Abstract
Atypical femoral fractures (AFFs) are defined as atraumatic or low-trauma fractures located in the subtrochanteric or diaphyseal sites. Long-term bisphosphonates (BPs) are administered to prevent fragility fractures in patients with primary osteoporosis or collagen diseases who are already taking glucocorticoids (GCs). Long-term BP use is one of the most important risk factors for AFFs. Its pathogenesis is characterized by severely suppressed bone turnover (SSBT), but whether the characteristics of patients are different regarding to location of fracture site remains unknown. In this study, we compared the characteristics and bone histomorphometric findings between subtrochanteric and diaphyseal sites in patients with BP-associated AFFs. Nine women with BP-associated AFFs were recruited, including 3 with systemic lupus erythematosus, 2 with rheumatoid arthritis, 2 with primary osteoporosis, 1 with polymyalgia rheumatica, and 1 with sarcoidosis. Patients were divided into the subtrochanteric group (n = 5; average age, 52 years; BP treatment, 5.9 years) and the diaphyseal group (n = 4; average age, 77 years; BP treatment, 2.6 years). Compared with the diaphyseal group, the subtrochanteric group had significantly higher daily GC doses (average, 10.9 vs. 2.3 mg/day) and significantly lower serum 25-hydroxyvitamin-D levels (17.8 vs. 25.6 ng/mL). Bone histomorphometry of the biopsied iliac bone showed SSBT in 3 cases (subtrochanteric, n = 1; diaphyseal, n = 2). Osteoid volume and trabecular thickness were significantly lower in the subtrochanteric group than in the diaphyseal group. Bone formation was inhibited more severely in subtrochanteric than in the diaphyseal group due to the higher GC doses used.
Introduction
Bisphosphonates (BPs) reduce the fracture risk in women with postmenopausal osteoporosis (Black et al. 1996). However, it has been reported that long-term BP use may affect the incidence of atypical femoral fractures (AFFs) (Shane et al. 2010). A typical femoral fracture is defined as a high-energy trauma, such as a traffic accident, that is frequently accompanied by a third fragment and shape of comminuted fracture. However, AFFs are defined as atraumatic or low-trauma fractures located in the subtrochanteric region or femoral shaft (Shane et al. 2014). The number of studies investigating the association between long-term BP use and AFFs have recently increased (Girgis et al. 2010; Meier et al. 2012). The causality of AFF is as follows: the accumulation of microdamage (Mashiba et al. 2001) leads to homogeneity in bone tissue, which becomes low due to BP use, and subsequently leads to lower bone quality (Saito et al. 2008). A recent review demonstrated that long-term BP exposure causes premature aging of bone, rendering them more brittle and less likely to impede crack tip progression (Ettinger et al. 2013). Odvina et al. (2005) advocated that the pathogenesis of AFFs is associated with biopsy-proven, severely suppressed bone turnover (SSBT). They reported that of 9 patients with nonvertebral fractures, 5 had femoral fractures. The average duration of bisphosphonate treatment was 5.6 years and bone histomorphometric findings from the iliac bone demonstrated prominently decreased bone formation and bone resorption.
Other studies have reported limited bone histomorphometric data in patients with atypical femoral fractures (Visekruna et al. 2008; Somford et al. 2009; Tamminen et al. 2013). Low trabecular bone volume and low heterogeneity were reported in 4 cases (Tamminen et al. 2013). A patient with iliac bone histomorphometry rheumatoid arthritis and bilateral femoral subtrochanteric/diaphyseal fractures treated with alendronate for 8 years exhibited decreased bone formation but increased bone resorption (Somford et al. 2009). Double tetracycline-labeled bone biopsy revealed low activation frequency or limited single tetracycline labeling in 3 patients treated with long-term BP (Visekruna et al. 2008).
