2017 Volume 241 Issue 3 Pages 189-199
2017 Volume 241 Issue 3 Pages 189-199
In Japan, patients who require home medical care are increasing especially in the elderly. In home medical care settings, devices such as gastrostomy tubes, tracheal cannulas, and urethral catheters are usually replaced by visiting physicians or nurses. However, device replacement services are not always available in Japan. Unless device replacement services are sufficiently provided to patients at home, patients have to suffer various disadvantages, including a forced visit to a hospital for device replacement despite inability to walk. We therefore investigated background factors of clinics and nursing stations providing home-care visits using a cross-sectional postal survey from August to September 2013. We targeted physicians from 5,828 clinics providing home medical care and nurses from 1,798 home-visit nursing stations across six prefectures (Tokyo, Kanagawa, Saitama, Chiba, Miyagi and Iwate). Responses were received from 933 clinics (16.5%) and 552 stations (31.3%). We analyzed the responses using multivariable logistic regression with two models. “Model 1” mainly included the number of full-time staff and the availability of a 24-hour care service system, and “Model 2” mainly included the number of clinics, the number of home-visit nursing stations, and the ratio of the population aged ≥ 65 years to study the influence of medical resources. We thus found that clinic staff numbers and 24-hour care availability were associated with physicians’ replacement of gastrostomy tubes and tracheal cannulas (p < 0.001 for each). In conclusion, single-handed and group practices need to cooperate to ensure the replacement of these devices in home medical care settings.
In Japan, patients who require home medical care are increasing not only in the elderly but also in children, and demand for home medical care is increasing. There are increasing numbers of patients who are unable to attend healthcare facilities and/or who choose to receive medical care at home (Ozawa and Nakayama 2005; World Health Organization 2014; Center for Home Care Medicine, Faculty of Medicine, The University of Tokyo 2015) . In Japan, home medical care is provided by physicians and visiting nurses (Center for Home Care Medicine, Faculty of Medicine, The University of Tokyo 2015). Japan’s home medical care is considered to be unique as compared with other developed countries in that physicians play a leading role in care without delegating care to nurses (Monsen and de Blok 2013; Young et al. 2016).
A variety of medical services are provided in patients’ homes. For example, devices such as gastrostomy tubes, nasogastric tubes, tracheal cannulas, and urethral catheters are regularly used and replaced relatively frequently (Center for Home Care Medicine, Faculty of Medicine, The University of Tokyo 2015). As most patients who receive home medical care are unable to attend healthcare facilities, home-based device replacement services are necessary, regardless of the available medical resources. As far as the authors know, there is no literature in Europe and the United States reporting that device replacement services are not always available in home medical care settings. However, device replacement services are not always available in Japan, and the reasons for this are unclear. Unless device replacement services are sufficiently provided to patients in home medical care settings, patients will have to suffer various disadvantages; for example, they are forced to visit a hospital for device replacement even if they have difficulties in going out of the home, and the use of devices at home is restricted for the reason that they chose medical care at home. We therefore investigated background factors of those providing home-care visits.
Physicians and visiting nurses are responsible for device care. This responsibility includes re-insertion of devices if one is accidentally removed, which may require an emergency visit, so a 24-hour care service system is important. In Japan, however, some clinics and home-visit nursing stations do not provide a 24-hour care service system (Ministry of Health, Labour and Welfare of Japan 2013a, b; Center for Home Care Medicine, Faculty of Medicine, The University of Tokyo 2015). Clinics and nursing stations with more staff may be better able to provide a 24-hour care service system (including holiday cover). However, there are a lot of single-handed clinics and nursing stations with fewer staff in Japan (Ministry of Health, Labour and Welfare of Japan 2013a, b).
In other words, the number of staff and 24-hour availability of care differs from facility to facility even among clinics and nursing stations that provide 24-hour care services. To examine the factors related to device replacement in home settings, we formulated a hypothesis that, besides factors personal to physicians and nurses, such as years of home-visit care experience, (1) higher staff numbers are linked to more frequent device replacement, and (2) device replacement is more likely to happen from facilities providing a 24-hour care service system. This hypothesis was used to clarify the relationship between these factors, with a view to improving the device replacement system in Japan. We examined background factors among physicians and nurses who carry out device replacement in home medical care settings.
