2017 年 242 巻 3 号 p. 215-221
2017 年 242 巻 3 号 p. 215-221
Obesity is a major risk factor of cardiovascular, osteoarthritis, metabolic and pulmonary disorders, and exercise is an efficient method for treating obesity. However, obese patients often complain of dyspnea on exertion, which makes it difficult to continue exercise program. Obesity is also known to have an adverse effect on pulmonary function. The purpose of this study was to examine the effects of a comprehensive obesity rehabilitation (COR) program on pulmonary function in Japanese patients with morbid obesity. We enrolled 29 Japanese obese patients (14 males and 15 females) with BMI > 29 and an average age of 42.2 ± 11.7 years, who underwent the COR program for 1-3 months. Our COR program included a calorie-restricted diet, nutritional counseling, exercise training, and health education. We focused on the changes in pulmonary function, anticipating that changes in ventilation volume may contribute to improving exercise tolerance. After the intervention, all the subjects had lost weight, with a mean value of 12.0 kg (P < 0.001). We found that the lung volume compartment was significantly increased after our COR program, and that there is a strong positive correlation between a change in expiratory reserve volume and the weight loss (r = 0.74, P < 0.01). Through the COR program, body fat mass was significantly reduced, while the skeletal muscle mass remained more or less unchanged, which is advantageous for improvement in exercise tolerance. In conclusion, our COR program is helpful to improve the pulmonary function of patients with obesity.
Obesity is the most common metabolic disease in the world, and the prevalence of obesity with BMI ≥ 25 is approximately 20-30% in Japan. Obesity is also known to be a major risk factor of cardiovascular, osteoarthritis, metabolic and pulmonary disorders. Therefore, it is of utmost importance not only for obese patients themselves but also for our society to establish an efficient method for treating obesity.
Obesity is known to have an adverse effect on pulmonary function, such as an increase in labored breathing (Sood 2009) and reduction in total respiratory system compliance and lung volumes (Naimark and Cherniack 1960; Pelosi et al. 1996; Salome et al. 2010). In particular, a reduction in expiratory reserve volume (ERV: the maximum volume of air that can be exhaled from the end-expiratory tidal position) is considered to be closely related to the degree of obesity (Littleton 2012; Brazzale et al. 2015).
In the field of rehabilitation, comprehensive rehabilitation composed of nutritional intervention, exercise, and education has recently attracted considerable attention as a treatment for obesity. While exercise is known to be effective for improving insulin resistance (Bloem and Chang 2008), a few studies have evaluated the changes in pulmonary function after exercise- and diet-induced weight loss (Babb et al. 2011; Mafort et al. 2016). Bariatric surgery is also considered to be an effective option for weight loss, especially for morbidly obese patients. Some studies have shown an improvement of pulmonary function after bariatric surgery (Thomas et al. 1989; El-Gamal et al. 2005). However, the surgical option is associated with several problems, including surgical complications, anemia, and decrease in muscle mass and bone density (Center and White 2013).
In this study, we examined the effects of a comprehensive obesity rehabilitation (COR) program on pulmonary function in patients with morbid obesity. Our COR program included a calorie-restricted diet, nutritional counseling, exercise training, and health education. Since exercise tolerance is partly determined by pulmonary function, we focused on changes in pulmonary function, anticipating that changes in ventilation volume may contribute to improving exercise tolerance.
In this study, we enrolled twenty-nine Japanese obese patients admitted to our hospital for the treatment of obesity and they underwent a COR program for 1-3 months. We measured body weight, biochemical measurements and pulmonary function at the beginning and end of the COR program.
SubjectsParticipants included patients who were referred to our department for the purpose of weight reduction from November 2011 to September 2015 at Tohoku University Hospital. 29 Japanese obese patients (14 males and 15 females) with an average age of 42.2 ± 11.7 years (range, 23 to 65 years), an average body weight of 118.7 ± 39.3 kg, and an average BMI of 43.8 ± 11.5 kg/m2 were enrolled as subjects. The primary criterion for participation was being overweight, which was defined by a BMI > 29.0. Exclusion criteria were smoker, pregnancy, or musculoskeletal abnormalities.
