2017 Volume 243 Issue 1 Pages 67-75
2017 Volume 243 Issue 1 Pages 67-75
People living with HIV or AIDS (PLWHA) experienced severe medical discrimination which is seriously affecting their lives. However, few studies examined the epidemic characteristics of self-perceived medical discrimination from the discrimination objects such as PLWHA. Therefore, we aimed to investigate the epidemiological status and analyze the influential factors of the self-perceived medical discrimination on PLWHA in South China. The self-designed questionnaire was used to investigate the medical discrimination status of the 443 infected persons, who were randomly recruited from the representative AIDS designated hospitals in Guangdong Province in South China. The results showed that 49.0% of PLWHA experienced medical discrimination, and 55.3% received discriminatory treatment, 48.4% experienced refusal of treatment, 36.4% had private information leaked and 12.9% received mandatory test. However, 52.2% patients chose to endure discrimination in silence. Compared with the Asymptomatic HIV-infected patients, AIDS patients perceived more medical discrimination. The Logistic regression analysis indicated that PLWHA self-perceived medical discrimination status was influenced by 4 factors: the voluntary of first medical detection, the route of transmission, the stage of the disease and the familiarity with the HIV/AIDS-related law. Additionally, the two dimensions of the life quality scale were influenced by medical discrimination, namely, overall function and disclosure worry. Ultimately, our study provides a better understanding of the relationship between infection status, quality of life and the medical discrimination they experienced or perceived. It will help health professionals and policy makers to develop tailored behavioral and policy-oriented intervention strategies for PLWHA to tackle different types of medical discrimination in high-risk settings.
After the first case of Acquired Immune Deficiency Syndrome (AIDS) was identified in 1981, China confronts a rampant AIDS epidemic (Wang 2007). Up to now, the epidemic situation is still grim (Guo et al. 2017). Additionally, people living with HIV or AIDS (PLWHA) have become the most vulnerable crowd to be discriminated in the world (Simbayi et al. 2007). One study showed that 73% of participants thought it shameful to have HIV (Sullivan et al. 2010). Due to its infectiousness, incurability and dangerous lifestyle (men having sex with men, injecting illegal drugs and having commercial sex), the crowd gradually alienated them. So far, no effective cure for PLWHA has been found. One of the most important challenges in successfully controlling the spread of HIV is mainly to control the discrimination (Abdool Karim 2013).
AIDS-related discrimination mainly occurs on three areas: social and community area, medical and health work area and personal perception, and the discrimination also include three types: perceived discrimination, internalized discrimination and associated discrimination (Phillips et al. 2011). Perceived discrimination, also called self-discrimination, is an individual’s subjective awareness of discriminatory and prejudicial attitudes from people around them (Phillips et al. 2011). In the medical health care field, there are several main kinds of discrimination. For example, Discriminatory Treatment (providing different treatment compared with other similar symptoms), Refusal of Treatment (refusing to provide medical services on the grounds of the person having AIDS), Leaking Privacy (revealing infector’s private information to the public or their family members), and Mandatory Testing (testing for HIV/AIDS without the patient’s permission) (Templier et al. 2000). Therefore, self-perceived medical discrimination can be comprehended as the awareness of actual or potential social rejection from medical workers and normal people.
The existence of discrimination adversely affects AIDS control. Studies have consistently found that HIV-related discrimination can lead to a series of negative effects, causing them to end up with antiretroviral therapy, delaying access to health care, and inhibits the use of preventative services by persons at risk of HIV (Overstreet et al. 2013; Su et al. 2013). Research showed that the social support system including the medical treatment using anti-HIV drugs can prolong life expectancy and improve quality of life for PLWHA (Yadav 2010). Therefore, it is necessary to curb the HIV-related discrimination in order to promote the AIDS patients desire for, and receive antiviral treatment effectively. In most situations, because of the fear of being discriminated against, PLWHA will hide their infection status and continue to engage in high-risk behaviors, which exacerbate the spread of AIDS and leads to a worse quality of life (Makoae et al. 2008; Bharat 2011). As far as we know, the study of the medical discrimination has mainly focused on the discrimination subjects, such as the public, medical staff, school teachers and so on (Memish et al. 2015; Zarei et al. 2015). However, it is rarely aimed at the discrimination objects such as HIV/AIDS patients. We found that few articles describe the AIDS-related humiliation and discrimination from the perspective of PLWHA. Actually, self-perceived discrimination has a stronger negative impact on the overall well-being of PLWHA than public external discrimination (Kalichman 2013). Relevant investigation and intervention into self-perceived discrimination should arouse our attention. If not, this will make the experience of discrimination an imagination, not a real experience.
