series. Every year, we continuously revised the contents of the lectures to improve it. The aim of the lecture series is to facilitate an understanding of rural health-care and to motivate the students to choose careers within the rural community.
To our knowledge, little is known as to whether the educational program offered through the lecture series on rural practice improves student interest in a rural career. Therefore, we have conducted a survey to examine the effect of this program.
This study was a descriptive pre- and post-intervention study using questionnaires. First, we organized a lecture series involving six lectures concerning medical practice in rural areas in 2014. We appointed six clinicians as lecturers. Each clinician had been working in a rural community or had experience in rural practice. The content for the lecture series was determined during the course of planning by the prefectural officers in charge of the program independently from the university teachers (Table 1). For each lecture, the lecturers were requested to emphasize their experiences in rural community. Each lecture was comprised of a 60-minute presentation using PowerPoint (Microsoft Corporation; Redmond, WA, US) materials and a 30-minute discussion with the students. The lectures were given to 125 medical students attending the first of six years of medical education as a required subject. This study was performed in accordance with the Helsinki Declaration and was approved by the internal review board.

Topics covered in the lecture series.
*A large hospital indicated a facility with > 100 hospital beds; a small hospital had <= 100 beds.
**Kamishima island is one of the remote islands in Mie prefecture. Although the island has the population of approximately four hundred, only one doctor has been providing medical service to the residents.
We administered questionnaires in a blinded manner once at the beginning (‘pre-study’) and once at the end of the lecture series (‘post-study’). Fig. 1 lists the questionnaire items concerning rural practice. The questionnaire consisted of two parts addressing the following topic, respectively: (1) the understanding of rural practice, and (2) motivation to work in rural areas. Part 1 was comprised of 16 declarative statements. For each statement, students evaluated their current impression on a 10-point scale ranging from 0, which indicated disagreement with the statement, to 10, which signified agreement. In Part 2, the students were posed a four-choice question concerning their motivation to work in rural areas and a five-choice question inquiring about the length of time they intended to work in rural areas.
All students provided informed consent prior to completing the questionnaire.

Questionnaire items addressing rural practice.
The figure lists the questionnaire items concerning rural practice.
Because both parts in the questionnaire were administered in a blinded fashion, we could not identify the individual students. We therefore used a Mann-Whitney U test for non-parametric distributions in lieu of the Wilcoxon signed rank sum test to determine the differences between the pre- and post-study groups. The chi-square test or Fischer’s exact probability test was performed in a factor analysis for categorical variables. All statistics were performed using EZR statistical software (Saitama Medical Center, Jichi Medical University, Saitama, Japan) (Kanda 2013). A p value < 0.05 was considered statistically significant.
We collected 104 pre-study and 94 post-study questionnaires. Five students prior to the lecture series and one student following the lecture series did not consent to the study. Part1 was not entirely completed in 9 of the 104 pre-study questionnaires whereas all items in Part 1 were completed in the post-study questionnaires. Therefore, we analyzed responses for part 1 based on a total of 90 pre-study and 93 post-study questionnaires. For Part 2, only one post-study questionnaire had a missing response to the first question “Do you want to work in rural areas?” (Fig. 2).
Table 2 represents the results for Part 1 items which addresses the students’ understanding of rural practice. Among the 16 items, the pre-study and post-study responses differed significantly for the following 8 items: 1) Rural practice is interesting (6.1 vs. 7.6, respectively; p < 0.001), 2) Rural practitioners can deliver adequate medical care (6.7 vs. 7.5, p < 0.01), 3) Rural practitioners cannot go back to urban areas (5.4 vs. 4.0, p < 0.001), 4) I want to be a rural practitioner (5.6 vs. 6.8, p < 0.001), 5) Healthcare facilities in rural areas have been developed (4.4 vs. 5.6, p < 0.001), 6) Rural practitioners can be a specialist (5.2 vs. 6.2, p < 0.001), 7) Rural residents can be served adequate healthcare service (5.8 vs. 6.5, p < 0.01), and 8) Rural practitioners have no privacy (3.7 vs. 4.7, p < 0.01).
Table 3 summarizes the responses for Part 2 concerning the motivation to work in rural areas. With respect to the first question “Do you want to work in rural areas?”, the percentage of students who desired to work in rural areas increased significantly (11.1% vs. 23.9%, p = 0.04) following the lecture series. The percentages of students who were contemplating working in rural areas (30.0% vs. 17.4%, p = 0.07) and those who did not want to work in rural areas (6.7% vs. 4.3%, p = 0.72) decreased, but the differences between the pre-study and post-study frequency of responses were not significant.
Students affirming the statement “I am wondering whether to work in rural areas” or “I don’t want to work in rural areas” were directed not to answer the second question “How long do you want to work in rural areas?”. Thirty five students in the pre-study questionnaire and 25 in the post-study questionnaire did not respond to the second question (Fig. 2).
