Abstract
Intravascular large B-cell lymphoma (IVLBCL) is a rare subtype of diffuse large B-cell lymphoma. There have been only a limited number of reports regarding pituitary dysfunction associated with IVLBCL. We present a 71-year-old woman with hypopituitarism without any hypothalamic/pituitary abnormalities as assessed by magnetic resonance imaging. She presented with edema, abducens palsy, and elevated levels of lactate dehydrogenase and soluble interleukin-2 receptor. Provocative testing showed that the peaks of luteinizing hormone, follicle-stimulating hormone, thyroid-stimulating hormone and adrenocorticotropic hormone were evoked to normal levels by simultaneous administration of luteinizing hormone-releasing hormone, thyrotropin-releasing hormone and corticotropin-releasing hormone, but the responses of these four pituitary hormones showed a delayed pattern. She was diagnosed with IVLBCL with cerebrospinal invasion by pathological findings of the bone marrow, skin, and cerebrospinal fluid. She achieved hematological remission after immunochemotherapy. Pituitary function was also restored without hormonal replacement, and the improvement of the pituitary function was confirmed by dynamic testing. We reviewed the literature with respect to hypopituitarism associated with IVLBCL. There were less than 20 case reports and most of the patients died. Endocrinological course was described in only two cases, and both of them required hormonal supplementation. To our knowledge, this is the first case of hypopituitarism induced by IVLBCL that was successfully managed by immunochemotherapy alone. This case suggests that early diagnosis and treatment of IVLBCL might improve anterior pituitary function and enable patients to avoid hormone replacement therapy.
Introduction
Intravascular large B-cell lymphoma (IVLBCL) is a rare subtype of diffuse large B-cell lymphoma characterized by the proliferation of lymphoma cells within the lumina of small blood vessels, according to the World Health Organization (WHO) classification (Nakamura et al. 2008). Because lymphoma cells invade the blood vessels throughout the whole body, IVLBCL shows a wide variety of clinical manifestations. IVLBCL is an aggressive disease and often results in severe outcomes (Ferreri et al. 2004). However, the prognosis of patients has been greatly improved by the introduction of rituximab, a recombinant monoclonal antibody against CD20 (Shimada et al. 2008).