Now, with the AIDS epidemic, AIDS-related medical discrimination is gradually becoming a topic of concern to us. The occurrence of medical discrimination against PLWHA remains unclear. Furthermore, research about self-perceived medical discrimination in PLWHA has seldom been reported. To address this research gap, we determine to explore the current status and prevalent features of AIDS medical discrimination. In our study, we use quantitative research to discuss the distribution of medical discrimination against PLWHA in Guangdong Province, examining influential factors of medical discrimination of AIDS patients and determining which dimensions of life quality are affected by their infection characteristics so as to better describe the current situation and main problems of medical treatment discrimination for PLWHA.
A total of 443 patients with confirmed HIV or AIDS in Guangdong province, one of the strongest economic provinces and one of the areas hardly hit by the AIDS epidemic in China, were enrolled in the cross-sectional study. Based on demographic characteristics, the discrimination situation in Guangdong Province was investigated at AIDS-designated hospitals, such as the Eighth People’s Hospital of Guangzhou and the Third People’s Hospital of Shenzhen. PLWHA were eligible to participate if they were at least 12 years of age, had antiretroviral therapy at one of the designated hospitals in Guangdong Province, had no mental illness ever and had the ability to read and comprehend Chinese character.
ProceduresThe study concerning the PLWHA’s infection, quality of life and self-perceived medical discrimination from health care workers were collected using a self-administered questionnaire. Before formal investigation, 443 PLWHA who were eligible to enroll were asked to sign informed consent. The researcher verbally clarified words or sentences for participants who did not understand particular questions. The questionnaire took an average of 30 minutes to complete. Each participant was assured of data confidentiality, use of pseudonyms, safe storage of the data, and the right to withdraw at any time without being questioned. After the patients independently finished their own questionnaire, we reviewed the questionnaire on the spot, then arranged and numbered the questionnaires in real time. The investigation occurred from June to September 2016. All procedures were approved by the Ethical Committee of the Guangzhou Center for Disease Control and Prevention.
Data collectionPersonal characteristics, including gender, birthplace, educational background and marriage, were measured. The occurrence and distribution characteristics of self-perceived medical discrimination were investigated. To understand which institution, crowd or therapy section had high rates of conflict, we designed some relative issues. In addition, we identified the influencing causes and key sticking points of PLWHA’s self-perceived medical discrimination in medical treatment. Besides, Quality of life (QoL) was measured using the HIV/AIDS-targeted quality of life (HAT-QoL) instrument developed by Holmes and Shea (1998). The Cronbach’s α coefficient range of HAT-QoL scale is 0.54-0.90, with higher internal consistency and retest reliability (Holmes and Shea 1998; Holmes and Ruocco 2008). The HAT-QoL scale covers nine domains: overall function, medication concerns, disclosure worries, health worries, provider trust, financial worries, understanding of HIV, life satisfaction and sexual function. We translated the English HAT-QoL into Chinese and retranslated. Ensuring the accuracy of the translation, an analysis was made of the original version and retranslated version, and then we chose the closest version after modification. Measures are re-scaled from 0 to 100, where higher scores indicate better QoL.
Statistical analysisAfter the entire questionnaire was developed by researchers, a specialist checked the papers for a second review, and a timely coded uniform classification number was placed on the questionnaire using Epidata3.0 software for data repository. The data were transformed and entered into SPSS Version 13.0 for analysis. Descriptive statistics were conducted to obtain frequencies for categorical variables and means, standard deviations, and ranges for continuous variables. A comparison between groups was conducted to investigate the association between self-perceived medical stigma and each explanatory variable using Chi-square tests. For inferential statistics, multivariate analyses were performed on the variables of interest, and stepwise multiple logistic regressions examined possible factors associated with different types of self-perceived medical stigmatization of PLWHA and quality of life based on an including standard α (alpha) of 0.05 and exclusion criteria β (beta) of 0.10.
