Abstract
After the Great East Japan Earthquake of 2011, there has been a concern about health problems among children. Therefore, we investigated the prevalence of wheeze and eczema symptoms and associated factors among children in areas primarily affected by the disaster. From 2012 to 2014, we distributed the parent-administered questionnaire to 25,198 children in all 233 public schools in the 13 municipalities of Miyagi Prefecture in northeast Japan. A total of 7,155 responses (mean age 10.5 ± 2.2 years) were received (response rate: 28.4%). The prevalence of allergic symptoms according to the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire in 2nd, 4th, 6th, and 8th graders was 12.4%, 9.9%, 9.3%, and 5.6% for wheeze, and 20.1%, 18.0%, 14.0%, and 12.4% for eczema. In multivariate logistic analysis, younger age, history of hospitalization, and difficulties in children’s daily lives as assessed by the Strengths and Difficulties Questionnaire (SDQ), were significantly and consistently associated with both allergic symptoms (both P < 0.05). Living in a coastal municipality was also associated with eczema symptoms (P = 0.0278). The prevalence of eczema symptoms in the 2nd (20.1%) and 8th (12.4%) grades was significantly higher than previously reported in Japan. Living in a coastal municipality was independently associated with eczema symptoms, and psychometric properties were also closely linked to allergic symptoms. These findings are clinically important for understanding the risks of allergic disorders after natural disasters.
Introduction
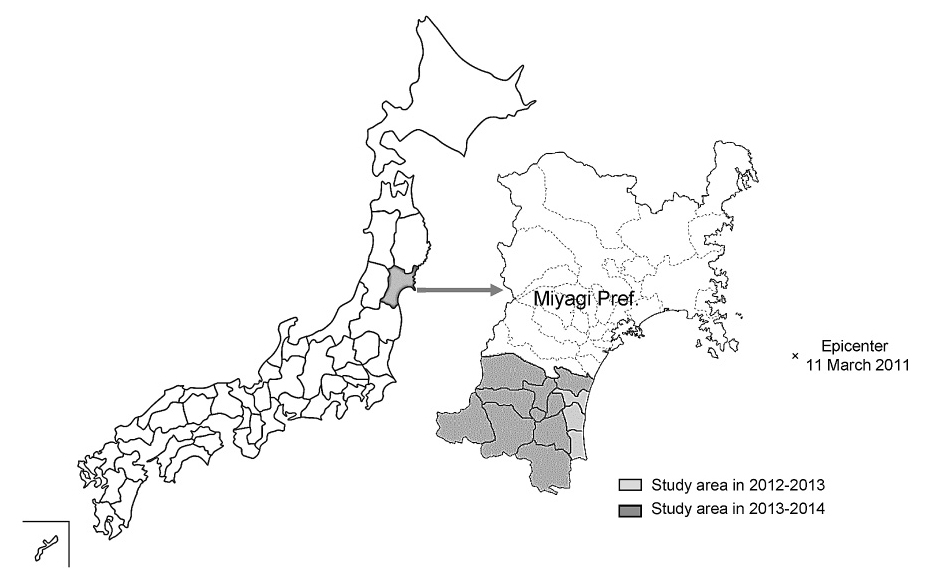
The Great East Japan Earthquake of 2011 was a combination disaster comprising both a massive earthquake and a tsunami, and caused serious damage in northeast Japan. Miyagi Prefecture, which is located in northeast Japan, was particularly affected by the disaster, due in large part to its relative proximity to the epicenter (see Fig. 1). Among all 47 prefectures in Japan, Miyagi had the highest number of victims (9,539 dead, 1,244 missing) (National Police Agency of Japan 2015). It took more than a month after the disaster to restore lifelines along the coast of Miyagi Prefecture, and during this time, residents were unable to carry out many activities of daily living such as taking a bath. Accompanying such conditions was a concern for potential health problems among high risk populations, particularly children. Regarding potential health problems in children, allergic diseases were the major concern.
Several studies focusing on allergic diseases after natural disasters, including bronchial asthma (Takakura et al. 1997; Tomita et al. 2005; Suzuki et al. 2007; Madhok et al. 2015) and atopic dermatitis (Kodama et al. 1999) after earthquakes, have been reported. In addition, studies after combination disasters involving both an earthquake and a tsunami have also been reported; these include skin problems such as eczema after the 2004 Sumatra earthquake (Lee et al. 2006) and control of asthma after the 2011 Great East Japan Earthquake (Yamaoka et al. 2011; Fukuhara et al. 2012; Minoura et al. 2012; Yanagimoto et al. 2012; Ishiura et al. 2013; Ohkouchi et al. 2013). Although those studies were highly valuable, the generalizability of their results was limited as they relied primarily on data from patients; data from individuals who did not visit a clinic or medical institution remained hidden. In addition, these reports implemented “original” as opposed to international standardized questionnaires, which created potential difficulties in interpreting the results and comparing them with those from previous studies (Ueda et al. 1996; Takakura et al. 1997; Kodama et al. 1999; Tomita et al. 2005; Lee et al. 2006). Furthermore, those studies focused mainly on adults as opposed to children. Few studies on wheeze and eczema symptoms among schoolchildren after a natural disaster have been conducted.
Therefore, we conducted a large-scale cross-sectional study of health among schoolchildren using a standardized epidemiological questionnaire, the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire, to examine the prevalence of wheeze and eczema symptoms and associated factors among schoolchildren in disaster-affected areas (Kikuya et al. 2015).
