Abstract
Patients with systemic sclerosis (SSc) often display Raynaud’s phenomenon and digital skin ulcers. As these ulcers are not associated with autoimmune factors or abnormal coagulation, conventional immunosuppressive therapies, vasodilators, and anticoagulants are often ineffective. Here, we used extracorporeal shock wave therapy (ESWT) to treat these ulcers. Nine SSc patients with new digital ulcers, previously treated with at least one currently available vasodilator or anticoagulant were enrolled. One ESWT session consisted of 100 pulses at 0.08-0.25 mJ/mm2 in 20 areas on both hands and 15 areas on both feet, totaling 7,000 pulses. Treatment was performed once per week for 9 weeks with observations over 20 weeks. Outcomes were evaluated according to the number and diameter of ulcers, Rodnan skin score, Health Assessment Questionnaire (HAQ), EuroQol 5 dimensions (EQ-5D), visual analog scale for pain, and the PainVision system. The surface skin temperature of all the fingers was measured using thermography. Ulcers showed signs of healing after one session, and their mean number decreased from 5.4 to 1.1 at 9 weeks. In particular, of the 18 large ulcers (> 5 mm) observed in 7 patients before the treatment, 10 disappeared and the rest became smaller; namely, the mean size decreased from 10.9 mm to 2.5 mm at 20 weeks. The average scores on the HAQ, EQ-5D, and PainVision system also improved. Treatment was minimally invasive and could be repeated without any adverse effects. ESWT may be added to standard treatments for indolent digital ulcers of SSc, as an effective and safe method.
Introduction
Systemic sclerosis (SSc) is an autoimmune disease characterized by excessive deposition of collagen in the skin and visceral organs as well as vascular damage, including Raynaud’s phenomenon and digital ulcers. Digital ulcers are common and occasionally disabling manifestation of SSc, which develop due to a narrowing and occlusion of the digital arteries and arterioles. Digital ulcers occur within 4 years of diagnosis in 65% of patients with SSc (Poole et al. 2004). In some patients, particularly those with limited cutaneous SSc, digital ulcers represent the primary functional limitation. In some cases, infection may occur and lead to substantial loss of tissue. Over a period of years, the healing of ulcers leads to residual scarring and progressive digital shortening (Poole et al. 2004). The pathogenesis of this condition is complex; the pivotal steps are endothelial cell damage, immune activation, and collagen production by fibroblasts (Abraham and Varga 2005). Endothelial involvement is associated with an increase in some circulating markers, including vascular endothelial growth factor (VEGF) (Cerinic et al. 2003; Carvalho et al. 2007). Treatment of SSc is generally ineffective because it is impossible to modify the course of the disease, especially with regard to the effects of Raynaud’s phenomenon and stenosis of the peripheral arteries, which ultimately results in digital ulcers. As such ulcers are not caused by autoimmune factors or abnormal coagulation, immunosuppressive therapies and anticoagulants have shown little effect (Denton and Black 2005).
Extracorporeal shock wave therapy (ESWT) is defined as a sequence of sonic pulses characterized by high peak pressure (up to 100 MPa), fast pressure increase (10-100 ns), and short lifecycle. This technique was first applied in 1980 for treatment of kidney stones. During the last 10 years, it has been found to induce immediate antalgic and anti-inflammatory effects (Ciampa et al. 2005; Mariotto et al. 2005) together with long-term tissue regeneration (Schaden et al. 2007) and an increase in angiogenesis (Aicher et al. 2006; Ito et al. 2009). Recently, Nishida et al. (2004) applied low-energy ESWT to the ischemic region in a porcine model of chronic myocardial ischemia. Myocardial blood flow and cardiac function were improved and enhanced VEGF production was observed in vitro and in vivo. The efficacy and safety of ESWT for patients with angina pectoris has also been reported (Fukumoto et al. 2006; Kikuchi et al. 2010). Moreover, Hayashi et al. (2012) reported that endothelial nitric oxide synthase played a critical role in ESWT-induced accelerated wound healing in diabetic mice by promoting VEGF expression and neovascularization. Clinically, Moretti et al. (2009) reported, in a controlled study, that ESWT was effective in curing and re-epithelialization of diabetic neuropathic foot ulcers. ESWT has also been applied to collagen diseases, with Tinazzi et al. (2011) reporting that ESWT improved skin sclerosis and thickening in patients with scleroderma.
Based on these results, ESWT could have the potential to stimulate new vascularization and healing when applied to the skin of SSc patients with Raynaud’s phenomenon and digital ulcers. The aim of this study was to investigate the efficacy and safety of ESWT for treatment of refractory skin ulcers caused by SSc.
Patients and Methods
Study design
This was a phase 2 pilot study conducted at Tohoku University to evaluate ESWT for the treatment of digital ulcers caused by SSc, conducted from December 2012 to November 2013. This study was approved by the Ethical Committee of Tohoku University (2012-2-130) and was published as a clinical trial under UMIN (R000013893). Written informed consent was obtained from all 9 patients before enrollment.
Subjects
All patients were confirmed to have limited or diffuse SSc, fulfilling the 1980 American College of Rheumatology criteria for SSc (Subcommittee for Scleroderma Criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee 1980) and were then assessed according to the 2013 Classification Criteria for SSc (van den Hoogen et al. 2013). For entry into the study, patients had to have one or more newly developed digital ulcers. Patients entering the study continued taking oral vasodilators or intravenous prostaglandin E1 and continued receiving treatment for other complications such as interstitial pneumonia or pulmonary hypertension. Patients younger than 20 years and those with severe cardiovascular or respiratory disorders, or infection at the site of ESWT application were excluded. Pregnant or lactating participants and patients in another trial for a new medicine for digital ulcers were also excluded.