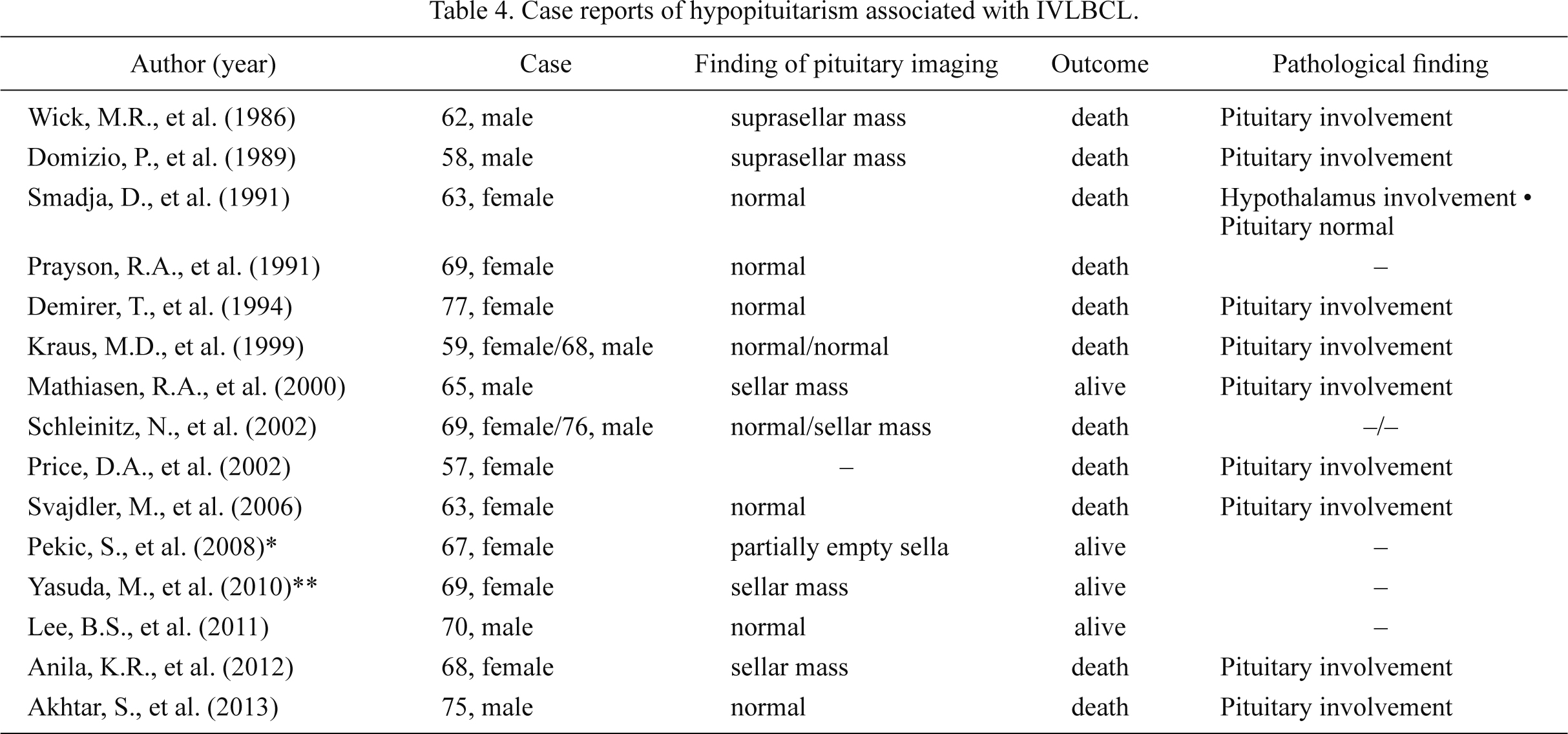
Pituitary insufficiency is induced by various disorders, including a pituitary tumor, trauma, inflammation, apoplexy, and developmental defects. A precise evaluation of pituitary function often requires provocative testing. Patients with hypopituitarism are usually treated with hormone replacement therapy (Carmichael 2011). Lymphoma is one of the potential causes for pituitary dysfunction, whereas there have been less than 20 case reports of hypopituitarism induced by IVLBCL. Moreover, only two reports have described the course of hormone levels after treatment of IVLBCL (Pekic et al. 2008; Yasuda et al. 2010).
Here we present a case of hypopituitarism associated with IVLBCL. The patient was treated with immunochemotherapy. The patient’s pituitary function recovered after hematological remission without hormonal replacement therapy, which was assessed by a pituitary stimulation test. To our knowledge, this is the first report of hypopituitarism induced by IVLBCL that was successfully treated with immunochemotherapy alone without hormonal replacement.
Case Presentation
A 71-year-old woman was admitted to our hospital with complaints of eyelid edema for the past 2 months and diplopia for the past few days. She did not have any particular medical history other than hypertension. None of her family had similar symptoms. She did not show any abnormal findings in her vital signs on admission. Physical examination demonstrated bilateral edema in her eyelids and lower legs, and right abducens nerve palsy. There was no hepatosplenomegaly, lymph node enlargement, or skin eruption. Laboratory investigation revealed significantly elevated serum lactate dehydrogenase (LDH) level, with dominance of fractions 2 and 3. Soluble interleukin-2 receptor (sIL-2R) level was also moderately high (Table 1). Anti-pituitary antibody was negative and IgG4 level was within normal limits. A contrast-enhanced magnetic resonance imaging (MRI) study revealed no abnormal findings in the brain, including the pituitary gland and hypothalamus (Fig. 1). Organs in the chest and abdominal cavity looked normal by computed tomography (CT) studies. 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) was not performed in this case.