Weight loss interventionAll participants were admitted to our hospital for the treatment of obesity and underwent a COR program, which involved reduced-calorie diets, nutritional counseling, walking with a pedometer, health education, and physical exercise under the supervision of a physiotherapist. Our COR program is based on our already established cardiac rehabilitation program which includes exercise training and health education. In order to apply the program to patients with morbid obesity, we added a calorie-restricted diet, increased the number of nutritional counseling, changed the contents of health education for obese patients (e.g., complication of obesity, risk factor modification, physical exercise, management of diet, weight control and self-management) and optimized the amount and strength of exercise depending on the status of each patient.
This COR program is routinely used in our department, and our program includes only non-invasive examination.
The diet was set at 25-30 kcal per body weight for each patient and adjusted while observing changes in weight, examination value, and exercise amount. Nutritional counseling was conducted individually by a registered dietitian for 60 minutes. Additionally, before and after home exercise, doctors and nutritionists conducted nutritional guidance individually. Regarding health education, doctors lectured patients and their families about complications of obesity, arteriosclerosis and risk factors, physical exercise, and diet management while taking account of individual conditions. The exercise protocol consisted of stretching, aerobic exercise on a bicycle ergometer or treadmill for 80 minutes (40 minutes in the morning and afternoon) five times per week, and moderate-intensity resistance training five times per week on a specified menu. Moreover, a self-walking exercise with a pedometer aimed at achieving approximately 7,000 steps every day. Each patient recorded his/her step counts, body pressure, pulse rate, and body weight on a recording paper. However, patients with knee pain or morbid obesity utilized an underwater treadmill as an aerobic exercise. The aerobic exercise intensity was determined by cardiopulmonary exercise testing. The duration of hospitalization was determined by the time when each patient became able to self-manage, and the average duration is about two months.
Body composition and metabolic evaluationsHeight was measured by a stadiometer at baseline. Body weight was measured everyday using a calibrated standard balance scale and body mass index was calculated as weight (kg)/height (m2). Biochemical measurements were followed before and after intervention. Body composition and waist-to-hip ratio at baseline and follow-up were measured by using bioelectrical impedance analysis (In Body S20, Kobe Medicare, Kobe, Japan). Among the above-mentioned measurements, the complete data of body composition and the waist-to-hip ratio was available for 23 and 20 patients, respectively, which we used in our analysis.
Pulmonary functionSpirometric tests were performed before and after the COR program using a CHESTAC 8900 (Chest, Tokyo, Japan).
Statistical analysisAll values were expressed as means ± SD. The statistical significance of the post-intervention effect was assessed by a paired student t-test. Correlations between variables were tested by the Pearson correlation coefficient. A P value less than 0.05 was considered statistically significant.
The baseline characteristics of the subjects are summarized in Table 1. The mean BMI was 43.8 ± 11.5 kg/m2. A biochemical test revealed high levels of liver transaminase, lipid parameter, blood glucose, hemoglobin A1c (HbA1c), and C-reactive protein (CRP).
By 1-3 months after the intervention, all the subjects had lost weight, with a mean value of 12.0 kg. The mean BMI decreased from 43.8 kg/m2 to 39.5 kg/m2. The mean body fat mass percentage decreased from 47.8% to 44.9%. Fat mass and fat mass percentage were significantly reduced compared to skeletal muscle mass (Table 2). The values for low-density lipoprotein cholesterol, uric acid, HbA1c and CRP were consistently reduced by the intervention, whereas high-density lipoprotein cholesterol did not improve (Table 2).

Baseline characteristics.
Values are expressed as the number (percentage) of patients or mean ± S D.
Hb, hemoglobin; AST, aspartate aminotransferase; ALT, alanine aminotransferase; Cr, creatinine; HbA1c, hemoglobin A1c; CRP, C-reactive protein.

Changes in body composition and biochemical measurements after weight loss.
Values are expressed as mean ± SD. *P < 0.05.