Femoral geometry is associated with the incidence of AFFs (Sasaki et al. 2012; Tsuchie et al. 2016). Low concentration of 25-hydroxyvitamin D (25-OH-D) less than 16 ng/ml increased the risk of subtrochanteric fractures (OR = 3.2) and prednisolone showed high Odds ratio (Shane et al. 2010). Taking BPs and glucocorticoids (GCs), as well as having collagen disease are risk factors for AFFs (Saita et al. 2015). In another report, 8 patients and 11 AFFs (3 patients had bilateral AFFs) with comorbidities including rheumatic diseases, systemic lupus erythematosus, and polymyositis were dominant (totally 4 cases, 50%); the average GC dose was 13.9 mg/day (Takakubo et al. 2017). These results suggest that collagen diseases and GC use accounted for high percentages of AFFs. However, the problem is that the risk factors have been discussed with mixed situations independently fracture sites. In addition, the detailed bone histomorphometric findings of BP-related AFFs remain unknown. For instance, whether all the cases of atypical femoral fractures show SSBT in iliac bone histomorphometry or not is not clear.
We hypothesized that the clear detection of the differences of clinical features or pathological findings between subtrochanteric and diaphyseal sites in atypical femoral fractures is useful for understanding the pathogenesis of AFFs or treatment intervention. Therefore, we evaluated the differences in clinical features, bone metabolism, including bone histomorphometric findings from biopsied iliac bone and femoral lateral bowing, between subtrochanteric and diaphyseal sites in patients with AFFs.
Patients and Methods
We retrospectively reviewed medical records of femoral fractures at our facility between January 2009 and June 2014. The total number of femoral fractures were 105 cases. AFFs were determined based on ASBMR Task Force 2013 revised case definition of AFFs (Shane et al. 2014). Major features include: 1) fractures associated with minimal or no trauma, as in a fall from a standing height or less; 2) fracture lines that originated at the lateral cortex and were substantially transverse in its orientation, although that could become oblique as it progressed medially across the femur; 3) complete fractures extending through both cortices and that may be associated with a medial spike, and incomplete fractures that only involved the lateral cortex; 4) noncomminuted or minimally comminuted fractures; and 5) localized periosteal or endosteal thickening of the lateral cortex that is resent at the fracture site (i.e., beaking or flaring). Minor features include: 1) generalized increase in cortical thickness of the femoral diaphysis; 2) unilateral or bilateral prodromal symptoms such as dull or aching pain in the groin or thigh; 3) bilateral incomplete of complete femoral diaphysis fractures; and 4) delayed fracture healing. Cases fulfilling 4 of 5 major features were diagnosed with AFF.
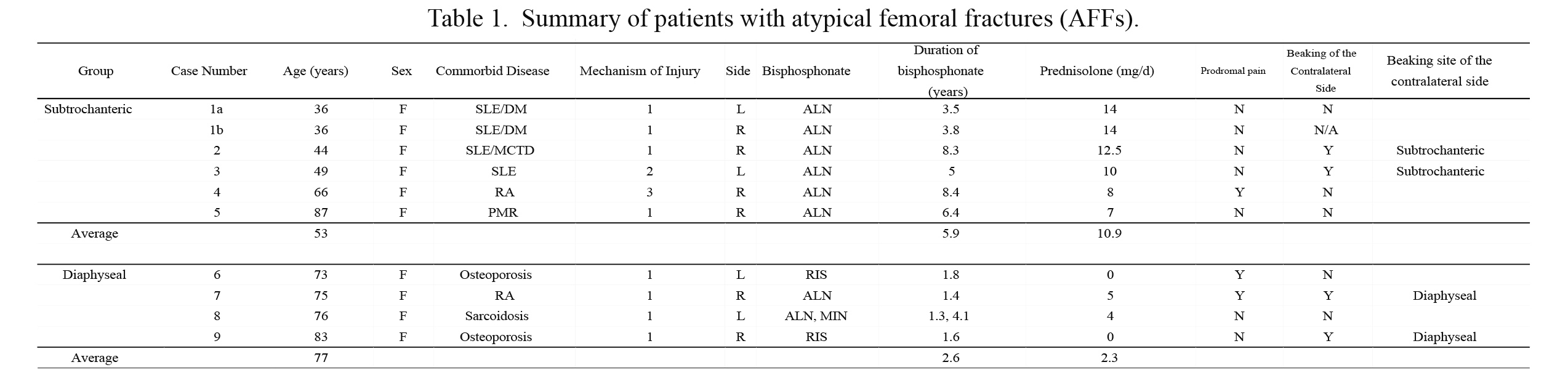
Nine cases and 10 limbs (9.4%) were diagnosed with AFFs. All cases were administered BPs. Case 1 had bilateral subtrochanteric atypical femoral fractures; see case 1a (left subtrochanteric fracture) and case 1b (right subtrochanteric fracture). We divided 9 patients into the 2 groups based on the fracture site: 5 patients with 6 subtrochanteric fractures (subtrochanteric group) and 4 patients with 4 diaphyseal fractures (diaphyseal group) (Table 1). Subtrochanteric was defined as being less than 5 cm distal from lesser trochanter, and diaphyseal was defined as being more than 5 cm distal from the lesser trochanter to the supracondylar site (Fig. 1). Ethics Committee approval was obtained from Niigata University Medical and Dental Hospital.