Eyelid and pretibial edema led us to assess her endocrinological status, including thyroid function. The patient suffered from panhypopituitarism on hospital days 2 and 13 before immunochemotherapy was started (Table 2, left). The levels of luteinizing hormone (LH), follicle-stimulating hormone (FSH) and adrenocorticotropic hormone (ACTH) were low, while prolactin level was slightly high. The levels of LH and FSH were lower on day 13 as compared to day 2. This might be due to rapid progression of IVLBCL. Low free thyroxin (fT4) and free triiodothyronine (fT3) levels with normal thyroid-stimulating hormone (TSH) suggested central hypothyroidism. Cortisol concentration was normal despite the low ACTH level. Urinary free cortisol level was also within normal range (70.0 µg/day, normal range: 11.2-80.3). The secretion of growth hormone (GH) and insulin-like growth factor-1 (IGF-1) did not look disturbed. To further study the function of anterior pituitary gland, provocative tests were performed. For this purpose, 100 µg of luteinizing hormone-releasing hormone (LH-RH), 200 µg of thyrotropin-releasing hormone (TRH) and 100 µg of corticotropin-releasing hormone (CRH) were simultaneously administered, and the serum levels of anterior pituitary hormones were measured at 0, 30, 60 and 90 minutes. The peaks of LH, FSH, TSH, and ACTH were evoked to normal levels, but the responses of these four hormones showed a delayed pattern. The response of prolactin to TRH was normal (Table 3, top). Imaging studies did not indicate pituitary diseases, such as pituitary tumor, lymphocytic hypophysitis, vascular diseases, or trauma. Based on her past history, it was not likely that a brain injury or severe hemorrhage in the parturition caused the hypopituitarism.
On the second hospital day, she developed an intermittent fever and night sweats. On the sixth day, atypical lymphocytes appeared in peripheral blood. Despite the absence of lymphadenopathy or tumors, her symptoms and elevated LDH and sIL-2R levels suggested malignant lymphoma rather than an infectious disease or a connective tissue disease. On the 11th day, bone marrow biopsy, random skin biopsy, and examination of spinal fluid were performed. Pathological studies demonstrated lymphoid aggregates in the small blood vessels within the bone marrow and skin, but lymphoid cells were not found outside of the vessels. Bone marrow aspiration was performed at the same time, but we obtained only peripheral blood sample, which contained atypical lymphoma cell clusters. Atypical lymphocytes were also found in the cerebrospinal fluid. Immunohistochemistry revealed that lymphoma cells were positive for CD20 (a B-cell marker, Fig. 2), CD5 (a B1-cell/T-cell marker), bcl-6 (a B-cell lymphoma marker), and bcl-2 (a B-cell lymphoma marker), but were negative for CD3 (a T-cell marker), CD10 (a germinal center B-cell marker), cyclin D1 (a proliferative marker), and CD34 (a Hematopoietic stem cell marker). She was diagnosed with IVLBCL with cerebrospinal infiltration two weeks after admission.
She was immediately treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP). 80 mg of prednisolone per day was orally administered for five days. In addition, we intrathecally administered methotrexate, arabinofuranosylcytosine, and 10 mg of prednisolone, because R-CHOP therapy might not have been effective for the cerebrospinal infiltration. She did not take any hormonal supplementation during immunochemotherapy. Her right abducens nerve palsy, edema, intermittent fever, and night sweats disappeared, and the levels of LDH and sIL-2R normalized after 2 cycles of R-CHOP immunochemotherapy. Thereafter, we added 2 courses of chemotherapy consisting of high dose methotrexate, vincristine and mercaptopurine, and she achieved clinical remission. We confirmed the absence of any atypical lymphoid cells in the bone marrow or cerebrospinal fluid. She did not have any severe adverse events during immunochemotherapy.
We reevaluated her hormonal status on day 51, when the effect of prednisolone was minimal because it was just before the third course of chemotherapy. Although the patient did not receive any hormonal replacement, the levels of LH, FSH, TSH, ACTH, and prolactin returned to normal. The endocrinological status remained normal on day 114, 39 days after the final course of chemotherapy (Table 2, right). Dynamic testing on day 114 showed significant improvement in LH, FSH, TSH, ACTH, and prolactin responses, although still delayed (Table 3, bottom). Polydipsia or polyuria was not observed and serum sodium levels were normal throughout the clinical course, suggesting that the posterior pituitary function was not perturbed.