Treatment protocol
An electromagnetic lithotripter (DUOLITH SD1 device, Storz Medical AG, Switzerland) was used for ESWT application. The treatment protocol in this study consisted of 1 session per week for 9 weeks (Fig. 1). Two hundred pressure pulses were focused on the volar side of each finger, 500 on each hand, and 500 on both forearms. Subsequently, 200 pulses were focused on the sole of each toe and 500 on the sole of both feet. In summary, 2,000 pulses were focused along each upper extremity and 1,500 along each foot, totaling 7,000 pulses in one session. The application of defocused energy started at 0.08 mJ/mm2, with a repetition frequency of 4 Hz, and was increased to 0.13 or 0.25 mJ/mm2 (≈10% of the energy for lithotripsy treatment), unless pain was sensed. Treatment did not require any kind of anesthetic.
Evaluation
The number and size of ulcers were measured before treatment began and at 9, 15, and 20 weeks after the first ESWT session (Fig. 1). Ulcers were defined as a loss of surface epithelialization and did not include fissures or cracks. Ulcers were photographed at each examination using a digital camera and the longest diameter of each ulcer was measured. Ulcer healing was considered complete when total re-epithelialization of the ulcer was observed. Skin elasticity was determined using a modified Rodnan skin score, with palpation of 17 anatomical sites and scoring on a scale of 0-3, with 0 = normal skin, 1 = slight thickening, 2 = moderate thickening, and 3 = hidebound skin sclerosis (Clements et al. 1993). A visual analog scale (VAS) and PainVision system were used to evaluate pain caused by the ulcers. The VAS assessed pain in the hand on a scale of 0-100, with 0 = best possible condition and 100 = worst possible condition. The PainVision system is a novel method for the quantitative measurement of pain intensity, using a painless electrical stimulation system (Matsumura et al. 2012). Disability parameters of the Health Assessment Questionnaire (HAQ) and the EuroQol 5 dimension (EQ-5D) questionnaire were also completed by each patient immediately prior to each session. Thermography of the whole hand was performed with a Thermoshot F30 (Nippon Avionics Co., Ltd., Tokyo, Japan). Subsequently, the temperature of each digit was calculated with an InfRec Analyzer NS9500 Standard System (Nippon Avionics Co., Ltd., Tokyo, Japan) (Cherkas et al. 2003). Prior