Four hundred forty-three PLWHA were investigated in this survey, including 396 HIV patients and 47 AIDS patients. 68.4% participants were male, and 31.6% patients were female. The average patient age was 34.46 years (S.D., 8.35 years; range, 13-67 years). Table 1 shows that 49.0% of respondents had ever suffered medical discrimination. Among these 217 PLWHA suffering medical discrimination, 55.3% were provided with treatment different from HIV/AIDS-uninfected patients with similar symptoms. It was the most common discrimination in the process of medical treatment. Additionally, 48.4% of patients were refused medical services by the medical establishment. Approximately 36.4% of patients reported that their infection situation was revealed forcibly to their sexual partners or relatives without permission. Nearly 12.9% of patients underwent mandatory testing by medical institutions. The four types of self-perceived medical discrimination in different socio-demographic characteristics are shown in Table 2. Females encountered medical discrimination more readily than males. As age increased, the PLWHA sought medical advice more often and suffered more discrimination.

Percentage of four types of medical discrimination perceived by the PLWHA.
aPercentage of four types of self-medical discrimination reported in the total number of medical discrimination.
bVariable was expressed as ratio.

Distribution of four types of self-perceived medical discrimination and different socio-demographic characteristics of PLWHA (n = 443).
aPercentage of four types of self-perceived medical discrimination reported in different socio-demographic characteristics and disease characteristics.
bcategorical variable was expressed as frequency.
PLWHA more readily encountered discrimination through medical institutions, such as general hospitals, primary hospitals and private clinics. The proportion was 62.2%, 54.4% and 43.8% respectively, whereas in the AIDS-designated hospitals, they suffered the least medical discrimination, at only 7.4%. In the course of medical treatment, PLWHA thought they were more vulnerable suffering discrimination from nurses (36.9%), followed by doctors (33.2%)and patients in the same ward (19.8%). The medical department with high occupational exposure risk more readily provided unfair treatment. The therapeutic procedures that resulted in discrimination were concentrated in clinics (28.6%), hospitalizations (23.5%), and surgical procedures (17.5%). Because of the existence of medical discrimination, survey data showed that 67.0% of all the participants were unwilling to proactively inform the doctor of their infection. The reasons were, in order, being afraid of being rejected treatment (46.8%) privacy protection (43.8%) and fear of discrimination and ridicule (42.1%). When confronted with discrimination, 52.2% of the patients with medical discrimination chose to endure in silence, and 24.9% swallowed the insult indignantly. Additionally, 17.5% strove for their legitimate rights.
Factors associated with self-perceived medical discriminationTable 3 shows that there no significant differences in sex, age, birthplace, education condition or familiarity with HIV/AIDS-related law between medical discrimination and characteristic variables. However, the differences in discrimination among the types of first check, infection routes and disease stages were statistically significant (p < 0.05). As exhibited by the multivariable regression analysis (Table 4), PLWHA who determined they were infected through involuntary testing, were more likely to perceive medical discrimination (OR: 1.738), especially the refusal of treatment (OR: 1.592). The risk of AIDS patients suffering medical discrimination was 3.566 times that of asymptomatic HIV-infected patients. In addition, AIDS patients were more likely to be treated ruthlessly (OR: 2.125) and have their private information revealed (OR: 2.555). In addition, disease infection routes affected the discrimination in the leakage of private information, as people who contracted the virus via having sex with others were more fearful of having their illness revealed than those who contracted it via blameless blood products and their peers. The ratio risk for homosexual transmission was 3.981. People who were unfamiliar with HIV/AIDS-related law more readily suffered medical compulsory tests than those who knew the law (OR: 2.930).