Methods
Design
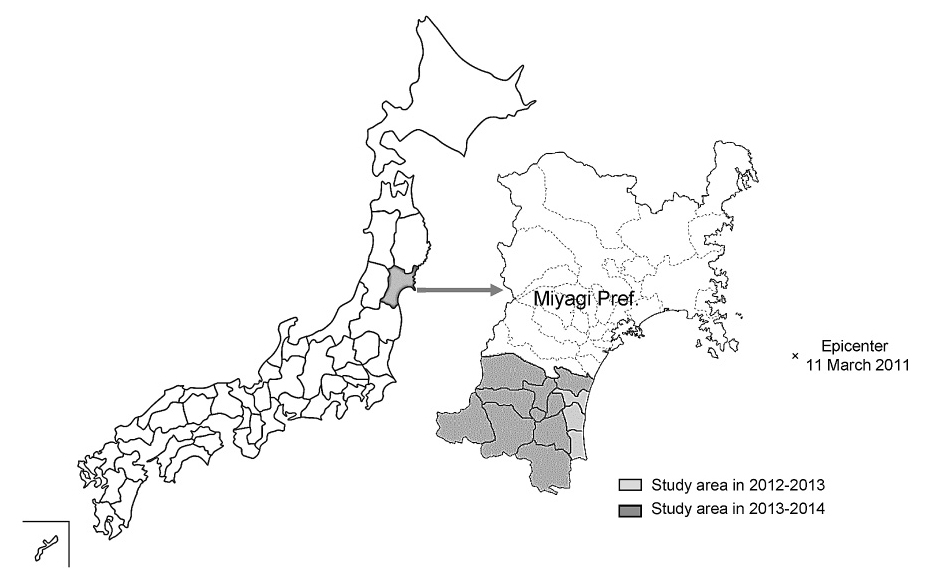
This report was based on an ongoing study project, the Tohoku Medical Megabank Organization (ToMMo) Child Health Study, which was a cross-sectional observation of schoolchildren in 28 municipalities of Miyagi Prefecture after the 2011 Great East Japan Earthquake. Details of the study project have been described previously (Kikuya et al. 2015). Although data collection had been completed in all 28 municipalities, at the time of preparing this manuscript, data were only available for the following 13: Shiroishi, Natori, Kakuda, Iwanuma, Zao, Shichikashuku, Ogawara, Murata, Shibata, Kawasaki, Marumori, Watari, and Yamamoto. Among these municipalities, Natori, Iwanuma, Watari, and Yamamoto are located in coastal areas (Fig. 1). Therefore, only data from schoolchildren in these 13 municipalities were analyzed.
In each municipality, due to insufficient human resources and annual research budget limitations, the questionnaire survey was divided into two consecutive years. In the first year, we examined children in the 2nd, 4th, 6th, and 8th grades, and in the second year, we examined those in the 1st, 3rd, 5th, and 7th grades. Since students progressed to the next grade the following year, the 2nd-, 4th-, 6th-, and 8th-grade students were examined at that time. In 2012, the survey was started in the three coastal municipalities of Iwanuma, Watari, and Yamamoto (Survey 2012) (Fig. 1). Then, in 2013, the study area was extended to all 13 municipalities, including the three municipalities from the previous survey (Survey 2013). These same municipalities, excluding Iwanuma, Watari, and Yamamoto, were also included in the study area in Survey 2014 because the survey was performed in two consecutive years in each municipality, as described above. Ethical approval was obtained from the Institutional Review Board of Tohoku University Graduate School of Medicine on September 24, 2012 (No. 2012-1-278). Completing and returning a questionnaire was considered to indicate consent to participate in our investigation.
Since elementary and junior high school education is compulsory in Japan, almost all children in Miyagi Prefecture were affiliated with a school, typically (about 99.7%) with a public school, according to the Miyagi Office of Education. There are 233 public schools in the 13 municipalities of Miyagi Prefecture. The 233 schools included 147 elementary, 76 junior high, and 10 special needs schools. One elementary school that participated in Survey 2013 withdrew from Survey 2014.
There were 3,505 schoolchildren in 26 public schools in the three municipalities in Survey 2012, 12,742 schoolchildren in 117 public schools in the 13 municipalities in Survey 2013, and 9,225 schoolchildren in 90 public schools in the 10 municipalities in Survey 2014. After excluding one elementary school from Survey 2014, in cooperation with the Board of Education of each municipality and the 233 public schools, the questionnaire was finally distributed to 25,198 children. The questionnaires were distributed in June every year except for 2012, in which questionnaires were distributed in November. The children took the questionnaires home for their parents or guardians to complete within two weeks; 1,369 (39.1%), 4,080 (32.0%), and 2,266 (25.3%) questionnaires were returned for Survey 2012, Survey 2013, and Survey 2014, respectively, for a total of 7,715 (collection rate: 30.6%). Grade-specific response rates were 32.9%, 31.7%, 28.1%, and 21.5% in 2nd, 4th, 6th, and 8th grade, respectively.
We excluded 560 questionnaires due to the following reasons: missing age data (N = 62); responses for children outside the target grades (N = 134); and missing responses for asthma symptoms (N = 94), eczema symptoms (N = 62), and the Strengths and Difficulties Questionnaire (SDQ, reference) (N = 208). Therefore, a total of 7,155 (28.4%) children were included in the present analysis. Among all children, there was no duplicate participant, a so-called “repeater,” who was held back for another year. In the Japanese elementary and junior high school system, “repeaters” are extremely rare. Furthermore, in each municipality, we only surveyed for two consecutive years. Thus, no participant other than the repeater answered the questionnaire twice.
Questionnaire items
To assess symptoms of asthma and eczema, we adopted the Japanese version of the ISAAC questionnaire (Nishima and Odajima 2002), which is an international standardized epidemiological questionnaire used to assess allergic symptoms. Current wheeze was defined as a positive response to the item “Has your child had wheezing or whistling in the chest in the last 12 months?” (Lai et al. 2009). Severe wheeze was defined as current wheeze with ≥ 4 attacks, or ≥ 1 night per week of sleep disturbance from wheeze, or wheeze affecting speech (Lai et al. 2009). Current eczema was defined as a positive response to the items “Has your child had this itchy rash at any time during the past 12 months?” and “Has this itchy rash at any time affected any of the following places: the folds of the elbows, behind the knees, in front of the ankles, under the buttocks, or around the neck, ears, or eyes?” (Odhiambo et al. 2009). Severe eczema was defined as current eczema accompanied by sleep disturbance ≥ 1 night per week (Odhiambo et al. 2009). In addition, to assess the extent of symptoms, we asked about any previous diagnosis of these allergic diseases.