Survey of prodromal pain and latent fracture on the contralateral side
Prodromal pain was defined as precursor symptoms, including dull or aching pain in the groin or thigh; it is included as a minor feature in the case definition of AFF. We evaluated whether each case had prodromal thigh pain before the incidence of complete AFFs. Findings from radiography or magnetic resonance imaging of the contralateral side were evaluated to examine latent AFF on the contralateral side.
Biochemical measurements
Laboratory scores were obtained shortly after the primary surgery. Serum samples were assayed for calcium (Ca), inorganic phosphorous (iP), alkaline phosphatase (ALP), bone-specific alkaline phosphatase (BAP; a bone formation marker), intact parathyroid hormone (PTH), and 25-hydroxyvitamin D (25-OH-D). Urine samples were examined for type I collagen crosslinked N-telopeptide (uNTx), and the uNTx level was normalized to that of urine creatinine (Cr) as a bone resorption marker.
Bone mineral density and incidence of AFF
X-ray absorptiometry (HOLOGIC, Tokyo, Japan) was used to measure bone mineral density (BMD) of the lumbar spine (L2 to L4). Measurements were obtained immediately after the onset of AFFs. T-scores were used to classify patients into the following three groups: normal, ≤ –1.0; osteopenia, > –2.5 to –1.0; and osteoporosis, ≤ –2.5.
Histomorphometric analysis of biopsied bone
A transiliac bone biopsy was performed after obtaining informed consent from the patients. In cases 1 and 3, iliac bone was biopsied during the revision surgery. Based on the treatments for cases 1 and 3, AFFs tended to exhibit delayed union or non-union. In the other cases, an iliac bone graft was primarily used during open reduction and internal fixation. However, in case 5, a bone biopsy was not performed because informed consent was not obtained from the patient.
Tissue preparation and bone histomorphometric analysis
Specimens were prestained for 72 hours using Villanueva bone stain. Following dehydration in an increasing concentration of alcohol, they were embedded in methyl methacrylate and kept at 37ºC until fully polymerized. Embedded biopsy samples were subsequently sectioned on a microtome (Leica RM2255; Leica Inc., Nussloch, Germany) at a thickness of 5 µm.
Histomorphometric measurements were obtained with a system consisting of an epifluorescence microscope (Olympus BX50; Olympus America Inc., Center Valley, PA, USA), a bone histomorphometry system, and software program (Histometry RT Camera; System Supply, Co., Nagano, Japan), which were connected to an Epson computer (Shinshu Seiki Co., Ltd., Nagano, Japan).
Bone histomorphometric findings and SSBT diagnosis
Bone histomorphometric data from each patient were compared to reference values depending on the patients’ age (Recker et al. 1988). When both bone formations (bone volume (BV/TV), trabecular thickness (Tb.Th), and trabecular width (W.Th) as for bone volume, and osteoid volume (OV/TV, OV/BV), osteoid surface (OS/BS), osteoid thickness (O.Th) as for bone formation), and bone resorption (eroded surface (ES/BS)) parameters were lower than the average value, the patient was defined as having “SSBT.” In addition, z-value of each parameter was calculated based on the reference data (Recker et al. 1988). Then, statistical analysis was performed for each parameter using Mann-Whitney U test.