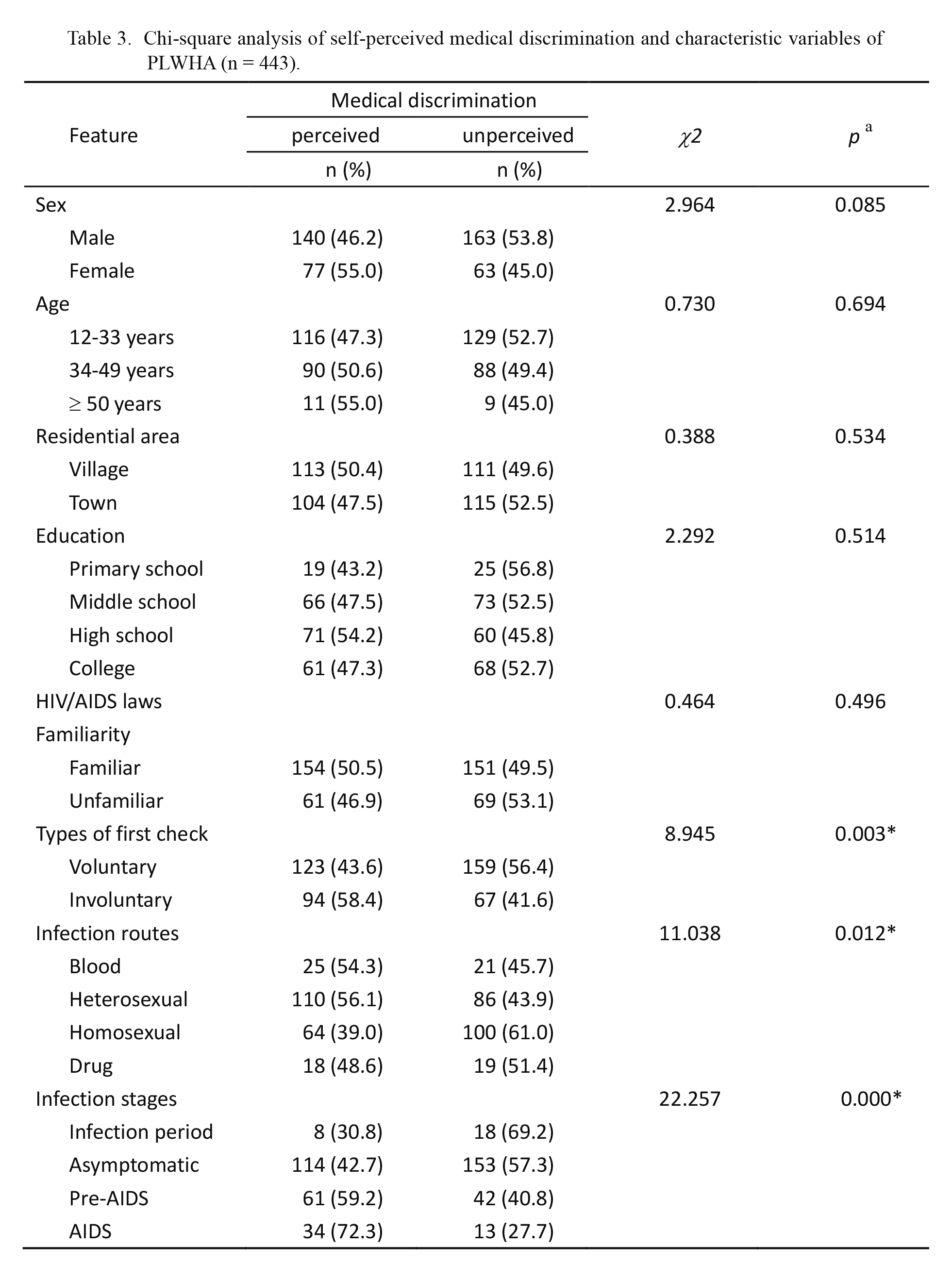
Chi-square analysis of self-perceived medical discrimination and characteristic variables of PLWHA (n = 443).
aCategorical variables were detected by Chi-square test. If p ≤ 0.05, it was regarded as statistical significance.
*Indicates the statistical significance under the condition of α = 0.05.