to each temperature measurement, patients were exposed to a temperature of 21°C for 15 minutes in a thermostatic chamber. Pain VAS, HAQ and EQ-5D scores were assessed before treatment began and at 9, 15, and 20 weeks, along with the counting of the ulcers. PainVision, Rodnan skin score and thermography were evaluated before treatment began and at 9, 15, and 20 weeks (Fig. 1).
Primary outcome
The number and diameter of ulcers (larger or smaller than 5 mm) at 20 weeks following the start of ESWT treatment was the primary outcome.
Secondary outcomes
Secondary outcomes included (1) pain VAS score, PainVision score, HAQ score, EQ-5D score, fingertip temperature, and Rodnan skin score at 20 weeks following the start of ESWT treatment; (2) the number and diameter of ulcers, pain VAS score, HAQ score, and EQ-5D score for each of the 9 weeks of treatment and at 15 weeks; (3) fingertip temperature, PainVision score, and Rodnan skin score at 9 and 15 weeks; and (4) incidence of adverse effects.
Statistical analysis
Calculations were performed with the SPSS statistical package (IBM Corp., Chicago, USA). For statistical analysis, a paired Student’s t test was used, and P-values of ≤ 0.05 were considered statistically significant.
Results
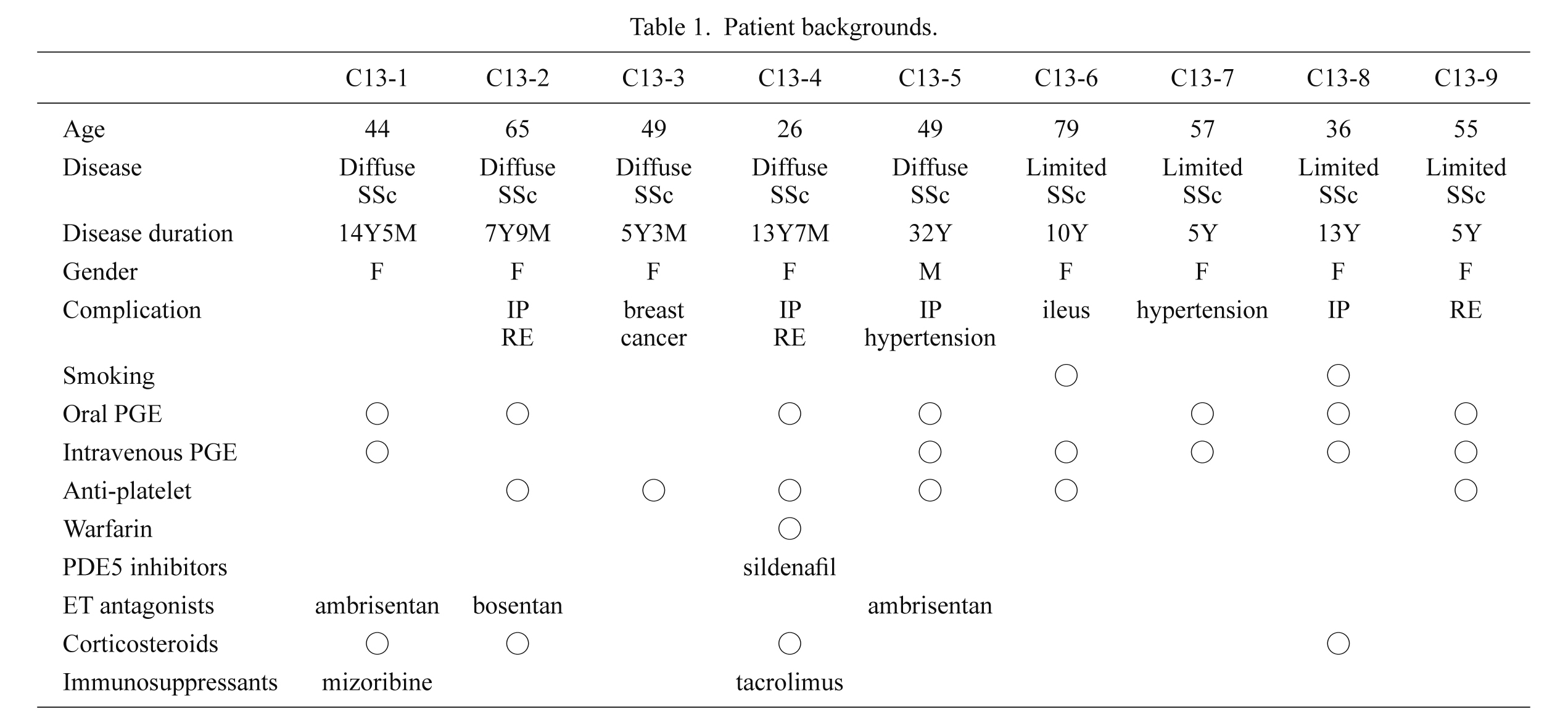
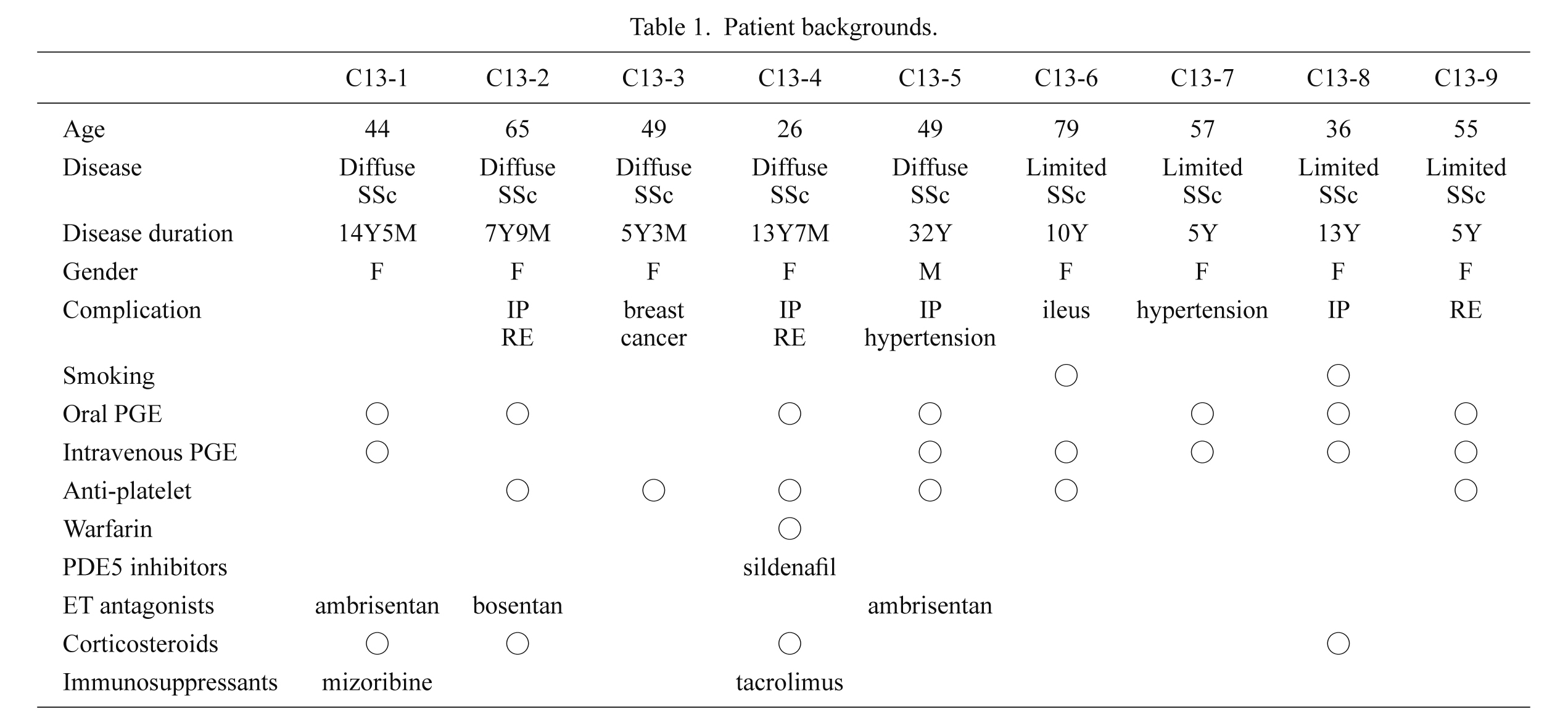
We enrolled 9 patients (8 women, 1 man), numbered as C13-1 to C13-9, aged 26-79 years (mean, 51.1 years). Five patients had diffuse cutaneous SSc and 4 had limited SSc (Table 1). Disease duration varied from 5-32 years (mean, 12.6 years). Four of the 9 patients were treated with prednisolone, 1 with tacrolimus and 1 with mizoribine. All 9 patients had taken at least 1 vasodilator, including 6 patients who took intravenous prostaglandin E1 and 7 patients who took oral prostaglandin E1. Five patients had taken both intravenous and oral prostaglandin E1. One patient also took warfarin, 6 took an antiplatelet agent, 3 took an endothelin receptor antagonist, and 1 took sildenafil, a phosphodiesterase inhibitor (Table 1). No patient had calcification at the area of ESWT application. Initially, 49 digital skin ulcers were observed in 9 patients; 40 on the fingers and 9 on the toes. The average number of ulcers per patient was 5.4. Eighteen of the ulcers were 5 mm or larger in diameter and 31 were smaller than 5 mm. The clinical features of the 9 patients are summarized in Table 2.