Lateral bowing evaluation using radiography
Since it has been reported that increased femoral curvature may be a causative factor for AFFs (Sasaki et al. 2012), we evaluated femoral lateral bowing using radiography. The lower limbs (total, 7) were evaluated using the entire anteroposterior femur. Lateral bowing of the femur was evaluated using the method outlined previously (Fujimaki et al. 2002). F1 was the midpoint of the transverse line, 3 cm distal to the lesser trochanter. F2 was the midpoint of the line, 6 cm proximal to the line through the joint surfaces of the lateral and medial condyles. The point equidistant to F1 and F2 was labeled N. The most lateral point of the transverse line was drawn through N and labeled N1, while the medial point was labeled N2. The ratio N1N:N1N2 × 100 (%) was the lateral bowing ratio.
Patients with lateral bowing of > 60% were defined as having femoral lateral bowing.
Statistical analysis
The Mann-Whitney U test or Pearson regression analysis was performed, and a p-value < 0.05 was defined as statistically significant. The SPSS version 21 software (SPSS, Inc., Chicago, IL, USA) was used to perform all statistical analyses.
Results
In total, 9 patients (10 limbs) with bisphosphonate-related AFFs were recruited. Of these patients, case 1 had bilateral AFFs. Patients were aged 36 to 87 years (average, 62 years) and the sites of fracture were subtrochanteric in 5 cases (6 limbs) and diaphyseal in 4 cases (4 limbs). Comorbid diseases comprised systemic lupus erythematosus (n = 3), including 1 complicated with dermatomyositis and 1 complicated with mixed connective tissue disease, rheumatoid arthritis (n = 2), primary osteoporosis (n = 2), polymyalgia rheumatica (n = 1), and sarcoidosis (n = 1).
Average duration of BP therapy was 4.1 years (range, 1.4 to 8.4 years). In total, 7 patients were taking alendronate; 2 patients, risedronate; and 1 patient, minodronate (4.1 years) following alendronate (1.3 years) treatment (case 8). Prednisolne (PSL) was used in 7 patients (average, 7.3 mg/day; range, 4-14 mg/day). Fractures developed when falling from a standing position in 8 cases, when losing footing from a standing position (case 3), and while walking (case 4). Patient characteristics are shown in Table 1.
The average age of patients was 53 years and 77 years in subtrochanteric group and diaphyseal group, respectively, indicating that individuals in the subtrochanteric group tended to be younger than those in diaphyseal group. The average duration of BP use was 5.9 years (3.5-8.4 years) in subtrochanteric group, which was longer than that in diaphyseal group (2.1 years; range, 1.4-5.4 years). No correlation was detected between age and BP duration following regression analysis (r = –0.19, p = 0.6).
Daily dose of PSL differed between the two groups (subtrochanteric group: 10.9 mg/day vs. diaphyseal group: 2.3 mg/day, p = 0.01). Two patients did not receive PSL in diaphyseal group.
The rate of prodromal pain was 17% (1/6 patients) in subtrochanteric group and 50% (2/4) in diaphyseal group. Beaking was detected on the contralateral side using radiography in 2/5 (40%) patients in subtrochanteric group and in 2/4 (50%) in diaphyseal group. The site of beaking was symmetrical in all 4 patients (Table 1).
Laboratory findings at the time of the surgery
Serum Ca and ALP levels from all patients were within the reference range (Table 2). The iP level was within the reference range in all patients, except case 7 (1.7 mg/dL). The serum BAP level was 5.6-10.5 U/L, and a low BAP level was detected in 3 patients (cases 2, 4, and 8). The uNTx level was relatively high in all patients, except case 5 (78 pg/mL). The serum 25-OH-D level was 20.7 ± 4.6 ng/mL on average. The serum 25-OH-D level was significantly lower in the S group, (17.8 ± 1.7 ng/mL), compared with the D group (25.6 ± 3.1 ng/mL; p < 0.05; Table 3). No significant difference in BMD was detected between the two groups.
Statistical comparison of each parameter
Daily dose of PSL was significantly higher in subtrochanteric group (10.9 mg/day), compared with that of diaphyseal group (2.3 mg/day; p < 0.05; Table 3). In addition, the serum 25-OH-D level was significantly lower in subtrochanteric group (17.8 ng/mL) than in diaphyseal group (25.6 ng/mL; p < 0.05). No significant difference was detected between the two groups in the other parameters (Table 3).