We used an anonymous self-administered postal questionnaire, from August to September 2013. Participants were physicians from clinics that provided home medical care and visiting nurses from home-visit nursing stations who worked in six areas in Japan. These were Tokyo and three adjoining prefectures (Kanagawa, Saitama and Chiba) that are expected to have significant aged populations in future, and two prefectures in Tohoku (Iwate and Miyagi) that have had marked decreases in medical resources because of the tsunami associated with the Great East Japan Earthquake in 2011. Questionnaires were sent to all physicians who worked in the 5,828 clinics listed as providing home medical care services (on the information on regional medical services website) and all nurses from 1,798 home-visit nursing stations (listed on the information on healthcare services website (Ministry of Health, Labour and Welfare of Japan 2013a, b). Where several physicians or nurses were working in a single facility, they were asked to discuss the questionnaire together and have one person respond on behalf of the group.
Approval for the study was obtained from the Ethical Committee of the Life Science Committee at The University of Tokyo (Approval numbers: 12-91, 13-77).
QuestionnairesThe questionnaire contained questions intended for two studies; one is the present study and the other a study for the structure of catheter replacement services in home medical settings and the regional characteristics in the same region covered in the present study (Kimura et al. 2016), and in total, contained 103 questions (16 pages) for physicians and 105 questions (16 pages) for nurses. Both physicians and nurses were asked to respond to items covering replacement of gastrostomy tubes, nasogastric tubes, tracheal cannulas, and urethral catheters for male and female patients (Center for Home Care Medicine, Faculty of Medicine, The University of Tokyo 2015). The questionnaire items were selected after discussion based on previous studies (All Japan Hospital Association 2011; Institute for Health Economics and Policy 2011; Ministry of Health, Labour and Welfare of Japan 2013a, b; Kimura et al. 2016).
Items for analysisThe principal outcome of this study was replacement of three types of devices, gastrostomy tubes, nasogastric tubes and tracheal cannulas. Participants answered “Yes” or “No” to whether they provided replacements during home medical care. Participants were also asked whether physicians or nurses replaced urethral catheters for male and female patients, in principle.
The questionnaire covered participants’ sex, and years’ experience of home-visit care. To test the study hypothesis, the questionnaire also asked about the participant’s clinic base, including the number of full-time equivalent physicians (rounding the number off to one decimal place), registration status as a home-care support clinic (“not registered”, “registered as an independent clinic”, and “registered as a cooperative clinic”) and the number of receipts (statements of medical expenses) related to home medical care (for health insurance) issued in the previous month. Nursing stations were asked to specify the number of full-time equivalent nurses (to one decimal place), the status of the additional reimbursement system used for 24-hour support systems (“not applied”, “24-hour emergency contact system”, and “24-hour care system”) and the number of receipts (statements of medical expenses) related to home medical care (for health insurance) issued in the previous month. A regional ID number was assigned on a municipal basis to each questionnaire to identify the respondents’ region.
The device replacement service system is likely to be influenced by the medical resources and demand for services in the region. We therefore included the number of clinics and nursing stations and the regional population ratio of older people as variables (Kimura el al. 2016). We considered that device replacement at home could be associated with the device delivery structure or medical resources in that region. We therefore evaluated replacement status using the numbers of clinics and nursing stations per 100,000 population.
We used data from the Ministry of Health, Labour and Welfare (2013a) to determine the number of clinics per 100,000 population on a municipal basis. The number of nursing stations per 100,000 population is not published, so we used the number of nursing stations in each region divided by the population of the region, then multiplied by 100,000 to obtain the number of stations per 100,000 population (Ministry of Health, Labour and Welfare of Japan 2013b).
We also considered that device replacement during home medical care could be associated with demand, or the number of patients who needed device replacement in each region. This was evaluated using the ratio of the population aged ≥ 65 years. We obtained the ratio of the population aged ≥ 65 years in the region on a municipal basis from the most recent National Population Census data (Ministry of Internal Affairs and Communications of Japan 2010).