The questionnaire also included items on birth year, birth month, person filling out the questionnaire (mother, father, grandparent, or other), history of hospitalization, history of being diagnosed with an allergic disease, the Japanese language version of the SDQ questionnaire (Matsuishi et al. 2008), and disaster experience. History of hospitalization was defined as hospitalization for any reason, including wheeze, eczema, or other diseases or symptoms. The SDQ is a brief questionnaire composed of 25 items designed to investigate difficulties in the daily and social lives of children (Goodman 1997). An SDQ total difficulties score of 16 points or more was considered to be in the abnormal or “clinical” range (Matsuishi et al. 2008). The questionnaire item regarding disaster experience was “At the time of the disaster, please choose all that your child experienced”, with the choices provided as: “earthquake”, “tsunami”, “both”, or “none”.
We also asked about children’s housing in Survey 2013 and Survey 2014, as “In which type of dwelling do you and your child currently live?”, with the choices provided as follows: 1) prefabricated temporary housing; 2) private rental housing under a designated leasing system for people affected by the disaster; 3) rental housing not under a designated leasing system for people affected by the disaster; 4) home of family, friends, or relatives; 5) housing rebuilt at the same location as before the disaster; 6) housing rebuilt at a new location; 7) same housing as that before the disaster; and 8) other.
Data analysis
For descriptive statistics, we calculated the frequency of asthma and eczema symptoms. To assess factors associated with these symptoms, we performed multiple logistic regression analysis with adjustment for sex (boy = 1, girl = 0), age (continuous variable, 1 year increments), history of hospitalization (yes = 1, no = 0), clinical range on the SDQ (yes = 1, no = 0), coastal municipality (yes = 1, no = 0), tsunami experience (yes = 1, no = 0), and survey year (Survey 2013 or Survey 2014 vs. Survey 2012 as a reference). The variable “coastal municipality” was defined by location of the public school affiliation of the children. If the school was located in a coastal municipality, i.e., Natori, Iwanuma, Watari, or Yamamoto, “coastal municipality” was coded as “yes”.
We then compared means and proportions using the unpaired t-test or analysis of variance, Fisher’s exact test, and the chi-square test. P values less than 0.05 were considered to be statistically significant. All statistical analyses were performed using SAS (version 9.4; SAS Institute Inc., Cary, NC, USA).
Results
Among the 7,155 completed and returned questionnaires, the person who filled out the questionnaire was most frequently the mother (N = 6,527, 91.2%), followed by the father (N = 545, 7.6%), a grandparent (N = 72, 1.0%), and other (N = 11, 0.2%). Almost all children (N = 7,071, 98.8%) had experienced an earthquake. Among the children, 1,443 (20.2%) and 1,275 (17.8%) had received a diagnosis of wheeze or eczema, respectively.
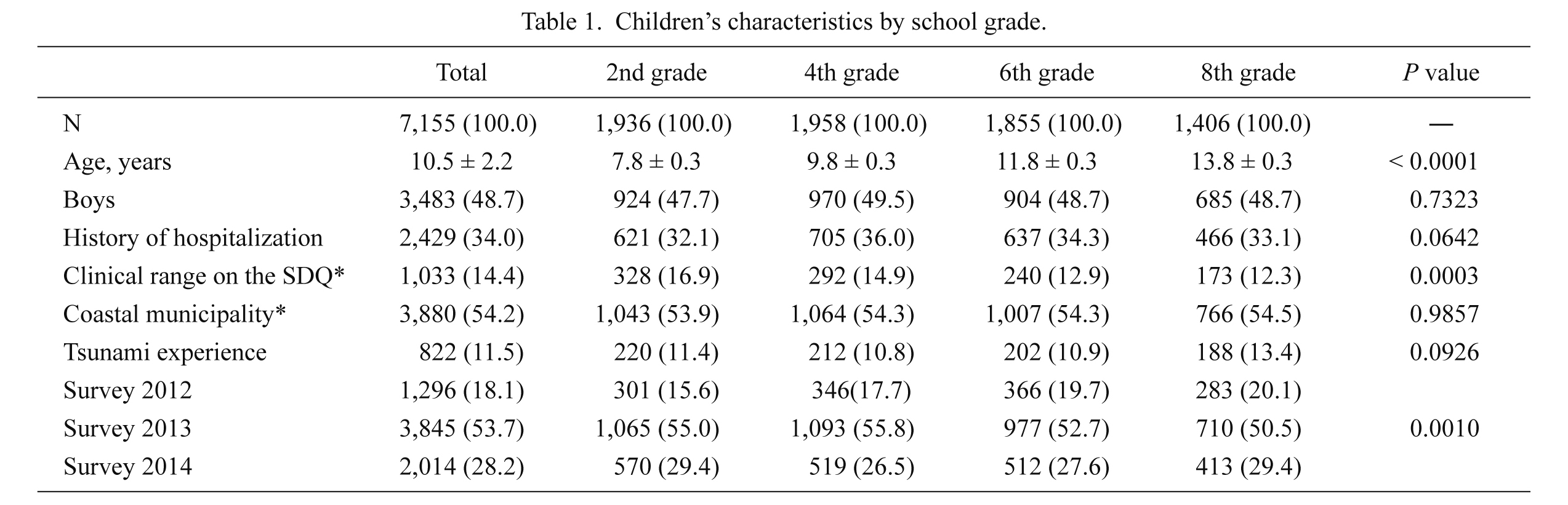
The demographic characteristics of the 7,155 children (boys: 3,483 [48.7%]) are shown in Table 1. The mean age ± standard deviation of the children was 10.5 ± 2.2. A total of 2,429 (34.0%) children had a history of hospitalization. Almost half the children (N = 3,880, 54.2%) were affiliated with a public school located in the municipalities along the coast. A total of 1,033 (14.4%) children had an SDQ total difficulties score in the clinical range (16 points or more). A total of 822 (11.5%) children had experienced a tsunami. The prevalence of these variables was similar between grades. Total numbers of 1,296 (18.1%), 3,845 (53.7%), and 2,014 (28.2%) children participated in Survey 2012, Survey 2013, and Survey 2014, respectively. Tsunami experience was more prevalent, but SDQ scores in the clinical range and history of hospitalization were less prevalent, in coastal than in inland municipalities (all P < 0.01).