For the second question, the percentage of the students who chose to work in rural areas ‘from 1 to 2 years’ increased significantly in the post-questionnaire compared to the pre-study questionnaire (29.1% vs. 56.7%, respectively; p < 0.01). Conversely, the percentage of students electing to work ‘more than 5 years’ decreased significantly (14.5% vs. 3.0%, p < 0.05).

Flow-chart.
The figure is a flow-chart of this study.
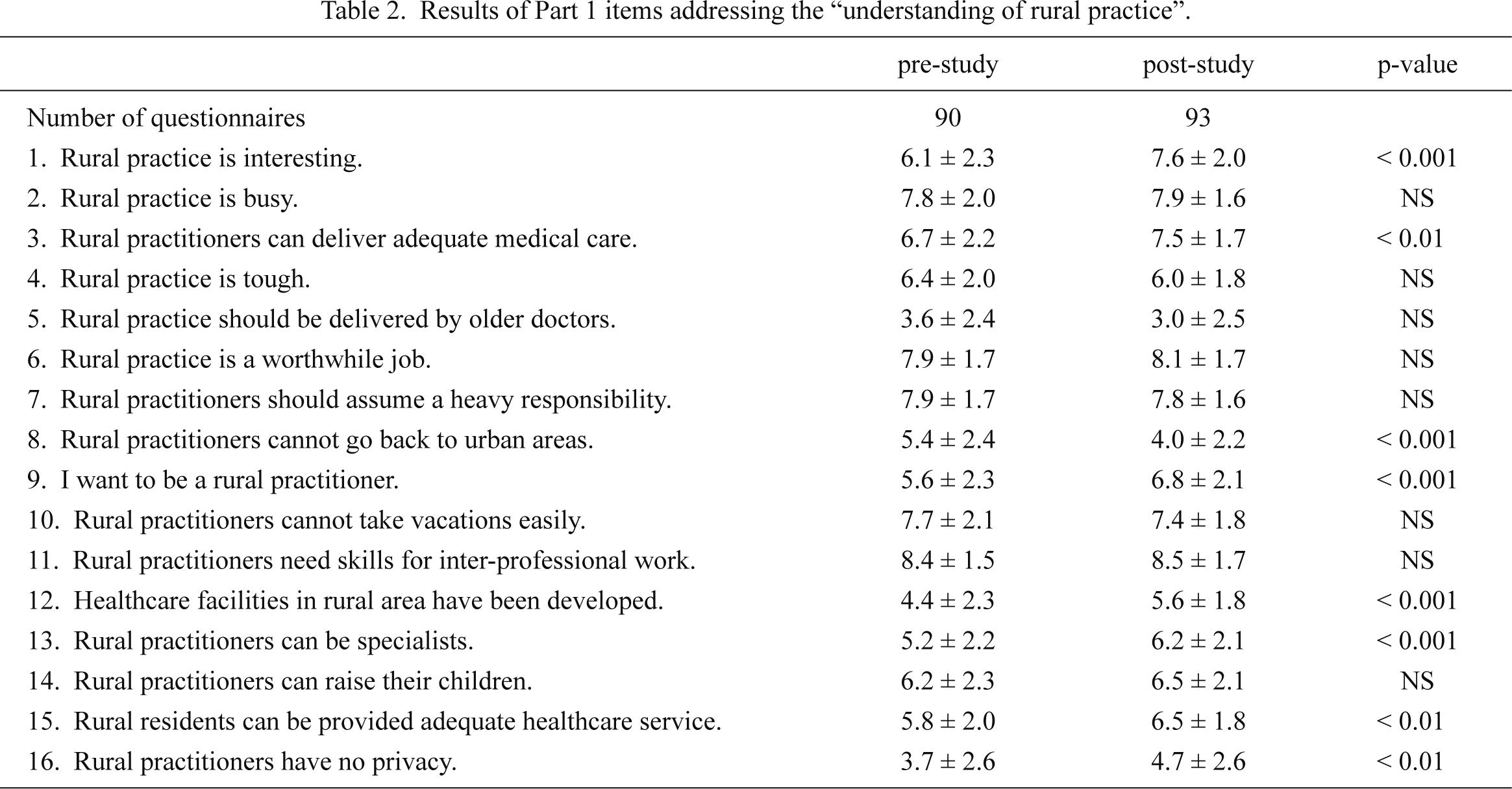
Results of Part 1 items addressing the “understanding of rural practice”.
Values for the pre-study and post-study scores represent the mean ± standard deviation.
NS, not significant.

Results of Part 2 items addressing the “motivation to work in rural areas”.
NS, not significant.