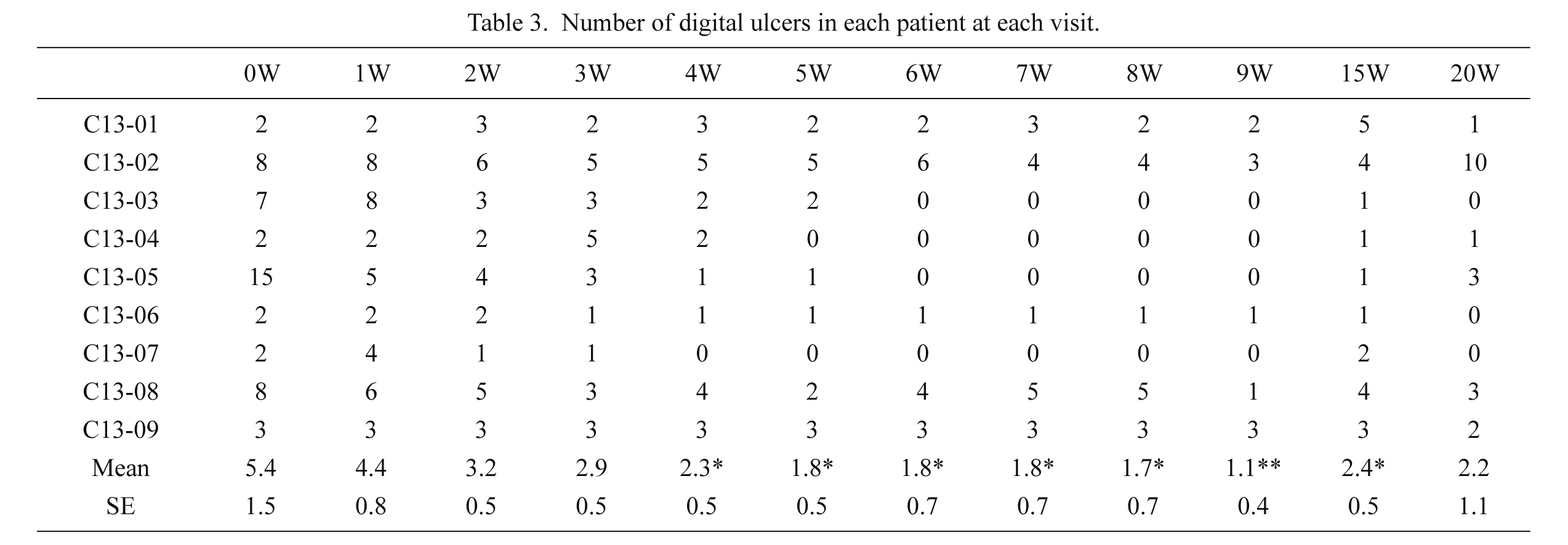
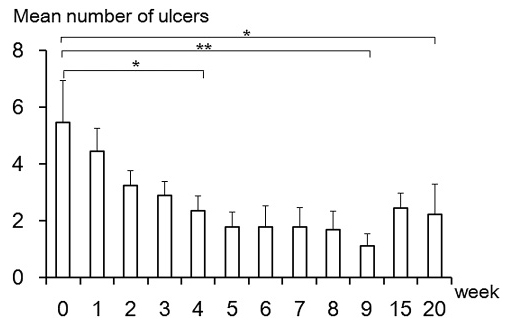
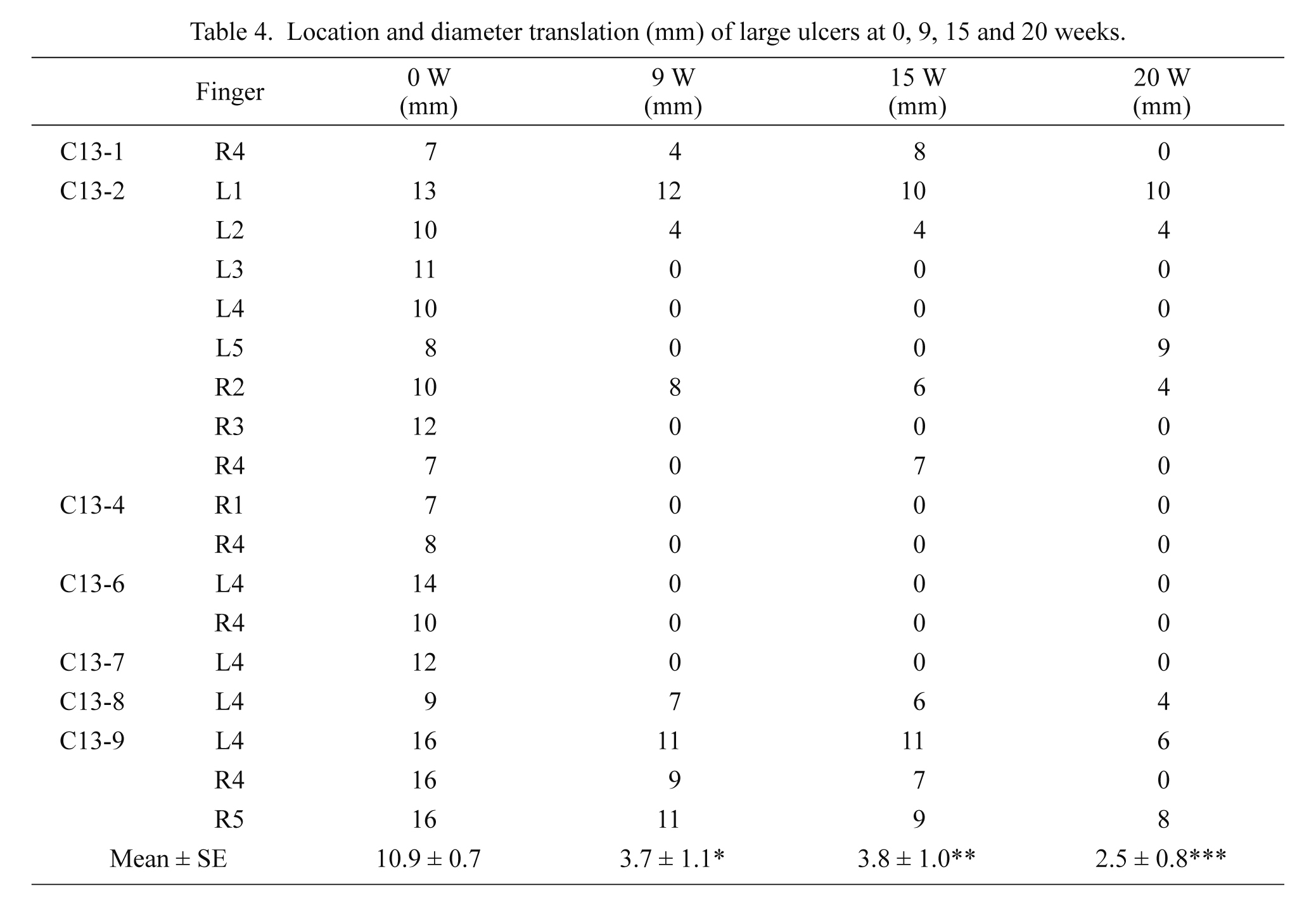
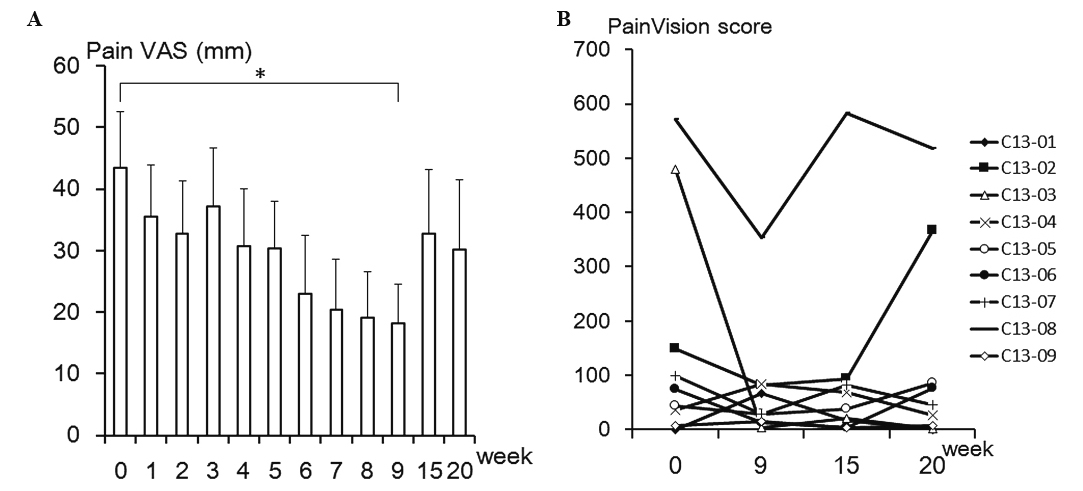
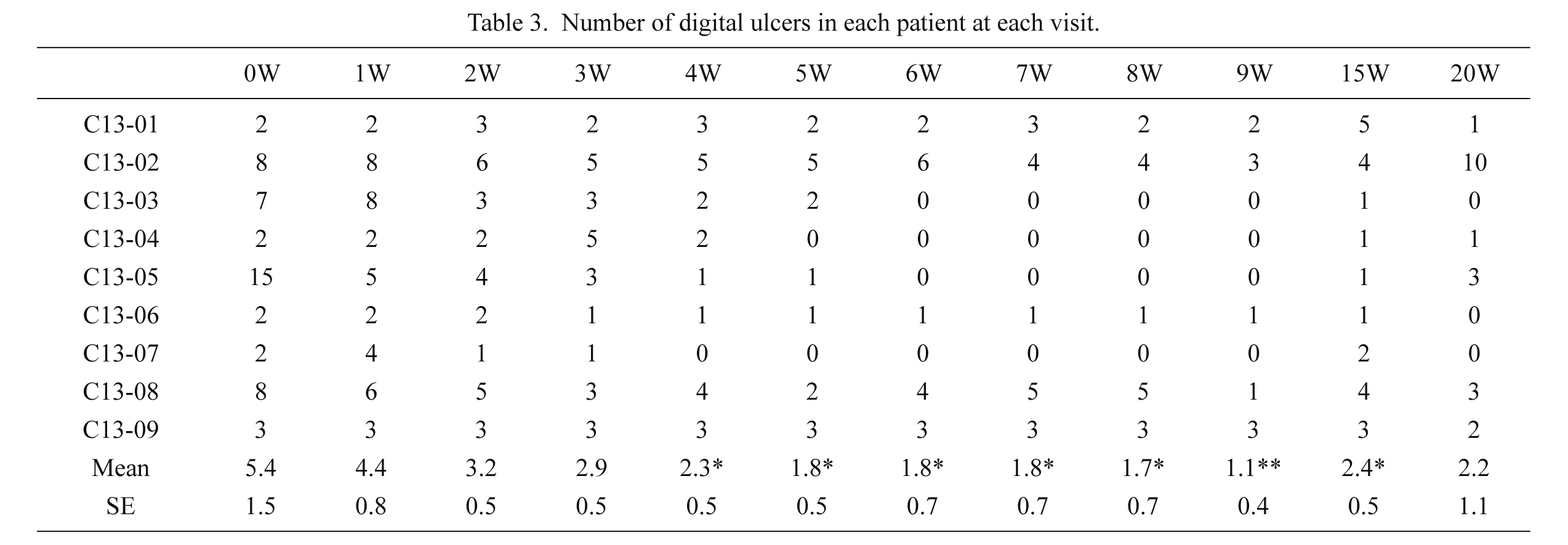
Some skin ulcers showed improvement at 1 week after the first ESWT session (Table 3). At 4 weeks, the average number of ulcers per patient was 2.3 ± 0.5, which was a significant decrease. At 9 weeks, 39 ulcers had disappeared and the average number of ulcers was 1.1 ± 0.4. At 20 weeks, ulcers had reappeared in some patients, with a mean of 2.2 ± 1.1 ulcers per patient. However, there were still significantly fewer ulcers per patient at 20 weeks than at the start of treatment (P < 0.05, Fig. 2). Thus, a positive primary outcome was achieved. In this study, we took note of large ulcers (diameter of 5 mm or larger) present in 7 patients (see Table 2). Before ESWT, 18 large ulcers existed with an average diameter of 10.9 ± 0.7 mm (Table 4). After ESWT, 10 of the large ulcers (larger than 5 mm before ESWT) had disappeared and the average diameter diminished significantly to 3.7 ± 1.1 mm at 9 weeks and 2.5 ± 0.8 mm at 20 weeks (Table 4). Fig. 3 shows the photographs of ulcers in 2 representative patients. Patient C13-2 had large ulcers on the right second and fourth digits before ESWT began. The original ulcers were improved at 9 weeks, but several new ulcers had appeared at 20 weeks (upper panel). In contrast, patient C13-9 had large ulcers on the right fourth and fifth digits before treatment. The ulcers showed apparent improvement at 9 weeks, and 1 ulcer on the fourth digit had completely disappeared at 20 weeks (lower panel). The mean VAS score improved significantly from 43.3 ± 9.3 before treatment to 18.1 ± 6.4 at 9 weeks, but worsened to 32.8 ± 10.4 and 30.2 ± 11.3 at 15 and 20 weeks, respectively (Fig. 4A). Seven patients showed improvement in PainVision scores at 9 weeks, but 6 showed worsening at 15 or 20 weeks, reflecting the reappearance of ulcers during the observation period (Fig. 4B).