Hb, hemoglobin; AST, aspartate aminotransferase; ALT, alanine aminotransferase;
Cr, creatinine; HbA1c, hemoglobin A1c; CRP, C-reactive protein.
Lung volume: The main changes in lung volumes are summarized in Table 3, where the listed values are for male, female and total subjects from top to bottom in each item. In the following, we mainly analyze the total subjects unless stated otherwise.
Before we started the intervention, both ERV and functional residual capacity (FRC) of all the patients were lower than the predicted values. In particular, ERV was only 47.6 ± 25.4% of predicted.
Vital capacity (VC), ERV, FRC increased significantly (P < 0.001) after weight loss. Inspiratory capacity (IC) did not change after weight loss. There was no significant change in residual volume (RV), but the total lung capacity (TLC) increased significantly (P < 0.01) and the RV/TLC ratio improved (P = 0.001). While there was no significant difference between males and females, the improvement was slightly greater for males than females.
We found a positive correlation between the improvement in ERV (r = 0.74, P < 0.01), VC (r = 0.65, P < 0.01), FRC (r = 0.62, P < 0.01), TLC (r = 0.68, P < 0.01), and weight loss (Fig. 1).
Flow-volume curve: Before we started the intervention, forced expiratory volume in one second (FEV1.0), % FEV1.0, and forced vital capacity (FVC) were reduced while FEV1.0/FVC (%) was preserved within the normal range (Table 4). The baseline maximum expiratory flow at 50% of FEV (V50), maximum expiratory flow at 25% of FEV (V25), %V25/HT were reduced while the V50/ V25 ratio was increased (Table 4).
FEV1.0 and, % FEV1.0 increased significantly (P < 0.001) and % V25/HT and, V50/ V25 ratio improved after weight loss (P < 0.01 and P < 0.05, respectively). Inspecting more closely, the improvement of V50/ V25 was greater for females than males. There was no significant change in peak expiratory flow (PEF). We found a positive correlation between the changes in FEV1.0 and VC, and TLC and V25 (Fig. 2).
After the intervention, two of the patients were admitted to our hospital again due to a weight increase. We examined the spirometry values of the two patients and found that ERV had decreased from those values measured at the end of the first intervention. This implies that there was a negative correlation between ERV and change in body weight.