Multivariate unconditioned logistic regression analysis of factors associated with different types of PLWHA self-perceived medical discrimination (n = 443).
aCategorical variables were detected by multivariate unconditioned logistic regression analysis. If p ≤ 0.05 or 95% confidence interval did not include value one, it was regarded as statistical significance.
*Indicates the statistical significance under the condition of α = 0.05.
OR, Odds ratio; CI, Confidence interval.
The multivariate stepwise regression analysis in Table 5 demonstrates that female respondents had higher scores than males on health worries, but men were significantly more likely to have a better understanding of HIV than women. The data showed that the participants with reliable partners had higher scores on provider trust, HIV awareness and sexual function, whereas they were more worried about finances than individual patients. Meanwhile, workers were better than the unemployed in term of financial concerns. In addition, PLWHA with an urban household registration understood more about HIV than those living in rural areas. Additionally, patients who contracted the disease through sexually transmitted infection had a better ability to master HIV-related knowledge than those who were blood-borne. PLWHA without HIV/AIDS-related complications had higher scores on overall function and financial worries than those with complications. Patients who received antiretroviral therapy had higher scores on medication concerns than those who did not. When compared to those who had not experienced medical discrimination, patients who ever experienced medical discrimination had lower overall functional scores, and they were more likely to worry about news of their infection being leaked. In this study, we also found no variables that affected the life satisfaction of patients.

Multivariate linear regression analysis results of quality of life and the explanatory variables (n = 443).
aContinuous variables were detected by multivariate linear regression analysis. If p ≤ 0.05 or 95% confidence interval did not include value one, it was regarded as statistical significance.
*Indicates the statistical significance under the condition of α = 0.05.
OR, Odds ratio; CI, Confidence interval.
With the aggravation of the AIDS epidemic, China developed AIDS prevention and control regulations in 2006, formulated tort liability law in 2009 and promulgated AIDS prevention and containment in the 12th Five Year Plan of action in 2012. These laws and regulations clearly defined how to protect the infected patient’s right for medical treatment and privacy. However, in recent years, PLWHA have been universally discriminated against in medical treatment. It is difficult for PLWHA to obtain medical advice and have surgeries (Jia 2016). HIV/AIDS-related discrimination occurs everywhere, but PLWHA may have more serious consequences in healthcare settings (Ahsan Ullah 2011). According to previous findings, HIV/AIDS-related discrimination has been extensively documented among healthcare providers, and an average level of discriminatory attitudes exists among health care workers in many studies (Sadob et al. 2006; Hossain and Kippax 2010).
In our study, we found that 49% of PLWHA had perceived discrimination from health workers in the process of seeking medical attention. One of the most commonly reported forms of discrimination is discriminatory treatment, followed by refusal of treatment, privacy leakage and mandatory testing. Although the data were conservative, this has become an urgent social problem to be solved in China. Results also showed that those who were older, female, from a rural area and had a higher educational level were more likely to perceive medical discrimination. The reason may be that the older they became, a higher frequency of seeking medical treatment should be expected and they would have more opportunities to perceive discrimination, especially for women, who could also require obstetric and gynecological treatment. General hospitals have medical and technical abilities enough to treat AIDS patients. They refused to treat PLWHA, however, from an economic perspective, because receiving PLWHA might result in loss of other patients. The level of knowledge about HIV among nurses was not as comprehensive and extensive as the doctors, and discrimination was more common among nurses. This was consistent with a study that demonstrated that healthcare providers who had lower basic HIV knowledge had higher discrimination scores (Umeh et al. 2008; Ahsan Ullah 2011; Doka et al. 2017).