Discussion
IVLBCL is a rare subtype of B-cell lymphoma. IVLBCL is characterized by massive neoplastic proliferation of lymphoid cells within the lumina of capillaries and small blood vessels (Nakamura et al. 2008). The diagnosis is not easy because the patients have general nonspecific clinical symptoms, and probably because IVLBCL is not widely known among clinicians. Furthermore, IVLBCL often can be an aggressive disease and results in severe outcomes (Ferreri et al. 2004). Thus, the diagnosis of IVLBCL had been often made based on postmortem examinations in previous reports (Domizio et al. 1989). However, advances in diagnostic technology and the recognition of the disease have increased the diagnostic yield for IVLBCL in recent years. In addition, novel immunochemotherapy using rituximab, a recombinant monoclonal antibody against CD20, has greatly improved clinical outcomes of patients with IVLBCL (Shimada et al. 2008).
The mechanism for the selective intravascular growth pattern remains unexplained. It has been proposed that the lack of key molecule expression for lymphocyte-endothelial adhesion, including CD29 (β-1 integrin subunit) and CD54 (ICAM-1), on the lymphoma cell surface may contribute to an intravascular and disseminated distribution pattern of lymphoma cells in IVLBCL (Ponzoni et al. 2000). Diagnosis of IVLBCL requires pathological identification of lymphoma cells within blood vessels. Bone marrow biopsy and random skin biopsy are frequently performed for this purpose. Because many patients with IVLBCL have accompanying multiple organ failure and hemorrhagic diathesis, it can be difficult to perform an invasive biopsy. Accordingly, as random skin biopsy is regarded as minimally invasive, it is the established diagnostic method (Gill et al. 2003; Asada et al. 2007; Barnett et al. 2008). In our case, random skin biopsies provided findings of IVLBCL, although the patient did not show any abnormal skin lesions.
IVLBCL is a systemic disease and pathological findings have been reported in many types of organs, such as the brain, skin, bone marrow, spleen, liver, and lung (Ferreri et al. 2004; Murase et al. 2007; Shimada et al. 2008). Occlusion of capillaries by lymphoma cells in multiple organs results in extremely variable clinical manifestations. In addition, patients with IVLBCL present with variable B symptoms, such as fever, weight loss, night sweats, malaise, fatigue, cutaneous lesions, neurological symptoms, gastrointestinal symptoms, edema, and dyspnea (Carmichael 2011). Laboratory findings of IVLBCL often show anemia, leukocytopenia, thrombocytopenia, hypoalbuminemia, and elevated C-reactive protein (CRP), LDH, and sIL-2R levels (Ferreri et al. 2004; Ponzoni et al. 2007; Shimada et al. 2009). IVLBCL with cranial neuropathies has often been reported; facial and auditory nerves are the most commonly affected ones, but disturbances in abducens and oculomotor nerves have also been described in the literature (Glass et al. 1993). In our case, the patient recovered from right abducens nerve palsy after hematological remission of IVLBCL, suggesting that the neuropathy was induced by lymphoma.
Hypopituitarism associated with IVLBCL has been described in less than 20 reports. Moreover, many of the patients died, and the hormonal evaluation after treatment was not always mentioned even in the survived cases (Wick et al. 1986; Smadja et al. 1991; Prayson et al. 1991; Demirer et al. 1994; Kraus et al. 1999; Mathiasen et al. 2000; Schleinitz et al. 2002; Price et al. 2002; Svajdler et al. 2006; Lee et al. 2011; Anila et al. 2012; Akhtar et al. 2013). Thus far, the endocrinological course has been described in only two cases in the literature (Table 4) (Pekic et al. 2008; Yasuda et al. 2010). In both cases, hormone replacement therapy was necessary. However, our patient did not need any hormonal supplementation. This might have been because we were able to start hematological therapy at earlier stage of the disease. Lymphoma cells invade capillaries of the pituitary gland or hypothalamus in most necropsy cases with pituitary IVLBCL. Therefore, it is suggested that hypopituitarism is induced by vascular occlusion by the lymphoid tumor cells in the hypothalamus or pituitary gland. Accordingly, it is possible that amelioration of pituitary/hypothalamic infarction improves pituitary function when damage is not irreversible. Our case suggests that early diagnosis and treatment of IVLBCL might improve anterior pituitary function and enable patients to avoid hormone replacement therapy, although there remains a possibility that the severity of lymphoma in our case was milder than that in previously reported cases. Another possible reason why the patient needed no hormonal supplementation may be the normal levels of cortisol before the treatment. These facts enabled us to avoid emergent glucocorticoid supplementation. In addition, prednisolone administered during the chemotherapy would have been beneficial for the patient. Case reports of hypopituitarism induced by IVLBCL have been limited, but the frequency might be higher because endocrinological evaluation is often absent. We also inquired whether there are any reports in which hypopituitarism induced by malignant lymphoma, other than IVLBCL, was successfully managed by immunochemotherapy alone. But, at least to our knowledge, we did not find any manuscript. Many patients with hypopituitarism accompanied by pituitary or hypothalamic lymphoma underwent surgery for the purpose of both diagnosis and treatment. Another potential reason why patients were not treated with immunochetherapy alone was that many case reports were written when rituximab was not available. These patients needed radiation with chemotherapy because CHOP chemotherapy was not effective enough for B-cell type lymphoma without rituximab.