Factors affecting wheeze and eczema
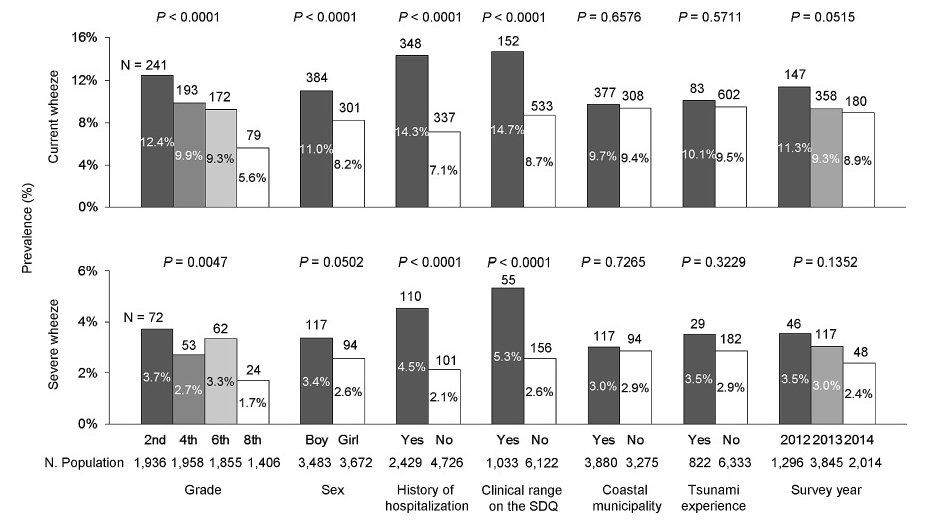
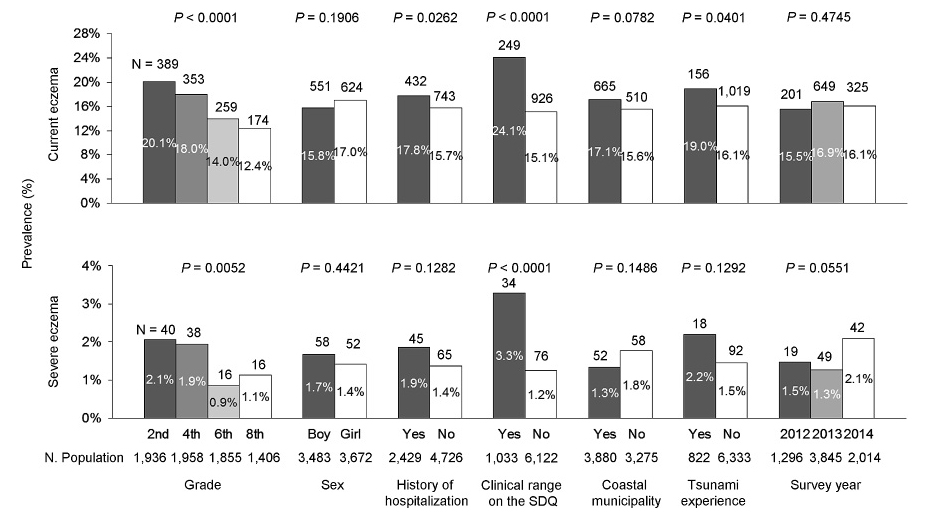
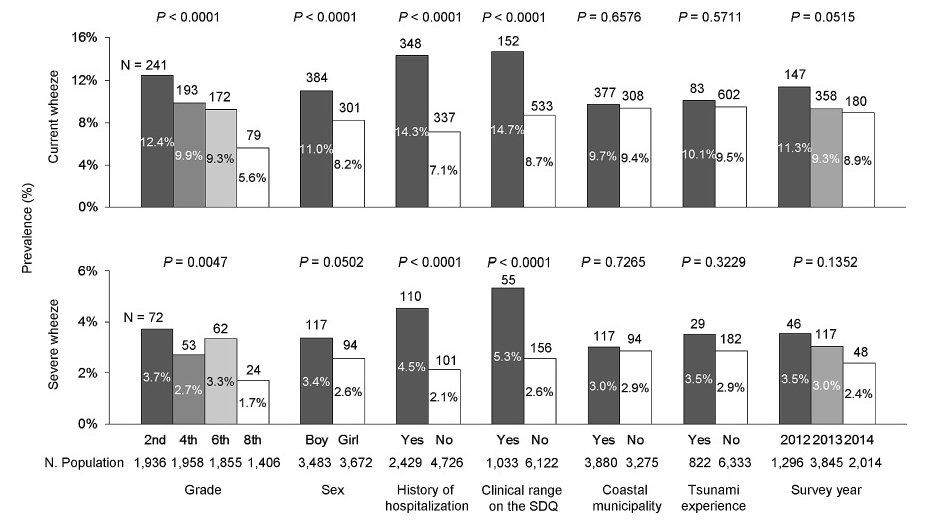
To investigate factors affecting current and severe wheeze, we conducted univariate analysis of the prevalence of these symptoms (Fig. 2). Boys, students with a history of hospitalization, students in lower grades, and students with SDQ scores in the clinical range had a significantly high prevalence of current wheeze (P < 0.0001). Results from Survey 2012, which was the survey conducted in the timeframe nearest to the disaster, also tended to be associated with a high prevalence of current wheeze (P = 0.0515); similar findings were observed for severe wheeze. Univariate analysis of current and severe eczema is shown in Fig. 3. A significantly high prevalence of current eczema was observed in children in lower grades, those with a history of hospitalization, those with SDQ scores in the clinical range, and those with previous tsunami experience. Although weaker associations were observed for severe eczema, those for lower grade and clinical range on the SDQ were still significant.