Lung volume before and after weight loss.
Various lung volumes for male, female, and total (shown in bold) from top to bottom in each item. Values are expressed as mean ± SD. *P < 0.05.
VC, vital capacity; IC, inspiratory capacity; ERV, expiratory reserve volume; FRC, functional residual capacity; RV, residual volume; TLC, total lung capacity.

Correlation of the changes in lung volume and body weight reduction.
Shown are correlations between changes in body weight reduction and lung volume, namely, VC (A), ERV (B), FRC (C), and TLC (D). Correlations between these variables were tested by the Pearson correlation coefficient.
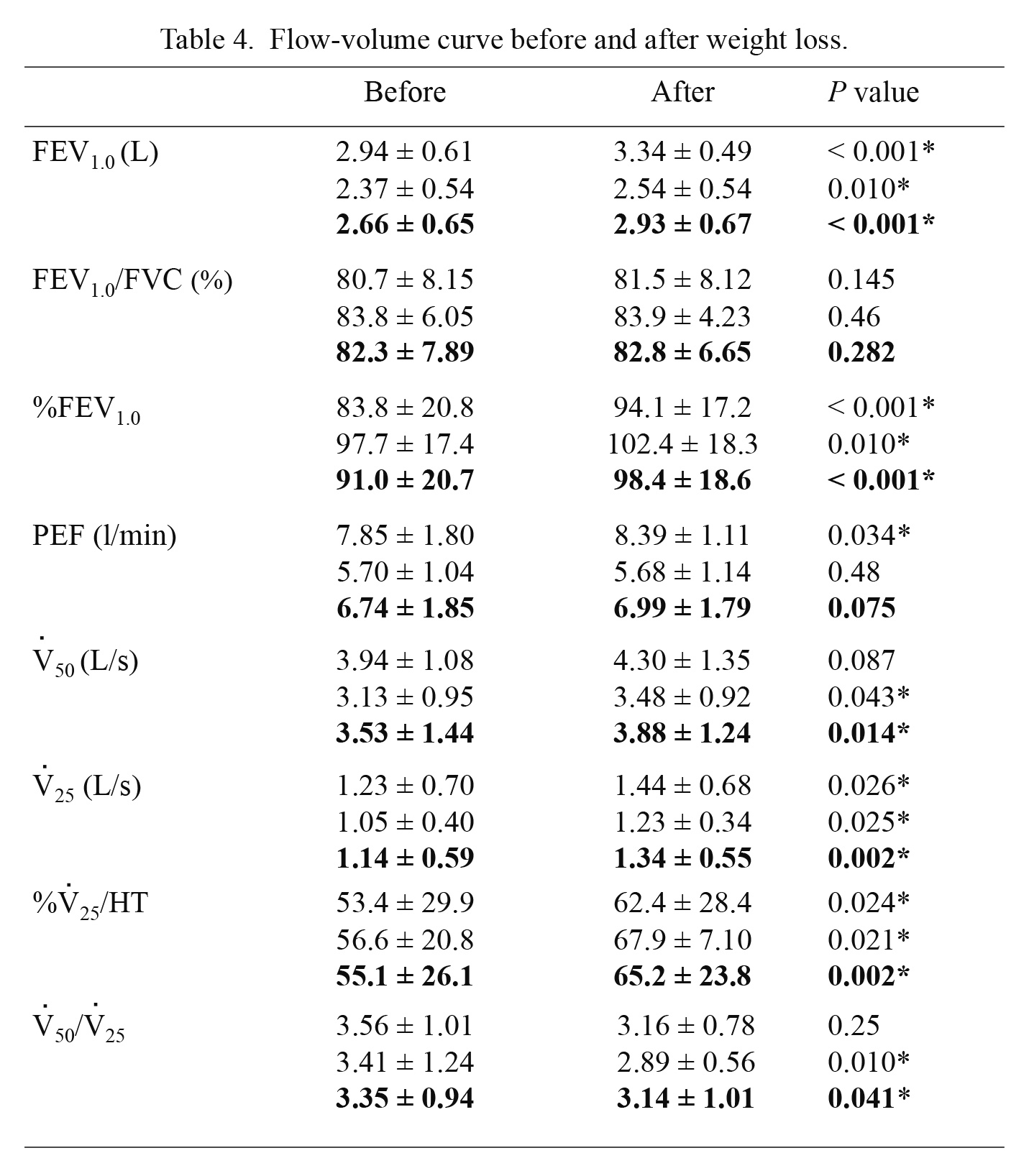
Flow-volume curve before and after weight loss.
Various flow volume curve for male, female, and total (shown in bold) from top to bottom in each item. Values are expressed as mean ± SD. *P < 0.05.
FEV1.0, forced expiratory volume in one second; FVC, forced vital capacity; PEF, peak expiratory flow; V50, maximum expiratory flow at 50% of FEV; V25, maximum expiratory flow at 25% of FEV.

Correlation between changes in pulmonary functions.
Shown are correlations between changes in various pulmonary fucntions in VC and ERV (A), VC and FEV1.0 (B), and TLC and V25 (C).
Obesity is known to cause impairments in pulmonary function. In particular, it affects the lung volume leading to a decrease in ERV (Littleton 2012; Brazzale et al. 2015). There are several reports on the improvement of ERV after weight loss by bariatric surgery (Thomas et al. 1989), a calorie restricted diet (Hakala et al. 1995), and intragastric balloon therapy (Mafort et al. 2014). However, to the best of our knowledge, there are few reports of studies that conducted a comprehensive weight loss program that included exercise (Babb et al. 2011; Littleton 2012). Our COR program consisted of reduced-calorie diets, nutritional counseling, health education, and physical exercise. It is worth investigating if this comprehensive program has advantages over other methods in improving pulmonary function test results. The purpose of this study was to examine the effects of our COR program on the pulmonary function tests of obese patients. We have also studied if there is any correlation between changes in pulmonary function and body weight reduction.