Although we do not have pathological evidence, we speculate that intravascular lymphoma cells might have affected the hypothalamus rather than the pituitary gland based on the dynamic stimulation test before treatment. Increases in LH, FSH, TSH, and ACTH levels were observed but the responses showed a delayed pattern. Mildly elevated prolactin level is also consistent with hypothalamic involvement because hypothalamic disease would suppress the secretion of prolactin-inhibiting factor. To our knowledge, there has been only one report of hypothalamic involvement (Smadja et al. 1991). The patient exhibited a wide variety of neurological symptoms and hypopituitarism, but the information obtained from pituitary provocative test was not sufficient, probably because the authors had to pay more attention to severe symptoms such as hemiparesis and decerebration reaction. In fact, the authors were able to make a diagnosis of IVLBCL by autopsy. Most cases of IVLBCL with hypopituitarism are accompanied by an enlarged pituitary gland, whereas normal-sized pituitaries and empty sella have been described as well. In contrast, similarly to our case, this patient did not show any abnormal findings in the hypothalamus or pituitary gland as demonstrated by MRI.
Cortisol concentration was normal despite the low ACTH level. Because abdominal CT did not show any abnormalities in the adrenal gland, and a response of ACTH to CRH stimulation was observed, autonomous secretion of cortisol in the adrenal gland did not likely occur. The effect of stress due to fever could induce ACTH-dependent hypercortisolemia, but the ACTH level was low in our case. Although the reason why the cortisol level was maintained is not clear, it has been reported that interleukin-6 (IL-6) stimulates the production of cortisol in adrenocortical cells (Weber et al. 1997). Our patient showed a slightly increased level of IL-6 (Table 1). So it might be possible that IL-6, to some extent, contributed to the secretion of cortisol.
In conclusion, we present a female IVLBCL patient with hypopituitarism and abducens palsy. This is the first report of hypopituitarism induced by IVLBCL that was successfully treated by immunochemotherapy without hormonal replacement. Recovery of pituitary function was also confirmed by provocative pituitary testing. This case suggests that early diagnosis and treatment of IVLBCL might improve anterior pituitary function and enable patients to avoid hormone replacement therapy.
Conflict of Interest
The authors declare no conflict of interest.
References
-
Akhtar,
S.,
Cheesman,
E. &
Jude,
E.B.
(2013) SIADH and partial hypopituitarism in a patient with intravascular large B-cell lymphoma: a rare cause of a common presentation. BMJ Case Rep., 2013, 2013.
-
Anila,
K.R.,
Nair,
R.A.,
Koshy,
S.M. &
Jacob,
P.M.
(2012) Primary intravascular large B-cell lymphoma of pituitary. Indian J. Pathol. Microbiol., 55, 549-551.
-
Asada,
N.,
Odawara,
J.,
Kimura,
S.,
Aoki,
T.,
Yamakura,
M.,
Takeuchi,
M.,
Seki,
R.,
Tanaka,
A. &
Matsue,
K.
(2007) Use of random skin biopsy for diagnosis of intravascular large B-cell lymphoma. Mayo Clin. Proc., 82, 1525-1527.
-
Barnett,
C.R.,
Seo,
S.,
Husain,
S. &
Grossman,
M.E.
(2008) Intravascular B-cell lymphoma: the role of skin biopsy. Am. J. Dermatopathol., 30, 295-299.