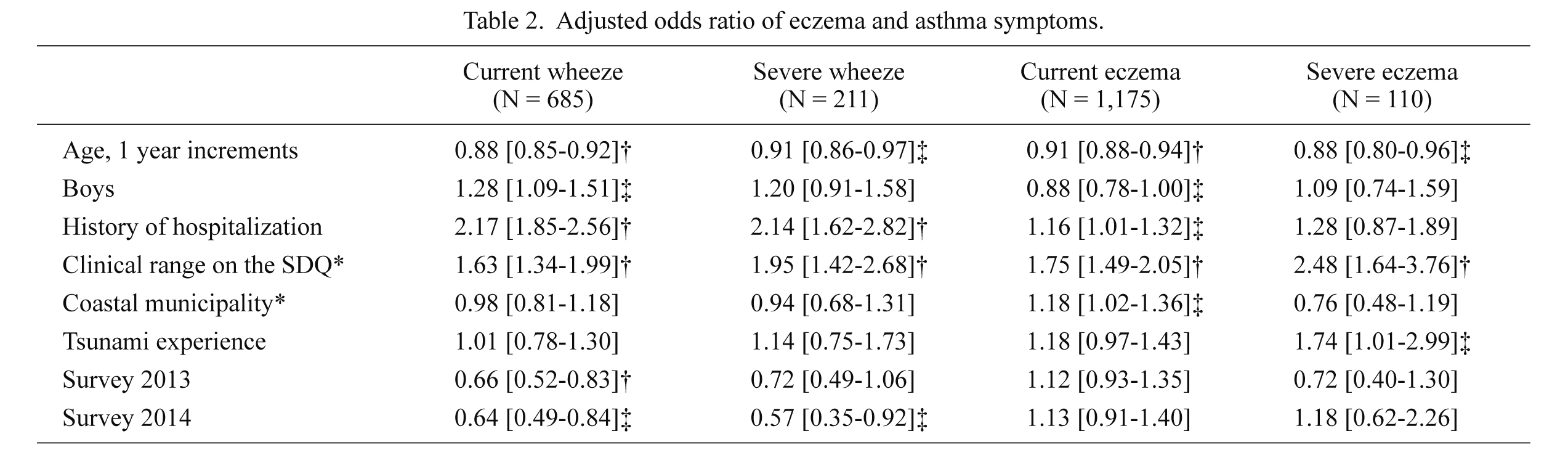
Multivariate logistic regression analysis was conducted to investigate the association of these variables with the allergic symptoms of current and severe wheeze, and current and severe eczema (Table 2). Younger age, history of hospitalization, and clinical range on the SDQ were significantly and consistently associated with all allergic symptoms (P < 0.05), with the exception of history of hospitalization and severe eczema (odds ratio [OR]: 1.28, P = 0.2). The association between sex and allergy was not uniform. Boys had significantly high ORs for current wheeze (OR: 1.28, P = 0.0025), but low ORs for current eczema (OR: 0.88, P = 0.0487). Regarding associations with allergic symptoms, no significant interaction was found between tsunami experience and coastal municipality (P > 0.1); however, coastal municipality was associated with current eczema (OR: 1.18, P = 0.0278), while tsunami experience was associated with severe eczema (OR: 1.74, P = 0.0467). Recent survey years, particularly Survey 2014, were inversely associated with wheeze symptoms when Survey 2012 was treated as the reference category (OR: ≤ 0.66, P ≤ 0.0013).
The questionnaires for Survey 2013 and 2014 contained items on the current living environment of parents/guardians and their children. After excluding children from Survey 2012 (N = 1,296) and missing responses for this item (N = 24), 5,835 responses were analyzed. The results were as follows: (1) prefabricated temporary housing (N = 64, 1.1%); (2) private rental housing under a designated leasing system for people affected by the disaster (N = 191, 3.2%); (3) rental housing not under a designated leasing system for people affected by the disaster (N = 131, 2.5%); (4) home of family, friends, or relatives (N = 166, 2.8%); (5) housing rebuilt at the same location as before the disaster (N = 74, 1.3%); (6) housing rebuilt at a new location (N = 316, 5.4%); (7) same housing as that before the disaster (N = 4,695, 80.5%); and (8) other (N = 198, 3.4%). With the exception of living in prefabricated temporary housing, a type of housing only found in coastal municipalities, no clear tendency was evident regarding living environment (coastal vs. inland municipality). In coastal municipalities, the prevalence of wheeze was significantly higher among schoolchildren living in housing rebuilt at the same location as before the disaster than those in the other living environments (23.1% [N = 9] vs. 8.7% [N = 221]; P = 0.0017). The prevalence of eczema was significantly higher among children living in rental housing not under a designated leasing system for people affected by the disaster than among those in the other living environments (28.3% [N = 17] vs. 17.7% [N = 447]; P = 0.0341). On the other hand, in inland municipalities, the prevalence of wheeze was significantly higher among schoolchildren living in rental housing not under a designated leasing system for people affected by the disaster (16.9% [N = 12] vs. 9.2% [N = 296], P = 0.0287), home of family, friends, or relatives (14.9% [N = 17] vs. 9.2% [N = 291], P = 0.0403), and not same housing as that before the disaster than among those in the other living environments (12.1% [N = 71] vs. 8.8% [N = 237]; P = 0.0125). No other associations were observed between allergic symptoms and the remaining response alternatives for current living environment.
Discussion
We investigated the prevalence of allergic symptoms and associated factors among 7,155 schoolchildren in areas affected by the Great East Japan Earthquake. The prevalence of wheeze in the 12 months prior to study in 2nd, 4th, 6th, and 8th graders was 12.4%, 9.9%, 9.3%, and 5.6%, respectively, and the prevalence of eczema, defined as an itchy flexural rash, during the same period was 20.1%, 18.0%, 14.0%, and 12.4%, respectively. The ORs of wheeze symptoms were higher in younger children, boys, those with a history of hospitalization, and those with SDQ scores in the clinical range, and were lower in children in the most recent surveys (Surveys 2013 and 2014). Regarding ORs for eczema, younger age, girls, a history of hospitalization, SDQ scores in the clinical range, and coastal municipality were shown to be significant factors. An association was also seen between tsunami experience and severe eczema.
As shown in Table 1, the ratio of boys to girls in each grade was almost identical, as was the sex distribution in each grade; this suggests the absence of any sex or age bias in terms of the distribution of the questionnaires, as well as the representativeness of our study subjects. However, 8th graders participated in the study to a lesser extent compared with the other students. This finding was also reported in our previous study (Kikuya et al. 2015). This could be due to parents or guardians of students in the upper grades being less motivated to participate in health research after a disaster than parents of students in the lower grades.