Currently, most hospitals’ lack of a strict series of AIDS occupational protection training or rules and regulations results in poor knowledge and skills among medical staff. Additionally, occupational exposure to HIV/AIDS in China has not been included in the scope of work-related injuries or occupational diseases, and there is no legal mechanism as yet for protection and compensation. A sound occupational exposure surveillance system has not been fully formed by most hospitals, which objectively hinders the supply of medical personnel health services. Medical staffs face more exposure risk when providing gynecological operations to female patients. A previous survey found that, after knowing the identity of the infected persons, a quarter of medical workers hold a negative or discriminatory attitude (Nie and Wang 2010). Therefore, more than half of the patients chose to conceal their infection when seeking medical advice. In addition, when they suffered discrimination, the majority of infectors chose to endure in silence. This silence was not conducive to alleviating the illness and controlling the spread of HIV. This finding was in agreement with previous studies, which indicated that when patients take inactive or negative measures to cope with the disease, they were more likely to perceive discrimination (Martin et al. 2013). Moreover, a survey of female patients also indicated that those with an avoidant style were more likely to have high levels of perceived discrimination (Nyamathi et al. 2013).
Involuntary testing often occurred in the hospital routine check before surgery. It did not represent the true wishes of patients, and at this time, if the test results were positive, the doctor would stop providing treatment services and transfer patients to designated hospitals. Patients, understanding the law, would take measures to defend their rights and interests in the process of diagnosis and treatment. Therefore, they can communicate with medical staff efficiently in order to ensure the maximization of their interests. In this way, PLWHA can avoid being discriminated against by medical personnel so that they can be treated properly. Meanwhile, several other studies have shown that the HIV infection route influenced perceived discrimination (Li et al. 2009; Brener et al. 2013). A possible explanation for this situation could be that individuals with sexual transmission usually had a chaotic sex life that was contrary to a normal dating relationship, and they may be more afraid of the reception that their illness may receive from family members and especially from their spouses. In addition, homosexual infectors are at elevated risk of HIV acquisition and transmission, live outside of broad social expectations for gender roles, and therefore often experience prejudice against homosexual individuals (Altman et al. 2012). The level of discriminatory medical treatment appears to be higher for PLWHA who have AIDS with various opportunistic infections when compared to those who have not yet presented with the typical symptoms. Previous relevant studies found that self-perceived health status was a predictor of discrimination, and the worse their physical condition, the higher the level of discriminatory treatment they received (Emlet et al. 2013).
At present, the traditional prevention and treatment pattern of HIV/AIDS have been changed into a combination of social participation, social intervention and social support. Social support which defined as the fighting spirit against AIDS was significantly associated with health-related quality of life (Nunes et al. 1995). It places great emphasis on the subjective feelings of infectors and can evaluate the therapeutic effect of AIDS more comprehensively than the traditional objective indicators such as mortality or CD4+ T lymphocytes (Subramanian et al. 2009). It also can provide a comprehensive basis to screen for intervention measures and health resource allocation decisions (Li et al. 2011). According to analysis, the infectors who have spouses have better quality of life, which means that family support has positive impact on living quality. In addition, with a steady job and income, PLWHA can receive timely treatment and care to reduce the physical and mental pressure of HIV infection and improve self-esteem at the same time. It is important to note that in this study, self-perceived medical discrimination continues to affect the quality of life of PLWHA in this cohort. This finding provides evidence that perceived HIV discrimination has a significantly negative and constant impact upon overall function. Besides, we found no variables that affected the life satisfaction of patients, indicating that the regulation of life satisfaction was influenced by many confounding factors, and thus further detailed studies are needed in the future.
In conclusion, our research findings can better reflect the true experience and inner desire of PLWHA from the perspective of patients to explore the characteristics of medical discrimination. Therefore, future treatment and support for AIDS patients should be more in line with their real needs, and they can get timely and effective help and treatment, thereby reducing the burden on patients and curbing the spread of HIV. The quality of life of PLWHA was inseparable with disease status and living conditions. The government should implement measures to improve the patient’s sense of social existence and alleviate the deterioration of the disease, thereby enhancing quality of life in the future.
This paper was completed with the support of the eighth People’s Hospital of Guangzhou and the third People’s Hospital of Shenzhen in Guangdong Province. We would like to thank the investigators and field workers for their collaboration and support, especially the Doctors Weiping Cai and Hui Wang.
This research was supported by a grant from the Medical Scientific Research Foundation of Guangdong Province and the Liaoyuan Foundation of Jinan University, item numbers A2013336 and JNUPHPM20160102, respectively.
The authors declare no conflict of interest.