Abstract
Health care disparities among people with schizophrenia is a global concern. Our previous study revealed cancer screening rates in Japanese people with schizophrenia lower than rates of approximately 40% of the general population. However, that study was based on self-reports, which can be inaccurate, and rates did not differentiate the types of cancer screening provider (i.e., municipal screening, collective opportunistic screening, and individual opportunistic screening). This study aimed to investigate records-based cancer screening rates, focusing on participation rates of people with schizophrenia who are subject to municipal cancer screening programs. We conducted a cross-sectional study at a psychiatric hospital outpatient clinic from September to November 2016. We randomly extracted 420 potential participants from among 680 eligible patients and asked them to participate. We then selected subgroups of participants living in Okayama city who were enrolled in the National Health Insurance or Public Assistance systems and were subject to colorectal, gastric, lung, breast, or cervical cancer screening provided by Okayama city (n = 97, 96, 97, 42, and 64, respectively). Participation in cancer screenings was assessed based on local government records. Municipal cancer screening rates were as follows: 13.4% (95% confidence interval: 6.6%-20.2%) for colorectal, 7.3% (2.1%-12.5%) for gastric, 16.5% (9.1%-23.9%) for lung, 21.4% (9.0%-33.8%) for breast, and 14.1% (5.6%-22.6%) for cervical cancers. The findings demonstrated extremely low cancer screening rates among people with schizophrenia subject to municipal cancer screenings in Japan. A strategy to promote municipal cancer screening for people with schizophrenia is needed.
Introduction
People with schizophrenia have a substantially greater risk of cancer mortality compared with the general population or people without schizophrenia (Zhuo et al. 2017). One of the causes of the disparity in cancer mortality among people with schizophrenia may be delays in diagnosis (Chou et al. 2016). Research shows that people with schizophrenia are more likely to have advanced cancer on first admission than people without psychiatric disorders (Ishikawa et al. 2016). Therefore, early detection of cancer in this population is an important public health issue.
Most previous studies on cancer screening participation among people with schizophrenia have found low cancer screening rates, including for breast (Dickerson et al. 2003; Lindamer et al. 2003; Chochinov et al. 2009; Jensen et al. 2016; Woodhead et al. 2016), cervical (Dickerson et al. 2003; Lindamer et al. 2003; Carney and Jones 2006; Martens et al. 2009; Lin et al. 2010; Abrams et al. 2012; Woodhead et al. 2016), and colorectal cancer screening (Kodl et al. 2010). However, most of these studies have been conducted in North America and Europe. There are few studies on this issue in Asia, even when including studies of individuals with mental illness not restricted to schizophrenia (Lin et al. 2010; Mo et al. 2014; Yen et al. 2015), and there are no studies on gastric and lung cancer screening among people with schizophrenia. We recently reported that outpatients with schizophrenia are less likely to participate in nationally recommended cancer screening (colorectal, gastric, lung, breast, and cervical cancer screening) than the general population (Fujiwara et al. 2017). These cancer screening rates in people with schizophrenia were approximately one-half the rates of nearly 40% of the general population. However, a limitation of our previous study is that participation in cancer screening was measured using self-report questionnaires, which can be inaccurate (Rauscher et al. 2008). Therefore, record-based studies are needed to confirm previous findings in Japan.
In addition, our previous study calculated cancer screening rates without differentiating between types of provider (i.e., municipal cancer screening, collective opportunistic cancer screening subsidized by insurers, and individual opportunistic screening), each of which promote cancer screening using different strategies and target different populations. Municipal cancer screening programs in Japan are aimed mainly at unemployed people, employees of small- to medium-sized companies, and self-employed people. This type of cancer screening program offers a major cancer screening opportunity for people with schizophrenia who have varying degrees of occupational disability. Therefore, it is especially important to investigate participation in municipal cancer screening by people with schizophrenia, to develop strategies to increase cancer screening rates in this population.
A few previous studies have reported factors related to non-participation in cancer screening in people with schizophrenia worldwide (Carney and Jones 2006; Chochinov et al. 2009; Martens et al. 2009). Our previous study found associations between social or physical factors and cancer screening non-participation in Japan (Fujiwara et al. 2017). We found that symptom severity and functional disability related to schizophrenia were the most consistent risk factors for a lack of participation in screenings for all types of cancer.
The objectives of the present study were (i) to obtain accurate cancer screening rates among people with schizophrenia subject to municipal cancer screening programs and (ii) to describe differences in screening rates between people with schizophrenia with severe disability and those with mild to moderate disability.
Methods
Study design and setting
This study was a preplanned preliminary subgroup analysis of data from the Study of Health Behavior in People with Schizophrenia (SHEAPS), which has been registered in a clinical trial registry (UMIN000023874). SHEAPS is a cross-sectional study with two related aims: to investigate cancer screening behaviors and to study smoking behaviors in patients with schizophrenia. We have previously described the study methods in detail (Fujiwara et al. 2017) and include methodogical details here. SHEAPS participants were recruited in an outpatient clinic at the Okayama Psychiatric Medical Center in Japan. This hospital is the core public psychiatric hospital in Okayama Prefecture and is located in the city center.