The relationship observed between prevalence of allergic symptoms and both sex and age was consistent with previous findings (Williams et al. 1999; Futamura et al. 2011), i.e., allergic symptoms were more frequent in younger students. Of note, in the present study, the associations between sex and allergic symptoms for wheeze and eczema differed. In line with previous studies (Futamura et al. 2011), boys had high ORs for current wheeze. On the other hand, the OR of 0.88 (95% confidence interval [CI]: 0.78-1.00) for current eczema was marginally significantly low in boys; in other words, current eczema was associated with girls. This result is also in line with previous findings. Williams et al. (1999) reported that the prevalence of eczema in girls was high; however, inconsistencies have been reported in the prevalence of eczema according to sex. However, Futamura et al. (2011) reported finding the opposite result, that the prevalence of eczema was similar in both sexes (Futamura et al. 2011).
To evaluate the effect of disasters on wheeze, we investigated the prevalence of allergic symptoms in the present study. There have been several reports on the prevalence of allergic symptoms in the general population based on the ISAAC questionnaire (ISAAC Steering Committee 1998a; Williams et al. 1999, 2008; Futamura et al. 2011). These reports focused mainly on 2nd and 8th graders because the ISAAC manual defines these students as the target population. In these reports, the prevalence of current wheeze ranged from 15.7% to 17.3% for 2nd graders and from 8.8% to 13.4% for 8th graders in Japan (Nishima and Odajima 2002; Akashi and Akasawa 2007; Futamura et al. 2011). Compared with these previous studies, the prevalence of current wheeze was significantly low (both P < 0.001) among both 2nd (12.4%) and 8th (5.6%) graders. Furthermore, no association was seen between asthma symptoms and disaster-related variables such as tsunami experience and affiliated school in a coastal municipality. However, associations were observed between wheeze symptoms and both rental housing not under a designated leasing system for people affected by the disaster and home of family, friends, or relatives. Based on these results, no association was found between wheeze and disaster-related damage in the population as a whole. However, wheeze symptoms were found to be associated with severely affected children who were forced to change their living environment. Therefore, special consideration should be paid to wheeze symptoms in children whose living environments are drastically affected by a disaster.
The prevalence of eczema in Japanese children has previously been reported to range from 16.0% to 17.4% in 2nd graders and from 9.8% to 10.7% in 8th graders (Williams et al. 1999; Nishima and Odajima 2002; Akashi and Akasawa 2007; Futamura et al. 2011). Compared with previous studies, we observed a significantly higher prevalence of eczema among 2nd (20.1%) and 8th (12.4%) graders (both P < 0.05). Furthermore, disaster-related variables such as coastal area, tsunami experience, and changes in living environment were associated with eczema symptoms. Specifically, the prevalence of eczema was higher in coastal than in inland areas (OR: 1.18; 95%CI: 1.02-1.36). Tsunami experience was also significantly related to severe eczema (OR: 1.74; 95%CI: 1.01-2.99). Based on these results, in relation to eczema, the effect of disasters on the prevalence of eczema in the population as a whole, as well as in children with tsunami experience, cannot be excluded. After the earthquake in Sumatra in 2004, eczema was reportedly the second most prevalent symptom among dermatology patients (Lee et al. 2006). After the Great East Japan Earthquake, wheeze and eczema were found in 22% and 55%, respectively, of children with food allergies (Yamaoka et al. 2011). These results suggest that disasters have a long-term effect on allergic symptoms.
Psychological or psychiatric conditions are closely related to allergic symptoms. Mental stress exacerbates symptoms of allergic disease (Ueda et al. 1996; Kodama et al. 1999; Buske-Kirschbaum et al. 2002; Rosenberg et al. 2014). In line with previous studies, our results demonstrated that SDQ scores in the clinical range was also significantly and consistently related to all allergic symptoms of current wheeze, severe wheeze, current eczema and severe eczema (Table 2), and the size of the effect was considerable, with ORs for these allergic symptoms ranging from 1.63 to 2.48. Due to the cross-sectional design of our study, a cause-effect relationship between psychological or psychiatric conditions and allergic symptoms could not be determined. Reverse causality could also explain these results. Allergic symptoms could potentially affect SDQ total scores, because the SDQ is a scale not only of psychological or psychiatric conditions, but also of difficulties in daily life. It is also possible that psychological and psychiatric conditions mediated the association between the disaster and allergic symptoms. Psychological and psychiatric conditions in children after disasters have been reported in several studies (McLaughlin et al. 2010; Fujiwara et al. 2014). Serious emotional disturbances remained significantly elevated for several years after Hurricane Katrina struck the United States in 2005 (McLaughlin et al. 2010). Even two years after the Great East Japan Earthquake, severe trauma related to the disaster was shown to be associated with behavior problems (Fujiwara et al. 2014). However, the specific or inherent mental problems of each children and their family that are not attributable to disasters, such as child abuse, developmental disabilities, or other disorders, should also be considered.
In general, asthma and eczema follow the “allergic march”, which means that various symptoms develop in patients as they age; therefore, they cannot be considered separately. However, in this study, only the prevalence of eczema was high; that of asthma in the population as a whole was not. This result indicated that eczema could be associated with specific factors (ISAAC Steering Committee 1998b). Several factors, including immunity, heredity, maternal problems, environment, and psychological stress, have been associated with the development or presence of eczema (Levy et al. 2003, Rosenberg et al. 2014). Further studies are required, not only to monitor the prevalence of eczema using the ISAAC questionnaire, but also to measure environmental factors in detail with the aim of clarifying the causal link between disasters and the prevalence of eczema.