Data analysisFor rates of replacement of gastrostomy tubes, nasogastric tubes and tracheal cannulas, we divided the numbers of physicians and nurses who responded “Yes, I have replaced it” for each question by the total number of respondents.
For replacement of urethral catheters, we analyzed the professions of those who usually replaced urethral catheters for male and female patients. The numbers who indicated that this task was done in principle by a physician or by a nurse were divided by the total number of respondents for each.
A univariate analysis was conducted for physicians using as variables sex, years of home medical care experience, the number of full-time physicians, the clinic’s registration status, the number of monthly receipts, the number of clinics, the number of nursing stations, and the ratio of the population aged ≥ 65 years.
A second univariate analysis was conducted for nurses using as variables sex, years of home-visit care experience, the number of full-time nurses, the status of the additional reimbursement system used for 24-hour support, the number of monthly receipts, the number of clinics, the number of nursing stations, and the ratio of the population aged ≥ 65 years. For both analyses, only data with no missing values were used for each of the variables.
Next, multivariable analyses were conducted to extract the factors associated with physicians replacing each device (gastrostomy tubes, nasogastric tubes, tracheal cannulas, and urethral catheters for male and female patients). The variables used in Physician Model 1 were sex, years of home medical care experience, the number of full-time physicians, the clinic’s registration status, and the number of monthly receipts. For Physician Model 2, we also added the number of clinics, the number of nursing stations, and the ratio of the population aged ≥ 65 years.
Multivariable analyses were also used to extract the factors associated with nurses replacing each type of device (gastrostomy tubes, nasogastric tubes, tracheal cannulas, and urethral catheters for male and female patients). The variables used in Nurse Model 1 were sex, years of home-visit care experience, the number of full-time physicians, the status of the additional reimbursement system used for 24-hour support, and the number of monthly receipts. Nurse Model 2 added the number of clinics, the number of nursing stations, and the ratio of the population aged ≥ 65 years. All statistical analyses were conducted using SPSS for Windows Version 20.0 (IBM SPSS Statistics for Windows, Version 20.0., IBM Corp., Armonk, NY, USA), with a significance level of 5%.
Of the 5,828 clinics that provided home medical care, 173 were excluded as the questionnaires could not be delivered. Responses were received from 933 (16.5%) of the 5,655 clinics that received questionnaires. The number of responses with no missing data was 619 (Fig. 1).
Of the 1,798 home-visit nursing stations, 1,764 received the questionnaires (excluding 34 to which the questionnaires were undeliverable), and responses were received from 552 (31.3%). The number of responses with no missing data was 427 (Fig. 2).
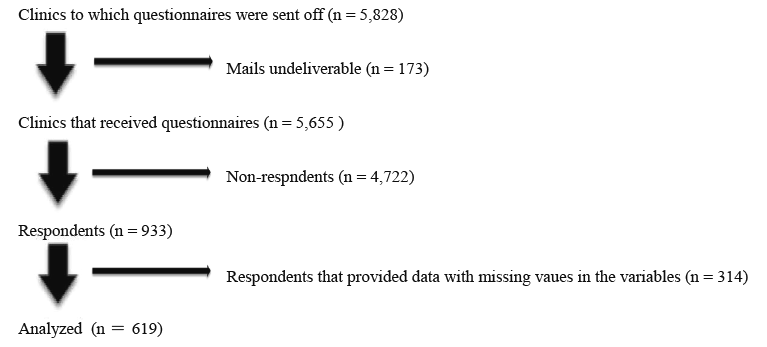
Flow diagram for participation of clinics (process and exclusion reasons).

Flow diagram for participation of home-visit nursing stations (process and exclusion reasons).
The mean age (± standard deviation [SD]) was 55 ± 10 years for physicians and 49 ± 8 years for nurses. In total, 552 physicians were male (89.2%) and 67 were female (10.8%); 417 nurses were female (97.7%) and 10 were male (2.3%). Physicians reported 13 ± 8 years of experience of home-visit care, and nurses reported 10 ± 6 years of experience.
