2017 Volume 243 Issue 2 Pages 101-105
2017 Volume 243 Issue 2 Pages 101-105
The rare and deadly Ebola virus disease (EVD) is caused by Ebola virus (EBOV) infection. The 2014-2015 EVD outbreak in West Africa was unprecedented. Person-to-person transmission of EBOV by direct contact with the body or bodily fluids of an infected person through broken skin or unprotected mucous membrane caused rapid outbreak in communities. Nosocomial infection was the cause of death of many health care workers (HCWs). This paper aims to reveal the importance and effect of intensive education of HCWs when combating an outbreak such as EVD. We compared the curricula of two educational programs and analyzed their effects by the trend of weekly new patients. In September 2014, a three-day training program on infection, prevention and control (IPC) was organized for nurses, but it was not sufficient to achieve good outcome. In December 2014, a newly established National Ebola Training Academy was set up to offer a platform of clinical training modules for frontline Ebola response workers. This academy addressed the training needs of clinicians and hygienists who were working or will work at Ebola treatment centers that were established after the onset of the 2014 outbreak. Increased intensive contents and simulated training at the academy improved HCWs’ understanding of EVD, IPC and patient care, which subsequently contributed to the survival of patients. The rapid settlement of the outbreak after introducing the Academy indicates that appropriate intensive education of HCWs is the key activity carried out to control the outbreak of EVD in Sierra Leone.
The rare and deadly Ebola virus disease (EVD), initially called Ebola hemorrhagic fever, is caused by infection with one of the strains of Ebola virus. The introduction of Ebola virus into the human population was likely caused by contact with infected animals, such as fruit bats. Several bat species are putative Ebola virus reservoirs. With respect to the 2014-2015 West African Ebola outbreak, three types have been implicated: the hammer-headed fruit bat (Hypsignathus monstrosus), the little collared fruit bat (Myonycteris torquata), and the Franquet’s epauletted fruit bat (Epomops franqueti) (Leroy et al. 2005; WHO, World Health Organization 2014a). This zoonotic disease causes person-to-person transmission by direct contact with the body or bodily fluids such as blood, vomitus, saliva, urine, feces and semen of an infected person through broken skin or unprotected mucous membranes. Furthermore, EBOV can be transmitted among people via direct contact with surfaces and materials that have been contaminated with infected bodily fluids. The corpse of an infected person is extremely contagious. Therefore, funeral practices involving direct contact with a corpse is another means of transmission. The symptoms of EVD include abdominal pain, diarrhea, fatigue, fever, headache, muscle pain, vomiting, and unexplained bleeding. However, during the 2014-2015 outbreak, there was no predominance of hemorrhagic complications in infected patients (Paessler and Walker 2013; Xu et al. 2016).
The 2014-2015 EVD outbreak in West Africa was unprecedented in history (Farrar and Piot 2014). After laboratory confirmation of a suspected Ebola case in the eastern district of Kailahun, which borders Guinea and Liberia, an EVD outbreak was declared in Sierra Leone by the government through its Ministry of Health and Sanitation (MOHS) on May 25, 2014 (Dixon and Schafer 2014). On August 8, 2014, WHO declared the EVD outbreak as a “Public Health Emergency of International Concern” (WHO 2014b). The Sierra Leone National Ebola Response Centre (NERC) as of December 23, 2015 reported a cumulative total confirmed EVD cases of 8,704 with deaths of 3,589 (excluding probable and suspected cases) (NERC, National Ebola Response Centre 2015). Freetown, situated on the Atlantic coast, is home to more than 1 million people and, is the capital and largest city of Sierra Leone. As a result of its dense population, Freetown and its surrounding Western region was the most affected area of the 2014-2015 EVD epidemic in Sierra Leone. The West African region was declared EVD free on January 14, 2016 (WHO 2016). However, sporadic cases were identified through enhanced surveillance even though WHO had declared the outbreak over in West Africa. All cases were controlled rapidly, but the potential for multiple flare-ups exists in the region because of the fact that male survivors can sexually transmit the infection (Mate et al. 2015; Christie et al. 2015).
In Sierra Leone, one reason for the initial failure to control the outbreak was inadequate education on infection, prevention and control (IPC). Nosocomial infection caused the death of many health care workers (HCWs). This raised public concern for establishment of Ebola treatment centers (ETCs) and HCWs to be provided with the necessary personal protective equipment (PPE) and training to serve in their respective roles effectively and safely.
In this paper, we aim to reveal the importance and effect of intensive education of HCWs when combating an outbreak such as EVD.