Our study did have several limitations. First, our results exclusively relied on a parent-administered questionnaire that was composed of subjective data in order to assess symptoms in a large number of subjects with minimal burden to participate in our study. Therefore, our results could differ from those found in studies based on doctor-diagnosed allergic diseases. Second, our findings were not derived from the entire disaster-affected area. Nonetheless, all of the public schools in the study area participated in this research. Third, Survey 2012 was conducted in November, which was different from the June survey period for Survey 2013 and Survey 2014. However, the questionnaire items regarding allergic symptoms were based on observations during the entire previous year (Asher et al. 1995). Therefore, this difference in the study period is not thought to have significantly affected the prevalence of allergic symptoms. Fourth, our study did not begin until after the disaster; therefore, we could not formally compare the prevalence of symptoms in children before and after the disaster. Fifth, in coastal municipalities, the survey was conducted in 2012-2013, but not in 2013-2014 (Fig. 1). This imbalance in study area for each study year could affect the results, even though we adjusted for survey year in our logistic regression model. Sixth, the response rate for the questionnaire was only 28.4%, and differed among the survey years as follows: 39.1% in 2012, 32.0% in 2013, and 25.3% in 2014. However, no differences in age or sex were found among survey years (P > 0.5). Furthermore, although we adjusted for survey year in multiple logistic analyses, our results may have been affected by self-selection bias.
In conclusion, after the disaster, the prevalence of eczema symptoms among 2nd and 8th grade students was significantly higher than previously reported. Living in a coastal municipality was independently associated with eczema symptoms, and psychometric properties were also closely linked to allergic symptoms in children. These findings are expected to be clinically important for understanding the risks of allergic disorders after natural disasters.
Acknowledgments
This work was supported by the MEXT Tohoku Medical Megabank Project. We would like to thank the Miyagi Prefectural Board of Education and the municipal boards of education in Shiroishi, Natori, Kakuda, Iwanuma, Zao, Shichikashuku, Ogawara, Murata, Shibata, Kawasaki, Marumori, Watari, and Yamamoto for participating in the study. We would also like to thank the expert psychologists, Tomoko Kitada, Kotomi Shingu, and Tomoka Shoji, for individual interviews and telephone support, Shoji Tanaka for technical assistance, and Chiaki Abe for clerical work.
Conflict of Interest
The authors declare no conflict of interest.
References
-
Akashi,
M. &
Akasawa,
A.
(2007) Study about all age rank nation-wide surveys about prevalence / morbidity of bronchial asthma and QOL. Jpn. J. Pediatr. Allergy Clin. Immunol., 21, 743-748.
-
Asher,
M.I.,
Keil,
U.,
Anderson,
H.R.,
Beasley,
R.,
Crane,
J.,
Martinez,
F.,
Mitchell,
E.A.,
Pearce,
N.,
Sibbald,
B.,
Stewart,
A.W.,
Strachan,
D.,
Weiland,
S.K. &
Williams,
H.C.
(1995) International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur. Respir. J., 8, 483-491.
-
Buske-Kirschbaum,
A.,
Gierens,
A.,
Hollig,
H. &
Hellhammer,
D.H.
(2002) Stress-induced immunomodulation is altered in patients with atopic dermatitis. J. Neuroimmunol., 129, 161-167.
-
Fujiwara,
T.,
Yagi,
J.,
Homma,
H.,
Mashiko,
H.,
Nagao,
K. &
Okuyama,
M.;
Great East Japan Earthquake Follow-up for Children Study Team
(2014) Clinically significant behavior problems among young children 2 years after the Great East Japan Earthquake. PLoS One, 9, e109342.
-
Fukuhara,
A.,
Sato,
S.,
Uematsu,
M.,
Misa,
K.,
Nikaido,
T.,
Inokoshi,
Y.,
Fukuhara,
N.,
Wang,
X.,
Kanazawa,
K.,
Tanino,
Y.,
Ishida,
T. &
Munakata,
M.
(2012) Impacts of the 3/11 disaster in fukushima on asthma control. Am. J. Respir. Crit. Care Med., 186, 1309-1310.
-
Futamura,
M.,
Ohya,
Y.,
Akashi,
M.,
Adachi,
Y.,
Odajima,
H.,
Akiyama,
K. &
Akasawa,
A.
(2011) Age-related prevalence of allergic diseases in Tokyo schoolchildren. Allergol. Int., 60, 509-515.
-
Goodman,
R.
(1997) The Strengths and Difficulties Questionnaire: a research note. J. Child Psychol. Psychiatry., 38, 581-586.
-
Ishiura,
Y.,
Fujimura,
M.,
Yamamoto,
H.,
Shiba,
Y.,
Ohkura,
N.,
Kasahara,
K. &
Ishida,
Y.
(2013) Asthma exacerbations after the East Japan Disaster. J. Med. Invest., 60, 61-65.
-
Kikuya,
M.,
Miyashita,
M.,
Yamanaka,
C.,
Ishikuro,
M.,
Sato,
Y.,
Obara,
T.,
Metoki,
H.,
Nakaya,
N.,
Nagami,
F.,
Tomita,
H.,
Kiyomoto,
H.,
Sugawara,
J.,
Hozawa,
A.,
Fuse,
N.,
Suzuki,
Y., et al.
(2015) Protocol and Research Perspectives of the ToMMo Child Health Study after the 2011 Great East Japan Earthquake. Tohoku J. Exp. Med., 236, 123-130.
-
Kodama,
A.,
Horikawa,
T.,
Suzuki,
T.,
Ajiki,
W.,
Takashima,
T.,
Harada,
S. &
Ichihashi,
M.
(1999) Effect of stress on atopic dermatitis: investigation in patients after the great hanshin earthquake. J. Allergy Clin. Immunol., 104, 173-176.
-
Lai,
C.K.,
Beasley,
R.,
Crane,
J.,
Foliaki,
S.,
Shah,
J. &
Weiland,
S.;
the ISAAC Phase Three Study Group
(2009) Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax, 64, 476-483.
-
Lee,
S.H.,
Choi,
C.P.,
Eun,
H.C. &
Kwon,
O.S.
(2006) Skin problems after a tsunami. J. Eur. Acad. Dermatol. Venereol., 20, 860-863.
-
Levy,
R.M.,
Gelfand,
J.M. &
Yan,
A.C.
(2003) The epidemiology of atopic dermatitis. Clin. Dermatol., 21, 109-115.
-
Madhok,
V.,
Futamura,
M.,
Thomas,
K.S. &
Barbarot,
S.
(2015) What’s new in atopic eczema? An analysis of systema reviews published in 2012 and 2013. Part 1. Epidemiology, mechanisms of disease and methodological issues. Clin. Exp. Dermatol., 40, 238-242.