There were 1.8 ± 2.2 full-time equivalent physicians in each clinic and 4.8 ± 2.5 nurses per station. The number of receipts for home medical or nursing care issued in the previous month was 117 ± 231 for physicians, and 203 ± 260 for nurses. In total, 185 clinics (29.9%) had not applied for registration as a home-care support clinic, 230 clinics (37.2%) were registered as an independent clinic, and 204 (33.0%) were registered as a cooperative clinic. In total, 58 stations (13.6%) had not applied for the additional reimbursement system used for 24-hour support systems, 39 (9.1%) were registered as qualified facilities with a 24-hour emergency contact system, and 330 (77.3%) were registered as qualified facilities with a 24-hour care system.
Device replacement structure in home settingsIn total, 287 physicians (46.4%) and 35 nurses (8.2%) had replaced gastrostomy tubes. Similar numbers of physicians (275, or 44.4%) had replaced nasogastric tubes, with 174 nurses (40.7%) saying that they had done so. Tracheal cannulas had been replaced by 330 physicians (53.3%) and 50 nurses (11.7%).
For the question to the physicians on urethral cannula replacement in male patients, 460 physicians (74.3%) replied that the device had been replaced by physicians in principle and 159 (25.7%) answered that the replacement had been done by nurses in principle. For the same question to the nurses, 126 nurses (29.5%) replied that the device had been replaced by nurses in principle and 301 (70.5%) answered that the replacement had been carried out by physicians in principle. On the other hand, for the question to the physicians on urethral replacement in female patients, 103 physicians (16.6%) replied that the device had been replaced by physicians in principle and 516 (83.4%) answered that the replacement had been done by nurses in principle. For the same question to the nurses, 412 nurses (96.5%) replied that the device had been replaced by nurses in principle and only 15 (3.5%) answered that the replacement had been carried out by physicians in principle.
Characteristics of regions where clinics and stations are locatedThe mean number (± SD) of clinics per 100,000 population in the regions with responding clinics was 82.0 ± 67.1, and the median was 69.7. The mean number (± SD) of home-visit nursing stations per 100,000 population in responding regions was 5.1 ± 2.74, and the median was 4.7. The mean ratio (± SD) of population aged 65 years or older per 100,000 population in the regions with responding clinics and stations was 21.0 ± 3.6%, and the median was 20.4%.
Associations between device replacement and patient and regional characteristicsTable 1 shows the patient and regional characteristics and the results of univariate and multivariable analyses for gastrostomy tube replacement. In the univariate analysis, gastrostomy tube replacement by physicians was significantly associated with a larger number of physicians, and independent and cooperative clinic registrations. In the multivariable analysis for Model 1, gastrostomy tube replacement by physicians was significantly associated with larger numbers of physicians, male doctors, and independent and cooperative clinics. In the multivariable analysis for Model 2, gastrostomy tube replacement by physicians was significantly associated with all the previous factors plus frequent home-visit nursing. However, a larger number of clinics was significantly associated with the finding that gastrostomy tubes were not replaced.
No factors were significantly associated with gastrostomy tube replacement by nurses in either univariate- and multivariable analyses.
Table 2 shows the patient and regional characteristics and the results of univariate and multivariable analyses for nasogastric tube replacement. In the univariate analysis, nasogastric tube replacement by physicians was significantly associated with a larger number of receipts, and independent and cooperative clinics. In the multivariable analysis for Models 1 and 2, nasogastric tube replacement by physicians was significantly associated with more experience of home-visit medical care, as well as independent and cooperative clinics.
In the univariate analysis, nasogastric tube replacement by nurses was significantly associated with greater experience of home-visit care and fewer nursing stations. In the multivariable analyses for Model 1, nasogastric tube replacement by nurses was significantly associated with greater experience of home-visit care. Using Model 2, the replacement was significantly associated with greater experience of home-visit care and higher population ratios aged ≧ 65 years.
Table 3 shows the patient and regional characteristics and the results of univariate and multivariable analyses of tracheal cannula replacement. In the univariate analysis, tracheal cannula replacement by physicians was significantly associated with greater numbers of receipts and physicians and with independent and cooperative clinic status. In the multivariable analysis for Model 1, tracheal cannula replacement by physicians was significantly associated with greater experience of home-visit medical care, more physicians, and independent and cooperative clinic status. In the multivariable analysis for Model 2, tracheal cannula replacement by physicians was significantly associated with all these factors plus more clinics.