Three phases of training programs of HCWsOn September 16-18, 2014 a three-day training program was organized for nurses by WHO and MOHS Sierra Leone. During this training, nurses were taught about the Ebola virus and measures taken to prevent transmission of the virus. This course was organized in Freetown just once. At that time, there were two ETCs in Sierra Leone (Lassa Fever Hospital in Kenema and ETC by UK Aid in Kerry Town). However, it turned out that two ETCs were not sufficient for the situation. Thus, the Sierra Leonean Government needed to establish additional ETCs and educate the HCWs to deal with the outbreak.
In December 2014, a National Ebola Training Academy was set up in Freetown by International Organization of Migrants (IOM) in partnership with WHO, UK Aid, the Sierra Leone MOHS, the College of Medicine and Allied Health Sciences (COMAHS) and the Republic of Sierra Leone Armed Forces (RSLAF). From December 1, 2014 to March 28, 2015, more than 5,000 frontline workers were trained (IOM, International Organization of Migrants 2015a). The Training Academy offered different courses using WHO curriculum and as of May 23, 2015 the number of HCWs trained had increased to more than 6,000 (Table 1) (IOM 2015b).
HCWs were also trained at their respective ETCs to encourage them to continue to work diligently and safely. It cautioned them against familiarity which was creeping in among them, since many patients were surviving the disease.
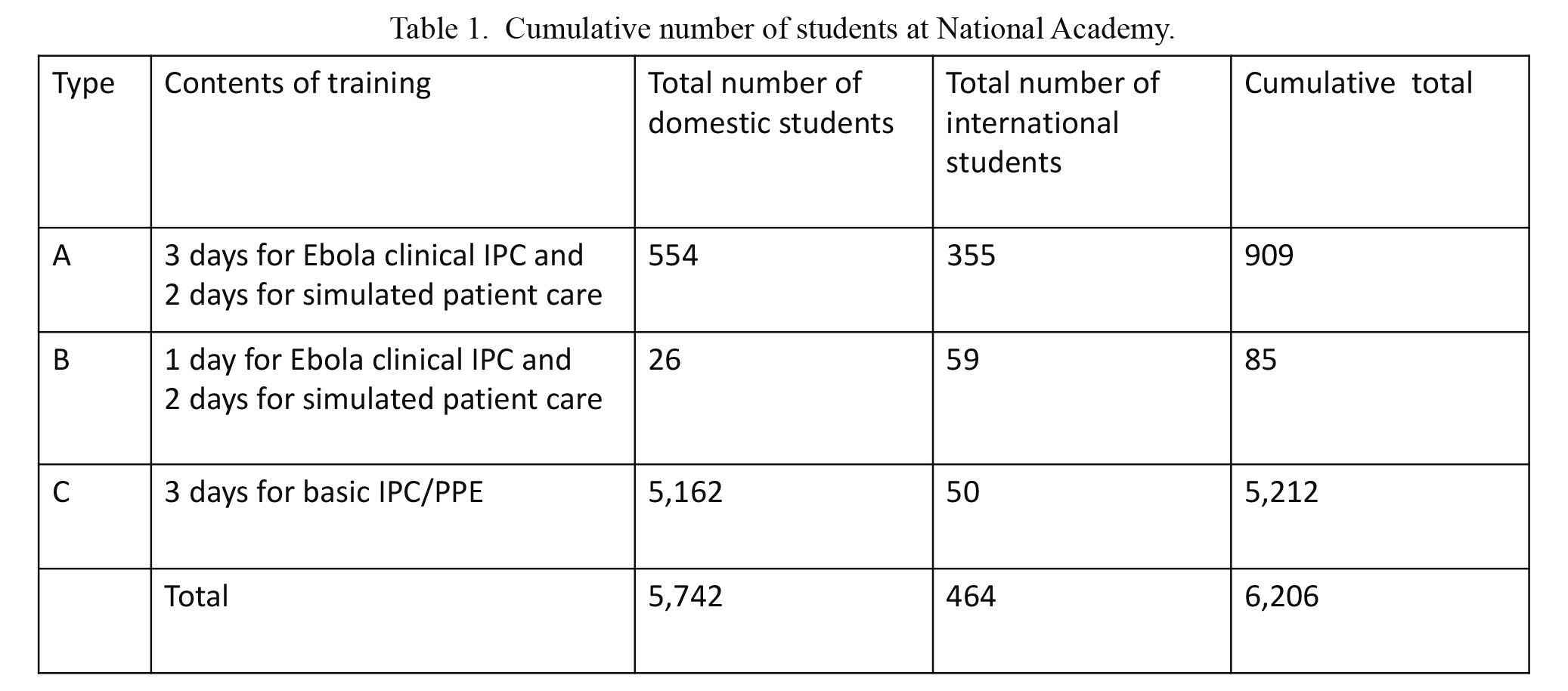
Cumulative number of students at National Academy.