Bone histomorphometric findings and SSBT diagnosis
Table 4 shows bone histomorphometric findings. In the subtrochanteric group, bone volume parameters (BV/TV, Tb.Th, and W.Th) were lower than the reference value, except W.Th in case 4. Bone formation parameters (OV/TV, OV/BV, OS/BS, and O.Th) were lower than the reference value, except OV/TV in case 2. However, bone resorption parameters (ES/BS) only decreased in case 1 (0.69%). No osteoclast was detected in case 1 (Oc.N/BS was 0), and was determined as SSBT.
In the diaphyseal group, bone volume parameters were not always lower than the reference value; 2/4 patients exhibited reduced BV/TV (cases 7 and 8) and 1/4 patients exhibited reduced W.Th (case 7). In addition, bone formation parameters (OV/TV, OV/BV, OS/BD, and O.Th) were either normal or reduced, excluding the possibility of osteomalacia. Bone resorption parameters (ES/BS) were lower in 3/4 patients (case 6, 7, and 9). Of these cases, case 6 was excluded because of normal OV/BV; cases 7 and 9 were determined as SSBT.
Because reference data were different depending on patients’ ages, we were unable to statistically compare raw data between the 2 groups. The z-value was calculated based on the reference data for each parameter (except OV/TV) and the statistical analysis was performed between the subtrochanteric and diaphyseal groups. Significant differences were subsequently determined in OV/BV (–3.2 ± 1.7 in subtrochanteric group vs –0.58 ± 0.68 in diaphyseal group, p = 0.029) and O.Th (–3.8 ± 0.92 in subtrochanteric group vs –2.3 ± 0.44 in diaphyseal group, p = 0.029). No significant difference was detected between the 2 groups (data not shown) for the other parameters, including bone volume parameters and bone resorption parameters.
Lateral femoral bowing
Lateral femoral bowing was evaluated in 4 cases from the subtrochanteric group (cases 2, 3, 4, and 5) and for 3 cases in the diaphyseal group (cases 7, 8, and 9) on the contralateral non-fractured side. Lateral femoral bowing was positive (61-94%) in 5/7 cases. Of these, 2 cases belonged to the subtrochanteric group, and 3 cases were within the diaphyseal group. In cases 2 and 3, lateral femoral bowing was not detected (48% and 35%, respectively) (Table 5). No significant difference was detected in the degree of lateral femoral bowing between the two groups (p = 0.114) (Table 3).
Discussion
In our case series, all the subtrochanteric cases were treated with alendronate. On the contrary, diaphyseal cases were treated with different bisphosphonate such as risedronate, minodronate, and alendronate. Actually, the number of reported cases of atypical femoral fractures treated with minodronate is very low. It was reported that there were only 3 cases out of 38 AFFs that were treated with minodronate (Hyodo et al. 2017). In mouse femora, minodronate accumulates in bone underneath osteoblasts rather than under osteoclasts and minodronate-coated bone matrix is resistant to osteoclastic resorption, suggesting bone-preserving effect by examining through isotope microscopy (Hongo et al. 2016). In our study, case 8 was treated with minodronate for 4.1 years following with alendronate for 1.3 years and ES/BS in case 8 (3.19%) was not suppressed.
GC use is associated a higher incidence of AFFs. Girgis et al. (2010) reported that GC therapy > 6 months and serum 25-OH-D levels < 16 ng/mL are risk factors for AFFs. In a series of 10 patients with 14 AFFs, Saita et al. (2015) reported that taking BPs and GCs, as well as having collagen disease are risk factors for AFFs. However, two reports have indicated no association between the occurrence of AFFs and a low 25-OH-D level or PSL dose (Schilcher et al. 2011; Feldstein et al. 2012). To the best of our knowledge, this is the first report indicating that higher doses of PSL and lower concentrations of serum 25-OH-D are associated with subtrochanteric fractures rather than diaphyseal fractures in cases of AFFs.
GCs have been shown to decrease trabecular bone formation and promote osteoclastic function in mice (Shi et al. 2015). Lower 25-OH-D levels were significantly associated with increased OV/BV (osteoid formation) in an evaluation of the iliac bone in 675 cases, because mineralization was impaired (Priemel et al. 2010). In the current study, a significantly increased duration of GC use and lower 25-OH-D levels were found in the subtrochanteric group, compared with the diaphyseal group. These two factors were conflicting for bone formation. In addition, osteoid parameters were lower than the reference values in most cases. The reason for this finding remains unknown.