In the univariate analysis, tracheal cannula replacement by nurses was significantly associated with greater experience of home-visit care. In the multivariable analysis for Model 1, it was significantly associated with greater experience of home-visit care and female nurses. In the multivariable analysis for Model 2, the replacement was significantly associated with greater experience of home-visit care.
Table 4 shows the patient and regional characteristics and the results of univariate and multivariable analyses of urethral catheter replacement in male patients. In the univariate analysis, urethral catheter replacement by physicians in male patients was significantly associated with the ratio of the population aged ≧ 65 years being high. Larger numbers of clinics and home-visit nursing stations were significantly associated with urethral catheters not being replaced. In the multivariable analysis for Model 1, there were no factors with significant associations. In the multivariable analysis for Model 2, a larger number of clinics and higher ratio of the population aged ≧ 65 years were significantly associated with urethral catheters not being replaced.
In the univariate analysis, urethral catheter replacement in male patients by nurses was significantly associated with greater number of receipts and the availability of a 24-hour care service system. A larger number of clinics was significantly associated with urethral catheters not being replaced. In the multivariable analysis for Models 1 and 2, urethral catheter replacement by nurses was significantly associated with the same factors.
Table 5 shows the patient and regional characteristics and the results of univariate and multivariable analyses of urethral catheter replacement in female patients. In the univariate analysis, urethral catheter replacement in female patients by physicians was significantly associated with greater numbers of receipts and physicians. More experience of home-visit medical care and more clinics were significantly associated with urethral catheters not being replaced. In the multivariable analysis for Model 1, the replacement was significantly associated with greater numbers of receipts. More experience of home-visit medical care was significantly associated with urethral catheters not being replaced. In the multivariable analysis for Model 2, longer experience of home-visit medical care and more clinics were significantly associated with urethral catheters not being replaced.
In the univariate analysis, a higher ratio of the population of ≥ 65 years was significantly associated with urethral catheters not being replaced in female patients by nurses. In the multivariable analysis, there were no factors significantly associated with replacement by nurses in either Models 1 or 2.