Following the lecture series comprised of six individual lectures on rural practice, the percentage of students desiring to work in rural areas and become rural practitioners increased significantly. Thus, our findings showed that the educational program enhanced the first-year medical students’ understanding and motivation to pursue a rural career.
When compared with practitioners working in urban areas, rural practitioners tend to carry a heavier workload, are requested to provide a wider range of services, and feel a higher level of clinical responsibility due to their relatively isolated situation (Strasser 2001). In addition, some attitudinal and perceptual barriers may discourage students and graduates from entering a rural career. Furthermore, some medical students may not clearly understand rural practice and the roles of practitioners in rural communities. As a result, many practitioners have preferred choosing an urban career over a rural career, which has led to the shortage of medical workforce in rural areas.
To improve this serious situation in the rural health-care system, the policymakers and educators are continuously challenged to find effective methods for fostering rural physicians (Rabinowitz et al. 2001; Matsumoto et al. 2004; Tani et al. 2009; Walker et al. 2012; Isaac et al. 2014; Jamar et al. 2014). We have introduced many initiatives including this program in collaboration with Mie University Faculty of Medicine as well as with municipal governments within the prefecture. Our collaboration offers several advantages. First, both the governments and university provide substantial information and have access to many personnel connections and facilities within the rural areas. The collaboration allows us to share and collect information about rural practice. In this case, we could appoint lecturers who had a little relationship with the university. Second, governments can offer a different perspective from the university, which enhances the ability to convey diverse perspectives to medical students attending the lecture series. Third, we can continue to be aware of the need to acquire medical workforce in rural areas. Following the lecture series, the university staff gained direct knowledge about rural practice, which in turn, may have potentially enhanced their interest in a rural career.
Our program invited local doctors to a lecture hall in a medical school and attempted to convey their experiences directly to medical students who had just started their education. We expected that students would gain knowledge of the “real-world experience” in rural settings. This lecture series may assist young students in understanding the significance of community medicine and stimulate them to work in rural areas equipped with a clear vision for growth as medical doctors. In this program, we appointed lecturers from diverse backgrounds, including specialists at a relatively large hospital in the region, family physicians working in a remote area, and a female doctor continuing her job while taking care of her children. These clinicians represent good role models for students.
Furthermore, some lecturers who were competent specialists expressed the belief that a rural career was useful, and that all clinicians, even those who work as specialists in large hospitals, were required to possess some degree of skills relating to general medicine and public health. Rural practitioners tend to provide a wide range of services and must focus on not only the patient’s disease but also the patient’s background and the health delivery system. Therefore, rural practice is an effective method for acquiring diverse knowledge and skills, even for practitioners who have worked for short period in rural areas.
Among the affirmative responses, only the number of students considering work in rural areas for more than 5 years had decreased after the lecture series. It is suspected that after contemplating information from the lectures, the students had concluded that experience in both rural and urban areas would be beneficial for their growth.
Another program on community medicine has been introduced in the curriculum for first- and second-year students at this medical school. In this program, a survey on community health problems is conducted by a group of four students using an anthropological interview method. In addition, the group engages in health promotion activities for members of the designated community. Furthermore, our collaboration has involved several other clinical practices in rural areas every year. Among these practices, the government officers have often accompanied the students and discussed the significance of rural practice during the course of practice. The combination of lectures and practical training in rural areas may produce synergic effects for enhancing the students’ understanding of community medicine.
This study has several limitations. First, we enrolled a small sample of students. Second, we evaluated only the immediate effect but not the long-term outcomes of the educational program. Third, there was potential for selection bias since the participants in this study were limited to first-year Japanese medical students confined to a single medical university. Therefore, the results may not be generalized to other institutions and other grades. Furthermore, the students who were not interested in a rural career may not have completed the questionnaires and might tend to be absent from the lectures. This might have influenced the results.
In conclusion, a lecture series on rural practice has enhanced the motivation of medical students and their interest in a rural career. Among various programs, this method for instruction may play an important role in community medicine education. While collaboration between the local government and medical school, such as in our study, rarely occurs in planning medical education programs, this approach may offer a promising way to foster local health professionals. Because no single strategy has yet to be effective, further studies are necessary to establish a successful strategy to resolve the shortage of rural medical workforce.
This study was supported by the Center for Medical and Nursing Education, the Mie University Faculty of Medicine and the Mie Municipal Development Corporation. We are grateful to Dr. Keigo Koizumi, Dr. Yu Nobuoka, Dr. Kenichi Sakakura, Dr. Chizuru Yabe, Dr. Kazumasa Nakata, and Dr. Takaaki Suzuki for providing the lectures. And we would like to acknowledge the valued assistance of Katsuhiko Matsuda, Shigeaki Aoki, Satomi Maeda who set up the survey and collecting the data.
The authors declare no conflict of interest.