Hyodo et al. (2017) reported a significant association between coronal bowing and middle fracture locations (diaphyseal), suggesting that the femoral geometry tends to affect the risk for the incidence of diaphyseal AFFs. Sasaki et al. (2012) also reported that the femoral curvature may be a causative factor for low-energy diaphyseal femoral fractures. Tsuchie et al. (2016) reported that a low 25-OH-D level is significantly associated with a curved femur (anterior and lateral bowing). They demonstrated that the average 25-OH-D concentration was 16.4 ng/mL in patients with a curved femur; however, this is inconsistent with our data. A possible reason for this difference is that the patients from our case series differed from those investigated by Tsuchie et al. (2016), as our patients had complete AFFs.
Epidemiological data have previously been reported concerning the difference in fracture sites in cases of AFFs (Schilcher et al. 2015). The subtrochanteric site was dominant in Singapore, whereas the diaphyseal site was dominant in Sweden. Furthermore, femoral bowing was associated with a diaphyseal fracture. In one report, this dichotomy was speculated to be due to cultural differences that can influence physical activity (Schilcher et al. 2015). In our study, lateral bowing results were in accordance with this previous report, although no significant difference was found.
Odvina et al. (2005) reported that all the 9 patients with a history of long-term alendronate use (3-8 years) they evaluated had SSBT. However, not all patients had SSBT in our study. Longer term BP use did not result in SSBT, because the ES/BS values of cases 2 and 4, in which the duration of BP use was > 8 years, were higher than the reference value. However, patients with SSBT in the D group had used BP for a shorter duration (< 2 years). Our data suggest that the incidence of AFF is not associated with SSBT, although our case series is based on data from only 9 patients (10 fractures).
In addition, osteoid parameters, including osteoid volume and trabecular thickness, were significantly lower in the subtrochanteric group than in diaphyseal group, suggesting that bone formation is more influenced in the subtrochanteric region of atypical femoral fractures.
We acknowledge several limitations in our study: 1) a small number of cases were included; 2) the variation of the patient age was quite wide in the subtrochanteric group, and 3) since no tetracycline labeling was used, dynamic parameters (such as the mineral apposition rate) could not be evaluated.
Further investigation is warranted to determine the detailed pathogenic mechanism of AFFs, such as the histology of the fracture sites, by evaluating the accumulation of microdamage, and analyze the association between iliac bone histology and fracture site histology and the association between the histology and femoral geometry.
In conclusion, not all patients had SSBT during the evaluation of iliac bone histomorphometry; therefore, the association between SSBT and the incidence of AFFs is not clear. Bone formation parameters, including osteoid volume and trabecular thickness, were significantly lower in the subtrochanteric group than those in diaphyseal group. Therefore, the pathogenic mechanism was different between them. The daily dose of PSL was higher, serum 25-OH-D levels were lower, and patients were younger in subtrochanteric group, compared with those in diaphyseal group.
Acknowledgments
We thank Dr. Hideaki E. Takahashi and Mr. Taketoshi Shimakura, Niigata Bone Science Institute, for their supervision and technical assistance. We also appreciate Editage (www.editage.jp) for English language editing.
This work was supported by Japan Osteoporosis Foundation (The 10th Lilly Research Grant Program, research about bone region in 2014).
Conflict of Interest
The authors declare no conflict of interest.
References
-
Black,
D.M.,
Cummings,
S.R.,
Karpf,
D.B.,
Cauley,
J.A.,
Thompson,
D.E.,
Nevitt,
M.C.,
Bauer,
D.C.,
Genant,
H.K.,
Haskell,
W.L.,
Marcus,
R.,
Ott,
S.M.,
Tomer,
J.C.,
Quandt,
S.A.,
Reiss,
T.F. &
Ensrud,
K.E.
(1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet, 348, 1535-1541.
-
Ettinger,
B.,
Burr,
D.B. &
Ritchie,
R.O.
(2013) Proposed pathogenesis for atypical femoral fractures: lessons from materials research. Bone, 55, 495-500.