In this study, we found that the lung volumes (VC, ERV, FRC, TLC) of 29 patients were significantly improved (P < 0.001-0.01) after our COR program. In particular, we found that there is a strong positive correlation between a change in ERV and weight loss.
In general, ERV can be improved by various factors such as weight loss, increase in respiratory muscles, and improvement of lung thorax compliance. In our study, the weight loss is considered to be the major reason for the improvement in ERV as we did not perform any training specialized for respiratory muscles.
More specifically, a change in the fat distribution may be an important factor for an improvement in ERV. Since there is a correlation between lung volumes and the upper body fat distribution with a waist-to-hip ratio > 0.95 (Collins et al. 1995), an improvement in ERV after weight loss may be closely related to a decrease of abdominal visceral adipose tissue. We have found that waist-to-hip ratio decreased after the COR program (P = 0.006), with a rather strong correlation between changes in ERV and waist-to-hip ratio (r = 0.60, P < 0.01). This may be attributed to an improvement of diaphragmatic excursion by a decrease in abdominal visceral adipose tissue. Therefore, our study suggests that not only the total weight loss, but also the decrease in abdominal visceral adipose tissue, contributes to an improvement in ERV.
We noted that while FEV1.0 increased after weight loss, FEV1.0/FVC was more or less maintained. We also found a positive correlation between a change of FEV1.0 and VC. This indicates that an improvement in FEV1.0 is mainly due to a change in the lung volume, and if so, it does not necessarily represent an improvement in airway obstruction. It is therefore customary either to normalize the expiratory flows with respect to the lung volume or to calculate their ratio to cancel the effect of lung volume changes. In this study, we focused on the ratio of V50/ V25 since V25 is considered to be more sensitive to a peripheral airway obstruction. We found that the ratio of V50/ V25 improved after weight loss (P = 0.041). Although we also found a positive correlation between V25 and the lung volume, the variance was large. This implies that the peripheral airway obstruction is caused by not only the reduced lung volume but also other factors such as the premature closure of the inflamed and edematous small airway induced by proinflammatory adipokines (Sood 2009).
There are several reports on the effect of a bariatric surgery on respiratory function. For instance, a study by Thomas et al. (1989) found that lung functions such as ERV, FRC, RV and TLC of morbidly obese patients significantly improved after weight loss due to the surgery. This may support the view that pulmonary function is related to weight loss. However, it is worth noting that while the study by Thomas et al. (1989) found no correlation between weight loss and lung volumes, we found a rather strong correlation between the two in our COR program. This may imply that our COR program with exercise has a more consistent effect on the improvement of lung function compared to bariatric surgery.
In our COR program with exercise, we have found that it is possible to predominantly reduce the body fat mass, while the skeletal muscle mass remains more or less intact (Table 2). The maintenance of muscle mass may be important for the improvement of lung function, as it is known that a reduction in respiratory muscles occurs in pathological conditions such as sarcopenia and cachexia (Dudgeon and Baracos 2016). Therefore, the maintenance of the skeletal muscle mass during weight loss is one of the advantages of our COR program.
One of the limitations of our study is the number of cases, which did not allow us to fully analyze the dependence of our results on other factors such as sex difference. In addition, due to the comprehensive nature of our program, it is difficult to determine which of the factors are most important. Collecting more detailed data will enable us to identify the most important factors and clarify their dependence and effects of age difference, lean body mass, fat distribution, and respiratory muscle strength. We also notice that, for some of the patients, there is no improvement in lung volumes as expected from their weight loss. A dedicated analysis is certainly necessary to understand those outliers. Further, rebound cases were also present, and further study is warranted to determine if our COR program is effective in weight loss for a longer term. By doing so, we would be able to optimize our COR program toward an efficient treatment of obesity that improves exercise capacity and respiratory function on firm ground.
This work was supported by JSPS KAKENHI Grant Number 15K16350 and 15K12588.
We would like to thank Editage for English language editing.
The authors declare no conflict of interest.