Eight patients improved or did not change at 9 weeks and only 2 patients worsened at 15 and 20 weeks (Fig. 5). The mean Rodnan skin score showed significant improvement at 9, 15, and 20 weeks.
Functional assessment
Eight out of 9 patients showed a decreased functional status before ESWT, while 1 patient demonstrated no decrease in functional status on both the HAQ and EQ-5D throughout the study period. The average HAQ score before treatment was 0.57 ± 0.16. At 9 weeks, 5 patients improved, including 2 patients who achieved a full score of 0.00. The average HAQ score improved to 0.43 ± 0.15 at 9 weeks, but worsened to 0.56 ± 0.24 and 0.50 ± 0.20 at 15 and 20 weeks, respectively. These changes in HAQ score were not significant (Fig. 6A). The average EQ-5D score was 0.54 ± 0.11 before treatment, and all 8 patients improved at 9 weeks, including 2 patients who reached a full score of 1.00. The average EQ-5D score exhibited a significant increase to 0.80 ± 0.06 at 9 weeks, followed by a slight decrease to 0.68 ± 0.10 and 0.69 ± 0.11 at 15 and 20 weeks, respectively (Fig. 6B).
Fingertip temperatures
The temperature of each digit was calculated by thermographic analysis. Fig. 7 shows the mean temperature of 10 fingertips at 0, 9, 15, and 20 weeks in each patient. A significant increase in temperature was observed in 3 patients at 20 weeks but 4 patients showed a significant decrease over the same period. The average fingertip temperatures of all 9 patients did not change significantly.
Safety
No adverse events were reported during the study period, demonstrating that this treatment was minimally invasive and could be safely repeated.
Discussion
Digital ulcers are a severe complication of SSc caused by micro-vessel impairment and the persistent vasospasms associated with Raynaud’s phenomenon. In a study of 938 patients with SSc, approximately 50% of patients experienced digital ulcers, of which 10% required continuous therapy and 1% had severe symptoms, such as gangrene. Moreover, reports of permanent damage, such as scarring (53.1%) and amputation (7.3%), reveal the potential severity of this disorder (Guiducci et al. 2007; Khimdas et al. 2011).
Treatment of SSc is generally ineffective because it is impossible to modify the course of the disease, especially the components due to Raynaud’s phenomenon and stenosis of the peripheral arteries, which ultimately lead to digital ulcers. Calcium channel blockers have been used widely but there is little evidence of their effect on digital ulcers. Clinical studies have reported the efficacy of intravenous iloprost for treatment of Raynaud’s phenomenon and digital ulcers, although this treatment is costly and requires weekly administration. There is little evidence of the effects of selective phosphodiesterase inhibitors, such as sildenafil, on digital ulcers (Steen et al. 2009). The dual endothelin-1 receptor antagonist, bosentan, has demonstrated an effect on preventing development of new digital ulcers but has failed to be effective in healing ulcers already present (Korn et al. 2004; García de la Peña-Lefebvre et al. 2008).
The present study demonstrated that in patients affected by SSc, skin application of ESWT stimulated rapid improvement in digital ulcers and clinical parameters of skin wellness. The mean number of ulcers and the number of large ulcers decreased significantly at 20 weeks and the treatment achieved the primary outcome of ulcer reduction. VAS and PainVision scores also showed evidence of pain reduction. Rodnan skin scores also improved significantly at 9 and 20 weeks. However, improvements in HAQ and EQ-5D scores were not significantly different at 20 weeks. Finger temperature increased, but the difference was not significant. Some ulcers did reappear after treatment completion, accompanied by worsening pain. However, the limited effect observed during the treatment period strongly supports the effectiveness of ESWT. In addition, improvements in Rodnan skin scores, showing increases in skin wellness and elasticity, persisted at 15 and 20 weeks, even when ulcers and pain reappeared. The improvement in dermal elasticity and ulcer healing, in spite of non-significant finger temperature change, suggests that there is another mechanism of the ESWT effect, besides vascularization and increased blood flow.