-
Carmichael,
J.D.
(2011) Anterior Pituitary failure. In The Pituitary, 3rd ed., edited by
Mermed,
S.
Elsevier, Amsterdam, pp. 343-381.
-
Demirer,
T.,
Dail,
D.H. &
Aboulafia,
D.M.
(1994) Four varied cases of intravascular lymphomatosis and a literature review. Cancer, 73, 1738-1745.
-
Domizio,
P.,
Hall,
P.A.,
Cotter,
F.,
Amiel,
S.,
Tucker,
J.,
Besser,
G.M. &
Levison,
D.A.
(1989) Angiotropic large cell lymphoma (ALCL): morphological, immunohistochemical and genotypic studies with analysis of previous reports. Hematol. Oncol., 7, 195-206.
-
Ferreri,
A.J.M.,
Campo,
E.,
Seymour,
J.F.,
Willemze,
R.,
Ilariucci,
F.,
Ambrosetti,
A.,
Zucca,
E.,
Rossi,
G.,
López-Guillermo,
A.,
Pavlovsky,
M.A.,
Geerts,
M.L.,
Candoni,
A.,
Lestani,
M.,
Asioli,
S.,
Milani,
M.,
et al.
(2004) Intravascular lymphoma: clinical presentation, natural history, management and prognostic factors in a series of 38 cases, with special emphasis on the ‘cutaneous variant’. Br. J. Haematol., 127, 173-183.
-
Gill,
S.,
Melosky,
B.,
Haley,
L. &
ChanYan,
C.
(2003) Use of random skin biopsy to diagnose intravascular lymphoma presenting as fever of unknown origin. Am. J. Med., 114, 56-58.
-
Glass,
J.,
Hochberg,
F.H. &
Miller,
D.C.
(1993) Intravascular lymphomatosis: a systemic disease with neurologic manifestations. Cancer, 71, 3156-3164.
-
Kraus,
M.D.,
Jones,
D. &
Bartlett,
N.L.
(1999) Intravascular lymphoma associated with endocrine dysfunction: a report of four cases and a review of the literature. Am. J. Med., 107, 169-176.
-
Lee,
B.S.,
Frankfort,
B.J.,
Eberhart,
C.G. &
Weinberg,
R.S.
(2011) Diagnosis of intravascular lymphoma by a novel biopsy site. Ophthalmology, 118, 586-590.
-
Mathiasen,
R.A.,
Jarrahy,
R.,
Cha,
S.T.,
Kovacs,
K.,
Herman,
V.S.,
Ginsberg,
E. &
Shahinian,
H.K.
(2000) Pituitary lymphoma: a case report and literature review. Pituitary, 2, 283-287.
-
Murase,
T.,
Yamaguchi,
M.,
Suzuki,
R.,
Okamoto,
M.,
Sato,
Y.,
Tamaru,
J.,
Kojima,
M.,
Miura,
I.,
Mori,
N.,
Yoshino,
T. &
Nakamura,
S.
(2007) Intravascular large B-cell lymphoma (IVLBCL): a clinicopathologic study of 96 cases with special reference to the immunophenotypic heterogeneity of CD5. Blood, 109, 478-485.
-
Nakamura,
S.,
Ponzoni,
M. &
Campo,
E.
(2008) Intravascular large B-cell lymphoma. In WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues, 4th ed., edited by
Swerdlow,
S.H.,
Campo,
E.,
Harris,
N.L.,
Jaffe,
E.S.,
Pileri,
S.A.,
Stein,
H.,
Thiele,
J. &
Vardiman,
J.W.
IARC Press, Lyon, pp. 252-253.
-
Pekic,
S.,
Milicevic,
S.,
Colovic,
N.,
Colovic,
M. &
Popovic,
V.
(2008) Intravascular large B-cell lymphoma as a cause of hypopituitarism: gradual and late reversal of hypopituitarism after long-term remission of lymphoma with immunochemotherapy. Endocrine, 34, 11-16.
-
Ponzoni,
M.,
Arrigoni,
G.,
Gould,
V.E.,
Del Curto,
B.,
Maggioni,
M.,
Scapinello,
A.,
Paolino,
S.,
Cassisa,
A. &
Patriarca,
C.