-
Feldstein,
A.C.,
Black,
D.,
Perrin,
N.,
Rosales,
A.G.,
Friess,
D.,
Boardman,
D.,
Dell,
R.,
Santora,
A.,
Chandler,
J.M.,
Rix,
M.M. &
Orwoll,
E.
(2012) Incidence and demography of femur fractures with and without atypical features. J. Bone Miner. Res., 27, 977-998.
-
Fujimaki,
Y.,
Kanekasu,
S.,
Honjo,
S. &
Nakata,
O.
(2002) Radiographic analysis of the lateral bowing femur. Kansetsugeka, 21, 1144-1151.
-
Girgis,
C.M.,
Sher,
D. &
Seibel,
M.J.
(2010) Atypical femoral fractures and bisphosphonate use. N. Engl. J. Med., 362, 1848-1849.
-
Hongo,
M.,
Sasaki,
M.,
Kobayashi,
S.,
Hasegawa,
T.,
Yamamoto,
T.,
Tsuboi,
K.,
Tsuchiya,
E.,
Nagai,
T.,
Khadiza,
N.,
Abe,
M.,
Kudo,
A.,
Oda,
K.,
Henrique Luiz de Freitas,
P.,
Li,
M.,
Yurimoto,
H. &
Amizuka,
N.
(2016) Localization of minodronate in mouse femora through isotope microscopy. J. Histochem. Cytochem., 64, 601-622.
-
Hyodo,
K.,
Nishino,
T.,
Kamada,
H.,
Nozawa,
D.,
Mishima,
H. &
Yamazaki,
M.
(2017) Location of fractures and the characteristics of patients with atypical femoral fractures: analyses of 38 Japanese cases. J. Bone Miner. Metab., 35, 209-214.
-
Mashiba,
T.,
Turner,
C.H.,
Hirano,
T.,
Forwood,
M.R.,
Johnston,
C.C. &
Burr,
D.B.
(2001) Effects of suppressed bone turnover by bisphosphonates on microdamage accumulation and biomechanical properties in clinically relevant skeletal sites in beagles. Bone, 28, 524-531.
-
Meier,
R.P.,
Perneger,
T.V.,
Stern,
R.,
Rizzoli,
R. &
Peter,
R.E.
(2012) Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch. Intern. Med., 172, 930-936.
-
Odvina,
C.V.,
Zerwekh,
J.E.,
Rao,
D.S.,
Maalouf,
N.,
Gottschalk,
F.A. &
Park,
C.Y.
(2005) Severely suppressed bone turnover: a potential complication of alendronate therapy. J. Clin. Endocrinol. Metab., 90, 1294-1301.
-
Priemel,
M.,
von Domarus,
C.,
Klatte,
T.O.,
Kessler,
S.,
Schlie,
J.,
Meier,
S.,
Proksch,
N.,
Pastor,
F.,
Netter,
C.,
Streichert,
T.,
Püschel,
K. &
Amling,
M.
(2010) Bone mineralization defects and vitamin D deficiency: histomorphometric analysis of iliac crest bone biopsies and circulating 25-hydroxyvitamin D in 675 patients. J. Bone Miner. Res., 25, 305-312.
-
Recker,
R.R.,
Kimmel,
D.B.,
Parfitt,
A.M.,
Davies,
K.M.,
Keshawarz,
N. &
Hinders,
S.
(1988) Static and tetracycline-based bone histomorphometric data from 34 normal postmenopausal females. J. Bone Miner. Res., 3, 133-144.
-
Saita,
Y.,
Ishijima,
M.,
Mogami,
A.,
Kubota,
M.,
Baba,
T.,
Kaketa,
T.,
Nagao,
M.,
Sakamoto,
Y.,
Sakai,
K.,
Homma,
Y.,
Kato,
R.,
Nagura,
R.,
Miyagawa,
K.,
Wada,
T.,
Liu,
L., et al.
(2015) The incidence of and risk factors for developing atypical femoral fractures in Japan. J. Bone Miner. Metab., 33, 311-318.
-
Saito,
M.,
Mori,
S.,
Mashiba,
T.,
Komatsubara,
S. &
Marumo,
K.
(2008) Collagen maturity, glycation induced-pentosidine, and mineralization are increased following 3-year treatment with incadronate in dogs. Osteoporos. Int., 19, 1343-1354.