-
Matsuishi,
T.,
Nagano,
M.,
Araki,
Y.,
Tanaka,
Y.,
Iwasaki,
M.,
Yamashita,
Y.,
Nagamitsu,
S.,
Iizuka,
C.,
Ohya,
T.,
Shibuya,
K.,
Hara,
M.,
Matsuda,
K.,
Tsuda,
A. &
Kakuma,
T.
(2008) Scale properties of the Japanese version of the Strengths and Difficulties Questionnaire (SDQ): a study of infant and school children in community samples. Brain Dev., 30, 410-415.
-
McLaughlin,
K.A.,
Fairbank,
J.A.,
Gruber,
M.J.,
Jones,
R.T.,
Osofsky,
J.D.,
Pfefferbaum,
B.,
Sampson,
N.A. &
Kessler,
R.C.
(2010) Trends in serious emotional disturbance among youths exposed to Hurricane Katrina. J. Am. Acad. Child Adolesc. Psychiatry., 49, 990-1000.
-
Minoura,
T.,
Yanagida,
N.,
Watanabe,
Y.,
Yamaoka,
A. &
Miura,
K.
(2012) The effects of great East Japan earthquake on patients with food allergy in Miyagi Prefecture. Arerugi, 61, 642-651 (in Japanese, abstract in English).
-
National Police Agency of Japan
(2015) Damage Situation and Police Countermeasures associated with 2011 Tohoku district-off the Pacific Ocean Earthquake. https://www.npa.go.jp/archive/keibi/biki/higaijokyo_e.pdf [Accessed: July 13, 2015].
-
Nishima,
S. &
Odajima,
H.
(2002) Prevalence of childhood allergoc diseases in Japan using International Study of Asthma and Allergies in Childhood (ISAAC) Phase I protocol. Jpn. J. Pediatr. Allergy Clin. Immunol., 16, 207-220 (in Japanese, abstract in English).
-
Odhiambo,
J.A.,
Williams,
H.C.,
Clayton,
T.O.,
Robertson,
C.F. &
Asher,
M.I.;
ISAAC Phase Three Study Group
(2009) Global variations in prevalence of eczema symptoms in children from ISAAC Phase Three. J. Allergy Clin. Immunol., 124, 1251-1258.
-
Ohkouchi,
S.,
Shibuya,
R.,
Yanai,
M.,
Kikuchi,
Y.,
Ichinose,
M. &
Nukiwa,
T.
(2013) Deterioration in regional health status after the acute phase of a great disaster: respiratory physicians’ experiences of the Great East Japan Earthquake. Respir. Investig., 51, 50-55.
-
Rosenberg,
S.L.,
Miller,
G.E.,
Brehm,
J.M. &
Celedon,
J.C.
(2014) Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J. Allergy Clin. Immunol., 134, 1009-1015.
-
Suzuki,
K.,
Hasegawa,
T.,
Iguchi,
S.,
Ota,
K.,
Sakagami,
T.,
Gejyo,
F. &
Suzuki,
E.
(2007) The impact of the Chuetsu earthquake on asthma control. Allergol. Int., 56, 179.
-
Takakura,
R.,
Himeno,
S.,
Kanayama,
Y.,
Sonoda,
T.,
Kiriyama,
K.,
Furubayashi,
T.,
Yabu,
M.,
Yoshida,
S.,
Nagasawa,
Y.,
Inoue,
S. &
Iwao,
N.
(1997) Follow-up after the Hanshin-Awaji earthquake: diverse influences on pneumonia, bronchial asthma, peptic ulcer and diabetes mellitus. Intern. Med., 36, 87-91.
-
The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee
(1998a) Worldwide variations in the prevalence of asthma symptoms: the International Study of Asthma and Allergies in Childhood (ISAAC). Eur. Respir. J., 12, 315-335.
-
The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee
(1998b) Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet, 351, 1225-1232.
-
Tomita,
K.,
Hasegawa,
Y.,
Watanabe,
M.,
Sano,
H.,
Hitsuda,
Y. &
Shimizu,
E.
(2005) The Tottori-Ken Seibu earthquake and exacerbation of asthma in adults. J. Med. Invest., 52, 80-84.
-
Ueda,
K.,
Tsuda,
K.,
Nakano,
H. &
Saigo,
K.
(1996) Asthmatic attacks in the Great Hanshin Earthquake: analysis of behavioral and environmental factors. Kokyu, 15, 1178-1183 (in Japanese).
-
Williams,
H.,
Robertson,
C.,
Stewart,
A.,
Ait-Khaled,
N.,
Anabwani,
G.,
Anderson,
R.,
Asher,
I.,
Beasley,
R.,
Björkstén,
B.,
Burr,
M.,
Clayton,
T.,
Crane,
J.,
Ellwood,
P.,
Keil,
U.,
Lai,
C., et al.
(1999) Worldwide variations in the prevalence of symptoms of atopic eczema in the International Study of Asthma and Allergies in Childhood. J. Allergy Clin. Immunol., 103, 125-138.
-
Williams,
H.,
Stewart,
A.,
von Mutius,
E.,
Cookson,
W. &
Anderson,
H.R.;
International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Groups
(2008) Is eczema really on the increase worldwide? J. Allergy Clin. Immunol., 121, 947-954.
-
Yamaoka,
A.,
Abe,
H.,
Watanabe,
Y.,
Kakuta,
H.,
Umebayashi,
H.,
Inagaki,
T.,
Abukawa,
D.,
Yanagida,
N.,
Minoura,
T.,
Morikawa,
M.,
Kondo,
N. &
Miura,
K.
(2011) The Questionnaire for caregivers of allergic children in the Great East Japan Earthquake. Jpn. J. Pediatr. Allergy Clin. Immunol., 25, 801-809 (in Japanese, abstract in English).
-
Yanagimoto,
S.,
Haida,
M. &
Suko,
M.
(2012) An asthma patient with steroid-resistant decrease in peak expiratory flow after the Great East Japan earthquake showing spontaneous recovery after 1 month. Intern. Med., 51, 1631-1634.