(2000) Lack of CD 29 (beta1 integrin) and CD 54 (ICAM-1) adhesion molecules in intravascular lymphomatosis. Hum. Pathol., 31, 220-226.
-
Ponzoni,
M.,
Ferreri,
A.J.M.,
Campo,
E.,
Facchetti,
F.,
Mazzucchelli,
L.,
Yoshino,
T.,
Murase,
T.,
Pileri,
S.A.,
Doglioni,
C.,
Zucca,
E.,
Cavalli,
F. &
Nakamura,
S.
(2007) Definition, diagnosis, and management of intravascular large B-cell lymphoma: proposals and perspectives from an international consensus meeting. J. Clin. Oncol., 25, 3168-3173.
-
Prayson,
R.A.,
Segal,
G.H.,
Stoler,
M.H.,
Licata,
A.A. &
Tubbs,
R.R.
(1991) Angiotropic large-cell lymphoma in a patient with adrenal insufficiency. Arch. Pathol. Lab. Med., 115, 1039-1041.
-
Price,
D.A.,
Thaker,
H.,
James,
A. &
Snow,
M.H.
(2002) Hypopituitarism in a patient with intravascular lymphomatosis. Haematologica, 87, ECR36.
-
Schleinitz,
N.,
Bernit,
E.,
Mazodier,
K.,
Charbonnier,
A.,
Horchowski,
N.,
Andrac-Meyer,
L.,
Veit,
V. &
Harle,
J.R.
(2002) Two cases of intravascular lymphomatosis disclosing with hypopituitarism. Haematologica, 87, ECR21.
-
Shimada,
K.,
Kinoshita,
T.,
Naoe,
T. &
Nakamura,
S.
(2009) Presentation and management of intravascular large B-cell lymphoma. Lancet Oncol., 10, 895-902.
-
Shimada,
K.,
Matsue,
K.,
Yamamoto,
K.,
Murase,
T.,
Ichikawa,
N.,
Okamoto,
M.,
Niitsu,
N.,
Kosugi,
H.,
Tsukamoto,
N.,
Miwa,
H.,
Asaoku,
H.,
Kikuchi,
A.,
Matsumoto,
M.,
Saburi,
Y.,
Masaki,
Y., et al.
(2008) Retrospective analysis of intravascular large B-cell lymphoma treated with rituximab-containing chemotherapy as reported by the IVL study group in Japan. J. Clin. Oncol., 26, 3189-3195.
-
Smadja,
D.,
Mas,
J.L.,
Fallet-Bianco,
C.,
Meyniard,
O.,
Sicard,
D.,
de Recondo,
J. &
Rondot,
P.
(1991) Intravascular lymphomatosis (neoplastic angioendotheliosis) of the central nervous system: case report and literature review. J. Neurooncol., 11, 171-180.
-
Svajdler,
M.,
Lazurova,
I.,
Bohus,
P. &
Pal’ko,
M.
(2006) Intravascular variant of diffuse large B-cell lymphoma with combined endocrine involvement. Wien. Klin. Wochenschr., 118, 422-425.
-
Yasuda,
M.,
Akiyama,
N.,
Miyamoto,
S.,
Warabi,
M.,
Takahama,
Y.,
Kitamura,
M.,
Yakushiji,
F. &
Kinoshita,
H.
(2010) Primary sellar lymphoma: intravascular large B-cell lymphoma diagnosed as a double cancer and improved with chemotherapy, and literature review of primary parasellar lymphoma. Pituitary, 13, 39-47.
-
Weber,
M.M.,
Michl,
P.,
Auernhammer,
C.J. &
Engelhardt,
D.
(1997) Interleukin-3 and interleukin-6 stimulate cortisol secretion from adult human adrenocortical cells. Endocrinology, 138, 2207-2210.
-
Wick,
M.R.,
Mills,
S.E.,
Scheithauer,
B.W.,
Cooper,
P.H.,
Davitz,
M.A. &
Parkinson,
K.
(1986) Reassessment of malignant “angioendotheliomatosis”. Evidence in favor of its reclassification as “intravascular lymphomatosis”. Am. J. Surg. Pathol., 10, 112-123.