Factors associated with gastrostomy tube replacement.
*OR ≥ 1 indicates gastrostomy tube replacement are more frequent.
CI = confidence interval.

Factors associated with nasogastric tube replacement.
*OR ≥ 1 indicates nasogastric tube replacement are more frequent.
CI = confidence interval.

Factors associated with tracheal cannula replacement.
*OR ≥ 1 indicates tracheal cannula replacement are more frequent.
CI = confidence interval.
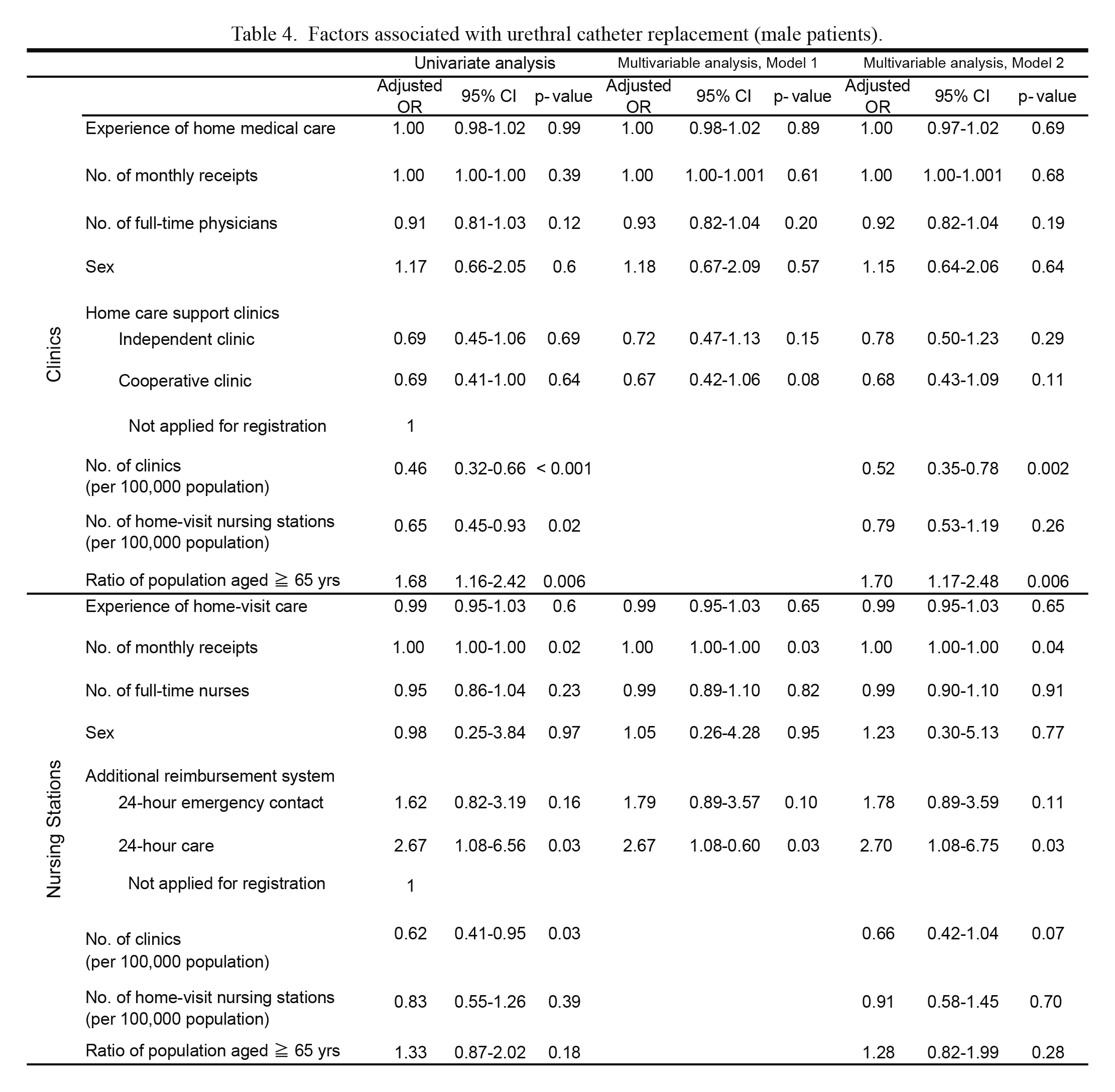
Factors associated with urethral catheter replacement (male patients).
*OR ≥ 1 indicates urethral catheter replacement (male patients) are more frequent.
CI = confidence interval.

Factors associated with urethral catheter replacement (female patients).
*OR ≥ 1 indicates urethral catheter replacement (female patients) are more frequent.
CI = confidence interval.
This study examined background factors of physicians and nurses who had replaced medical devices in home settings.
Gastrostomy tube replacementGastrostomy tubes had been replaced more frequently by physicians when there were more physicians working at the clinic and the facility was registered as an independent or cooperative clinic in both models in the multivariable analyses. In other words, those who had replaced gastrostomy tubes were more likely to be physicians working in larger groups in clinics providing 24-hour care services. This indicates that a 24-hour support system is required to replace gastrostomy tubes which are accidentally removed outside normal surgery hours, and that a system involving more than one physician is required for this provision.
Nasogastric tube replacementPhysicians with more experience of home-visit medical care were more likely to have replaced nasogastric tubes more frequently. Other associated factors were a greater number of physicians and the facility being registered as an independent or cooperative clinic in both models in the multivariable analyses. This suggested that those who had replaced nasogastric tubes were physicians with a certain level of home-visit medical care experience and working in clinics providing 24-hour support services using multiple physicians. This is similar to gastrostomy tube replacement.
Nasogastric tube replacement by nurses was more frequent with greater experience of home-visit medical care in both models in the multivariable analyses. It was also more likely to happen when the ratio of the population aged ≧ 65 years was high, suggesting a possibility that nasogastric tube replacement by nurses in high demand areas had been conducted in cooperation with physicians.