In spite of the positive results shown in the current study, there are remaining issues to consider. First, the initial number of ulcers varied between patients, which made statistical analysis difficult. The effect of ESWT varied as well so predictions about treatment effectiveness based on patient characteristics was not established by this study. The small number of patients also adds limitations to predictions of treatments outcomes. An increased number of subjects and more detailed information on patient backgrounds, allowing for better treatment predictions, should be included in the next phase of studies. Second, it was difficult to distinguish the effect ESWT from spontaneous ulcer healing due to seasonal changes. Ideally, a placebo-controlled study is desirable. However, there are problems in setting up a control group for this type of treatment as patients would recognize the lack of sensation during a sham ESWT shooting, and a treatment-hand vs. control-hand study may not be valid because ESWT presumably has systemic effects, even in single-hand application. However, there is information regarding the occurrence of spontaneous healing. A randomized, double-blind, placebo-controlled study with bosentan on healing and prevention of ischemic digital ulcers in SSc, which had patients with similar backgrounds as those in the present study, showed complete healing of digital ulcers in only 20% of patients taking bosentan or the placebo after 9 weeks (Matucci-Cerinic et al. 2011). To follow up on these results, in parallel with our pilot study, we performed an observational study of digital ulcers in 30 patients with SSc receiving only conventional treatment. By comparing the ESWT study with this control group, the efficacy of ESWT should be clearly shown. Third, worsening of digital ulcers after treatment completion should be taken into account. For further investigations aimed at obtaining approval of this new therapy for the treatment of digital ulcers associated with SSc, an increased number of subjects and a practical and understandable control group are required. Moreover, treatment prolongation should be considered according to each patient’s condition after the initial treatment period.
Overall, the results of our study suggest that ESWT is a novel and efficacious treatment that can be added to pharmacological therapy. This treatment is well tolerated, can be repeated without adverse effects, and requires no anesthesia. It demonstrated rapid improvement in skin elasticity and wellness even though some beneficial effects tended to decrease over time.
Acknowledgments
We would like to thank Dr. Hiromitusu Takemori, Dr. Tsuneo Konta, Dr. Atsushi Komatsuda, Dr. Tomomasa Izumiyama, Dr. Yasuhiko Hirabayashi, Dr. Yuikio Sato, and Dr. Yukitomo Urata for their cooperation in this study of scleroderma. The present study was supported by Health and Labour Science Research Grant from the Japanese Ministry of Health, Labour and Welfare (No. 069).
Conflict of Interest
The authors declare no conflict of interest.
References
-
Abraham,
D.J. &
Varga,
J.
(2005) Scleroderma: from cell and molecular mechanisms to disease models. Trends Immunol., 26, 587-595.
-
Aicher,
A.,
Heeschen,
C.,
Sasaki,
K.,
Urbich,
C.,
Zeiher,
A.M. &
Dimmeler,
S.
(2006) Low-energy shock wave for enhancing recruitment of endothelial progenitor cells: a new modality to increase efficacy of cell therapy in chronic hind limb ischemia. Circulation, 114, 2823-2830.
-
Carvalho,
J.F.,
Blank,
M. &
Shoenfeld,
Y.
(2007) Vascular endothelial growth factor (VEGF) in autoimmune diseases. J. Clin. Immunol., 27, 246-256.
-
Cerinic,
M.M.,
Valentini,
G.,
Sorano,
G.G.,
D’Angelo,
S.,
Cuomo,
G.,
Fenu,
L.,
Generini,
S.,
Cinotti,
S.,
Morfini,
M.,
Pignone,
A.,
Guiducci,
S.,
Del Rosso,
A.,
Kalfin,
R.,
Das,
D. &
Marongiu,
F.
(2003) Blood coagulation, fibrinolysis, and markers of endothelial dysfunction in systemic sclerosis. Semin. Arthritis Rheum., 32, 285-295.
-
Cherkas,
L.F.,
Carter,
L.,
Spector,
T.D.,
Howell,
K.J.,
Black,
C.M. &
MacGregor,
A.J.
(2003) Use of thermographic criteria to identify Raynaud’s phenomenon in a population setting. J. Rheumatol., 30, 720-722.
-
Ciampa,
A.R.,
de Prati,
A.C.,
Amelio,
E.,
Cavalieri,
E.,
Persichini,
T.,
Colasanti,
M.,
Musci,
G.,
Marlinghaus,
E.,
Suzuki,
H. &
Mariotto,
S.
(2005) Nitric oxide mediates anti-inflammatory action of extracorporeal shock waves. FEBS Lett., 579, 6839-6845.
-
Clements,
P.J.,
Lachenbruch,
P.A.,
Seibold,
J.R.,
Zee,
B.,
Steen,
V.D.,
Brennan,
P.,
Silman,
A.J.,
Allegar,
N.,
Varga,
J.,
Massa,
M.,
Wigley,
F.M.,
Ingenito,
F.,
Weisman,
M.,
White,
B.,
Martin
R.W., et al.
(1993) Skin thickness score in systemic sclerosis: an assessment of interobserver variability in 3 independent studies. J. Rheumatol., 20, 1892-1896.
-
Denton,
C.P. &
Black,
C.M.
(2005) Targeted therapy comes of age in scleroderma. Trends Immunol., 26, 596-602.
-
Fukumoto,
Y.,
Ito,
A.,
Uwatoku,
T.,
Matoba,
T.,
Kishi,
T.,
Tanaka,
H.,
Takeshita,
A.,
Sunagawa,
K. &
Shimokawa,
H.
(2006) Extracorporeal cardiac shock wave therapy ameliorates myocardial ischemia in patients with severe coronary artery disease. Coron. Artery Dis., 17, 63-70.
-
García de la Peña-Lefebvre,
P.,
Rodríguez Rubio,
S.,
Valero Expósito,
M.,
Carmona,
L.,
Gámir Gámir,
M.L.,
Beltrán Gutiérrez,
J.,
Díaz-Miguel,
C.,
Orte Martínez,
J. &
Zea Mendoza,
A.C.
(2008) Long-term experience of bosentan for treating ulcers and healed ulcers in systemic sclerosis patients. Rheumatology, 47, 464-466.
-
Guiducci,
S.,
Giacomelli,
R. &
Cerinic,
M.M.
(2007) Vascular complications of scleroderma. Autoimmun. Rev., 6, 520-523.
-
Hayashi,
D.,
Kawakami,
K.,
Ito,
K.,
Ishii,
K.,
Tanno,
H.,
Imai,
Y.,
Kanno,
E.,
Maruyama,
R.,
Shimokawa,
H. &
Tachi,
M.