IPC, Infection, Prevention and Control; PPE, Personal Protective Equipment.
(December 1, 2014-May 23, 2015, modified from IOM report (IOM 2015b))
The curriculum used for the initial training during early phase of the outbreak in September 2014 was the facilitators guide for IPC in the training of nurses, cleaners, hygienists and others working at an ETC.
This included:
● What is EVD and how it is transmitted.
● Signs and symptoms of EVD
● Open discussion on the effect of EVD on the community and how its spread can be stopped.
● Transmission of EVD in the health facility
● The concept behind the layout of the facility
● Putting on and removing PPE
● How to safely work at an EVD facility
● Preparing chlorine (bleach) solutions
Curriculum of training at the National AcademyThe National Academy offers a new platform of clinical training modules for frontline Ebola response practitioners to address the training needs of clinicians and hygienists working at ETCs.
The Academy offered theory, case studies, isolated skill station to perfect critical standards for working at an ETC and simulated case management at a mock Ebola Treatment Unit (ETU). The curriculum of training at the National Academy featured a three-day module on donning and doffing of Personal Protective Equipment (PPE), proper hand hygiene, mixing of chlorine solution, spill clean-up, identifying and dealing with Ebola infections and small group tutorials. Also a two-day practical component of an onsite mock ETU that took health care workers through various scenarios in each stage of the ETU was carried out.
The curriculum of the training academy was compared with that of the initial training by MOHS (Table 2). The training at the academy was more intensive, revealing how HCWs should prepare for working at the ETC, the IPC needed to be carried out by HCWs, clinical care and clinical cases at the ETC. Also another major difference between the two curricula was the inclusion of simulated patients and survivors’ panel discussion during the training at the Academy. A total of 10 survivors acted as expert simulated patients during the onsite mock ETU and also shared their experiences of the disease, treatment and life after Ebola in a panel discussion.

Comparison between Initial Training and Training at National Academy.
ETU, Ebola Treatment Unit.
The Training Academy offered the following courses using a WHO curriculum and these courses were taken in various combinations based on experience and needs (IOM 2014) (Table 1):
A) 5-day clinical training for clinicians without prior IPC/PPE training: This includes 3-day enhanced clinical/IPC training with lectures and skills stations, and 2-day simulated patient exercises at a mock ETU. This course was provided both at the National Academy and at the mobile education facility throughout the country.
B) 3-day augmented clinical training for clinicians with prior IPC/PPE training: This includes 1-day augmented clinical/IPC training with lectures, skills stations and clinical cases, and 2-day simulated patient exercises at a mock ETU.
C) 3-day IPC/PPE training for cleaners/hygienists.
Trends of EVD patient situations in Sierra LeoneData were retrieved from the WHO situation report archive (WHO 2015) to plot the weekly trends of confirmed new patients and new deaths (Fig. 1). Numbers of new patients and deaths were calculated by subtraction of the published cumulative numbers in two consecutive weeks. No data were available for new deaths before November 14, 2014 although the cumulative confirmed EVD deaths as of November 14, 2014 were 978 in Sierra Leone.

Three phases of the training system and weekly trends of the numbers of confirmed new patients and new deaths in Sierra Leone.
Solid circles, number of confirmed new patients; blank circles, number of confirmed new deaths. Data source: WHO Situation Summary, Data on new deaths before November 14, 2014 were not available, although the cumulative deaths as of November 14, 2014 were 978.
After the training in the mid of September 2014, the nurses started working at various treatment centers but there was no significant improvement in the outcome of the Ebola outbreak.
The training at the National Ebola Training Academy dealt with every aspect of the disease that was useful for the survival of patients and HCWs thus improving HCWs’ understanding of Ebola. That feeling of comfort decreased anxiety during patient care. Although there was no drug for treatment of EVD, effective patient care and IPC played a great role in controlling the outbreak. The peak of new patients occurred during the period from September to December 2014, and the number of new confirmed patients and deaths declined rapidly after introduction of the intensive education and training at the National Ebola Training Academy (Fig. 1).
The expert knowledge and skills of health practitioners made the difference in controlling the epidemic in Sierra Leone. Therefore, intensive and effective education of HCWs in countries that are prone to infectious diseases can be a strong defense mechanism to prevent, detect, and respond to future epidemics as soon as they occur.
This work was supported in part by a grant from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (MEXT) for the Joint Research Program of the Research Center for Zoonosis Control, Hokkaido University. Tracey Elizabeth Claire Jones is a participant of the African Business Education Initiative scholarship from Japan International Cooperation Agency (JICA).
The authors declare no conflict of interest.