Tracheal cannula replacementPhysicians were more likely to replace tracheal cannulas when they had greater experience of home-visit medical care, there were more physicians employed at the clinic and the facility was registered as an independent or cooperative clinic, in both models in the multivariable analyses. Again, this suggests that a certain level of experience is required to be able to replace tracheal cannulas, and that these physicians worked in clinics providing 24-hour care services. This may suggest that replacement is more likely to be necessary in an emergency (Center for Home Care Medicine, Faculty of Medicine, The University of Tokyo 2015). Nurses had replaced tracheal cannulas more frequently when they had more experience of home-visit medical care in both models in the multivariable analyses.
Urethral catheter replacement (male patients)More than 80% of physicians and nurses answered that physicians were more likely to replace urethral catheters in male patients. The multivariable analyses in both models suggested that nurses were more likely to have carried out replacement if they worked in home-visit nursing stations with larger numbers of monthly receipts and a 24-hour care service system. This suggests that in larger nursing stations, with more patients and providing 24-hour care services, nurses replace urethral catheters in male patients in cooperation with physicians.
Urethral catheter replacement (female patients)More than 80% of both physicians and nurses answered that nurses were more likely to replace urethral catheters in female patients. The multivariable analyses in Models 1 and 2 showed that physicians were more likely to carry out replacement when they worked in larger clinics, with more monthly receipts. We suggest that physicians in these larger clinics may replace urethral catheters in female patients in cooperation with nurses. Physicians were less likely to have replaced catheters frequently when they had more experience of home-visit medical care. The reason for that is unknown, but it may be that these physicians had delegated the replacement to nurses. Further research is necessary to explore this.
Relationship between device replacement and the number of staff in clinics/nursing stations, and a 24-hour care service systemGastrostomy tubes and tracheal cannulas were more frequently replaced by physicians when there were more staff at the clinic. We suggest that in home medical care settings, group clinics are able to replace gastrostomy tubes and tracheal cannulas more actively than single-handed clinics. It may be helpful for single-handed and group clinics to discuss cooperating over device replacement, to reduce the burden on the former. For nurses, the number of staff did not seem to affect frequency of device replacement. In Japan, home-visit nursing stations all meet minimum headcount requirements of at least 2.5 full-time equivalent nurses, and our findings suggest that this headcount is adequate (Ministry of Health, Labour and Welfare of Japan 2013b).
Where clinics provide 24-hour support services, gastrostomy tubes, nasogastric tubes and tracheal cannulas were all more likely to have been replaced by physicians. This suggests that physicians may be fully aware that they are obliged to make an emergency visit to patients in case of accidental removal of devices. Among nurses, only urethral catheters in male patients were more likely to have been replaced where clinics provide 24-hour care services. This was observed regardless of the number of clinics and nursing stations or the ratio of the population aged ≥ 65 years in the region. More than 80% of both physicians and nurses answered that physicians would normally replace urethral catheters in male patients. It may be, therefore, that nursing stations providing 24-hour support services only carried out urethral catheter replacement in male patients as an emergency, following accidental removal of catheters.
Study limitationsFirst, the results of this study are based on the subjective views of the participants; the actual structure of device replacement may differ from the responses. Second, the reliability and validity of the questionnaire was limited. Future studies should survey individual patients to check the reality of device replacement by physicians and nurses.
Third, the response rate of this survey was low; 16.5% in clinics and 31.3% in home-visit nursing stations. It is reported that in Japan the average response rate is 21.3% in mail-in and unpaid surveys without reminder like the present study (Hagihara et al. 2006), and that might give a hint to the reason for the low response rate in physicians. On the other hand, there is a report that the response rate was less than 15% (Kenzaka et al. 2016) and, therefore, the response rate of the present study is considered to represent physicians above a certain level.
In home medical care settings, the replacement of gastrostomy tubes and tracheal cannulas by physicians was associated with greater number of staff and provision of 24-hour medical care services, including emergency visits. It may, therefore, be necessary to discuss cooperation for device replacement in home medical care settings, particularly between single-handed and group clinics.
We are grateful to all physicians and nurses involved in this study for their cooperation.
The authors declare no conflict of interest.