(2012) Low-energy extracorporeal shock wave therapy enhances skin wound healing in diabetic mice: a critical role of endothelial nitric oxide synthase. Wound Repair Regen., 20, 887-895.
-
Ito,
K.,
Fukumoto,
Y. &
Shimokawa,
H.
(2009) Extracorporeal shock wave therapy as a new and non-invasive angiogenic strategy. Tohoku J. Exp. Med., 219, 1-9.
-
Khimdas,
S.,
Harding,
S.,
Bonner,
A.,
Zummer,
B.,
Baron,
M. &
Pope,
J.
(2011) Associations with digital ulcers in a large cohort of systemic sclerosis: results from the Canadian Scleroderma Research Group registry. Arthritis Care Res., 63, 142-149.
-
Kikuchi,
Y.,
Ito,
K.,
Ito,
Y.,
Shiroto,
T.,
Tsuburaya,
R.,
Aizawa,
K.,
Hao,
K.,
Fukumoto,
Y.,
Takahashi,
J.,
Takeda,
M.,
Nakayama,
M.,
Yasuda,
S.,
Kuriyama,
S.,
Tsuji,
I. &
Shimokawa,
H.
(2010) Double-blind and placebo-controlled study of the effectiveness and safety of extracorporeal cardiac shock wave therapy for severe angina pectoris. Circ. J., 74, 589-591.
-
Korn,
J.H.,
Mayes,
M.,
Matucci Cerinic,
M.,
Rainisio,
M.,
Pope,
J.,
Hachulla,
E.,
Rich,
E.,
Carpentier,
P.,
Molitor,
J.,
Seibold,
J.R.,
Hsu,
V.,
Guillevin,
L.,
Chatterjee,
S.,
Peter,
H.H.,
Coppock,
J., et al.
(2004) Digital ulcers in systemic sclerosis: prevention by treatment with bosentan, an oral endothelin receptor antagonist. Arthritis Rheum., 50, 3985-3993.
-
Mariotto,
S.,
Cavalieri,
E.,
Amelio,
E.,
Ciampa,
A.R.,
de Prati,
A.C.,
Marlinghaus,
E.,
Russo,
S. &
Suzuki,
H.
(2005) Extracorporeal shock waves: from lithotripsy to anti-inflammatory action by NO production. Nitric Oxide, 12, 89-96.
-
Matsumura,
H.,
Imai,
R.,
Gondo,
M. &
Watanabe,
K.
(2012) Evaluation of pain intensity measurement during the removal of wound dressing material using ‘the PainVision™ system’ for quantitative analysis of perception and pain sensation in healthy subjects. Int. Wound J., 9, 451-455.
-
Matucci-Cerinic,
M.,
Denton,
C.P.,
Furst,
D.E.,
Mayes,
M.D.,
Hsu,
V.M.,
Carpentier,
P.,
Wigley,
F.M.,
Black,
C.M.,
Fessler,
B.J.,
Merkel,
P.A.,
Pope,
J.E.,
Sweiss,
N.J.,
Doyle,
M.K.,
Hellmich,
B.,
Medsger,
T.A. Jr., et al.
(2011) Bosentan treatment of digital ulcers related to systemic sclerosis: results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann. Rheum. Dis., 70, 32-38.
-
Moretti,
B.,
Notarnicola,
A.,
Maggio,
G.,
Moretti,
L.,
Pascone,
M.,
Tafuri,
S. &
Patella,
V.
(2009) The management of neuropathic ulcers of the foot in diabetes by shock wave therapy. BMC Musculoskelet. Disord., 10, 54.
-
Nishida,
T.,
Shimokawa,
H.,
Oi,
K.,
Tatewaki,
H.,
Uwatoku,
T.,
Abe,
K.,
Matsumoto,
Y.,
Kajihara,
N.,
Eto,
M.,
Matsuda,
T.,
Yasui,
H.,
Takeshita,
A. &
Sunagawa,
K.
(2004) Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia-induced myocardial dysfunction in pigs in vivo. Circulation, 110, 3055-3061.
-
Poole,
J.L.,
Watzlaf,
V.J. &
D’amico,
F.
(2004) A five-year followup of hand function and activities of daily living in systemic sclerosis (scleroderma). J. Hand Ther., 17, 407-411.
-
Schaden,
W.,
Thiele,
R.,
Kölpl,
C.,
Pusch,
M.,
Nissan,
A.,
Attinger,
C.E.,
Maniscalco-Theberge,
M.E.,
Peoples,
G.E.,
Elster,
E.A. &
Stojadinovic,
A.
(2007) Shock wave therapy for acute and chronic soft tissue wounds: a feasibility study. J. Surg. Res., 143, 1-12.
-
Steen,
V.,
Denton,
C.P.,
Pope,
J.E. &
Matucci-Cerinic,
M.
(2009) Digital ulcers: overt vascular disease in systemic sclerosis. Rheumatology (Oxfod), 48 Suppl 3, iii19-24.
-
Subcommittee for Scleroderma Criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee
(1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum., 23, 581-590.
-
Tinazzi,
E.,
Amelio,
E.,
Marangoni,
E.,
Guerra,
C.,
Puccetti,
A.,
Codella,
O.M.,
Simeoni,
S.,
Cavalieri,
E.,
Montagnana,
M.,
Adani,
R.,
Corrocher,
R. &
Lunardi,
C.
(2011) Effects of shock wave therapy in the skin of patients with progressive systemic sclerosis: a pilot study. Rheumatol. Int., 31, 651-656.
-
van den Hoogen,
F.,
Khanna,
D.,
Fransen,
J.,
Johnson,
S.R.,
Baron,
M.,
Tyndall,
A.,
Matucci-Cerinic,
M.,
Naden,
R.P.,
Medsger,
T.A. Jr.,
Carreira,
P.E.,
Riemekasten,
G.,
Clements,
P.J.,
Denton,
C.P.,
Distler,
O.,
Allanore,
Y., et al.
(2013) 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum., 65, 2737-2747.