-
Sasaki,
S.,
Miyakoshi,
N.,
Hongo,
M.,
Kasukawa,
Y. &
Shimada,
Y.
(2012) Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: a case series. J. Bone Miner. Metab., 30, 561-567.
-
Schilcher,
J.,
Howe,
T.S.,
Png,
M.A.,
Aspenberg,
P. &
Koh,
J.S.
(2015) Atypical fractures are mainly subtrochanteric in Singapore and diaphyseal in Sweden: a cross-sectional study. J. Bone Miner. Res., 30, 2127-2132.
-
Schilcher,
J.,
Michaëlsson,
K. &
Aspenberg,
P.
(2011) Bisphosphonate use and atypical fractures of the femoral shaft. N. Engl. J. Med., 364, 1728-1737.
-
Shane,
E.,
Burr,
D.,
Abrahamsen,
B.,
Adler,
R.A.,
Brown,
T.D.,
Cheung,
A.M.,
Cosman,
F.,
Curtis,
J.R.,
Dell,
R.,
Dempster,
D.W.,
Ebeling,
P.R.,
Einhorn,
T.A.,
Genant,
H.K.,
Geusens,
P.,
Klaushofer,
K., et al.
(2014) Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J. Bone Miner. Res., 29, 1-23.
-
Shane,
E.,
Burr,
D.,
Ebeling,
P.R.,
Abrahamsen,
B.,
Adler,
R.A.,
Brown,
T.D.,
Cheung,
A.M.,
Cosman,
F.,
Curtis,
J.R.,
Dell,
R.,
Dempster,
D.,
Einhorn
T.A.,
Genant,
H.K.,
Geusens,
P.,
Klaushofer,
K., et al.
(2010) Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J. Bone Miner. Res., 25, 2267-2294.
-
Shi,
J.,
Wang,
L.,
Zhang,
H.,
Jie,
Q.,
Li,
X.,
Shi,
Q.,
Huang,
Q.,
Gao,
B.,
Han,
Y.,
Guo,
K.,
Liu,
J.,
Yang,
L. &
Luo,
Z.
(2015) Glucocorticoids: dose-related effects on osteoclast formation and function via reactive oxygen species and autophagy. Bone, 79, 222-232.
-
Somford,
M.P.,
Draijer,
F.W.,
Thomassen,
B.J.,
Chawassienx,
P.M.,
Boivin,
G. &
Papalolaus,
S.E.
(2009) Bilateral fractures of femur diaphysis in a patient with rheumatoid arthritis on long-term treatment with alendronate: clues to the mechanism of increased bone fragility. J. Bone Miner. Res., 24, 1736-1740.
-
Takakubo,
Y.,
Ohta,
D.,
Ishi,
M.,
Ito,
J.,
Oki,
H.,
Naganuma,
Y.,
Uno,
T.,
Sasaki,
A.,
Akabane,
T.,
Dairaku,
K.,
Goto,
S.,
Goto,
Y.,
Kanauchi,
Y.,
Kobayashi,
S.,
Nakajima,
T., et al.
(2017) The incidence of atypical femoral fracture in patients with rheumatic disease: Yamagata prefectural committee of atypical femoral fractures (YamaCAFe) Study. Tohoku J. Exp. Med., 242, 327-334.
-
Tamminen,
I.S.,
Yli-Kyyny,
T.,
Isaksson,
H.,
Turunen,
M.J.,
Tong,
X.,
Jurvelin,
J.S. &
Kröger,
H.
(2013) Incidence and bone biology findings of atypical femoral fractures. J. Bone Miner. Metab., 31, 585-594.
-
Tsuchie,
H.,
Miyakoshi,
N.,
Kasukawa,
Y.,
Senma,
S.,
Narita,
Y.,
Miyamoto,
S.,
Hatakeyama,
Y.,
Sasaki,
K. &
Shimada,
Y.
(2016) Factors related to curved femur in elderly Japanese women. Ups. J. Med. Sci., 121, 170-173.
-
Visekruna,
M.,
Wilson,
D. &
Mckiernan,
F.E.
(2008) Severely suppressed bone turnover and atypical skeletal fragility. J. Clin. Endocrinol. Metab., 93, 2948-2952.