Participants
The analysis in the present study was performed among a subgroup of participants in SHEAPS. We extracted eligible participants for this subgroup analysis, as described below. We focused on cancer screening rates among individuals who were enrolled in the National Health Insurance (NHI) or Public Assistance (PA) systems. This subgroup is subject to municipal cancer screening programs rather than collective opportunistic cancer screening subsidized by employee-based health insurers. The NHI covers unemployed people, self-employed people, and employees of small- to medium-sized companies. For the present subgroup analysis, we selected participants who lived in Okayama city and who were enrolled in the NHI or PA; thus, we accessed municipal cancer screening records with the permission of participants, as detailed below.
As described previously (Fujiwara et al. 2017), the SHEAPS inclusion criteria were as follows: on April 1, 2016, (i) patients aged 20-69 years; (ii) those who had visited the Okayama Psychiatric Medical Center for 1 or more years, and had visited the hospital twice or more in the last 6 months as their primary psychiatric outpatient service; and (iii) those who had been diagnosed by their primary psychiatrist with schizophrenia or schizoaffective disorder, but not other schizophrenia spectrum disorders, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (American Psychiatric Association 2013). The exclusion criteria were as follows: (i) patients comorbid for intellectual disabilities and unable to answer the questionnaire; (ii) those with psychiatric symptoms too severe to make study participation appropriate (as judged by their primary psychiatrist); (iii) those incapable of study participation because their physical status was too severe (as judged by their primary psychiatrist); and (iv) those unable to read or write in Japanese.
A total 680 patients were eligible for SHEAPS. Of these, 420 patients were randomly extracted in August 2016 using computer-generated randomization. The number of participants was set according to the available resources in the setting. Potential participants were asked to participate in SHEAPS from September to November 2016. We contacted most participants during their outpatient clinic visits. We also used telephone and mail to approach potential participants who could not be contacted at clinic visits. For this preplanned subgroup analysis in SHEAPS, we obtained permission from participants eligible for this subgroup analysis to examine their municipal cancer screening records registered in the municipal database.
In the present subgroup analyses of participation in screening for each type of cancer, we excluded individuals with a history of that cancer (e.g., the analysis of gastric cancer screening behavior excluded patients with a history of gastric cancer but included those with a history of other cancers).
Outcomes
The primary outcome was municipal cancer screening rates. The secondary outcome was stratified rates by symptom severity/functional disability.
Data source and measurements
Sex, age, and health insurance data were obtained from medical records. Educational level, employment status, marital status, and the presence or absence of current visits to other outpatient clinics for physical illness were based on self-report questionnaires. Participants completed the questionnaires with the help of researchers (M.I, and M.F., both psychiatrists) and a trained research assistant (a licensed nurse).
Cancer screening
In Okayama city, screening for different types of cancer, recommended by the Ministry of Health, Labour and Welfare, was provided in the municipal cancer screening programs, as follows: fecal occult blood testing, upper gastrointestinal X-ray with barium, annual chest X-ray for people aged 40 years or older, mammography for women aged 40 years or older every 2 years, and Pap smear test for women aged 20 years or older every 2 years. For breast cancer screening, Okayama city provided a breast screening program consisting of mammography combined with clinical breast examination (CBE). Contrary to recommendations, some screening participants only received CBE for breast cancer screening.
We examined participants’ records of participation in cancer screening programs, obtained from the Okayama City Health Center. We used records of participation in colorectal, gastric, and lung cancer screening for the previous year (2015 fiscal year), and participation in breast and cervical cancer screening for the previous 2 years (2014-2015 fiscal years). The breast cancer screening records classified individuals who received only CBE as receiving breast cancer screening. We submitted the list of participants (including participant’s name, date of birth, address, and study ID) to the Okayama City Health Center, who subsequently linked the participant list with cancer screening records and then returned the list, after excluding personally identifiable information.
Symptom severity and functional disability
Each patient’s primary psychiatrist assessed patient symptom severity and functional disability using the modified Global Assessment of Functioning (mGAF) (Hall 1995). The mGAF is a numeric scale with a score range of 1-100; a higher score reflects higher functioning. The mGAF scores are based on psychological, social, and occupational functioning. The Japanese version of the mGAF has good reliability and validity (Eguchi et al. 2015). We used mGAF scores for the best month in the last year. We classified individuals with scores of 50 or less as having severe dysfunction (Ruggeri et al. 2000). For example, patients who score 41-50 have serious symptoms or impairment in functioning, e.g., they are unable to keep a job or stay in school, or they fail at school, or are unable to care for their house and family.
Sample size
SHEAPS was an exploratory survey. We planned to sample 420 participants, which was the largest sample possible given our resources, drawn by random sampling from pooled eligible SHEAPS participants. We extracted all eligible samples in SHEAPS for the current study analysis.
Ethical approval
SHEAPS complied with the Declaration of Helsinki and was approved by the institutional ethics committee at the Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences and Okayama University Hospital (approval number KEN1608-010), and by Okayama Psychiatric Medical Center (approval number 27-38). Potential participants were informed that they could decline to participate or withdraw from the study at any time, and those who agreed to participate provided their written informed consent. In addition, participants who met the criteria for the current analyses also provided written informed consent to examine their records of participation in cancer screening programs from the Okayama City Health Center.
Statistical analysis
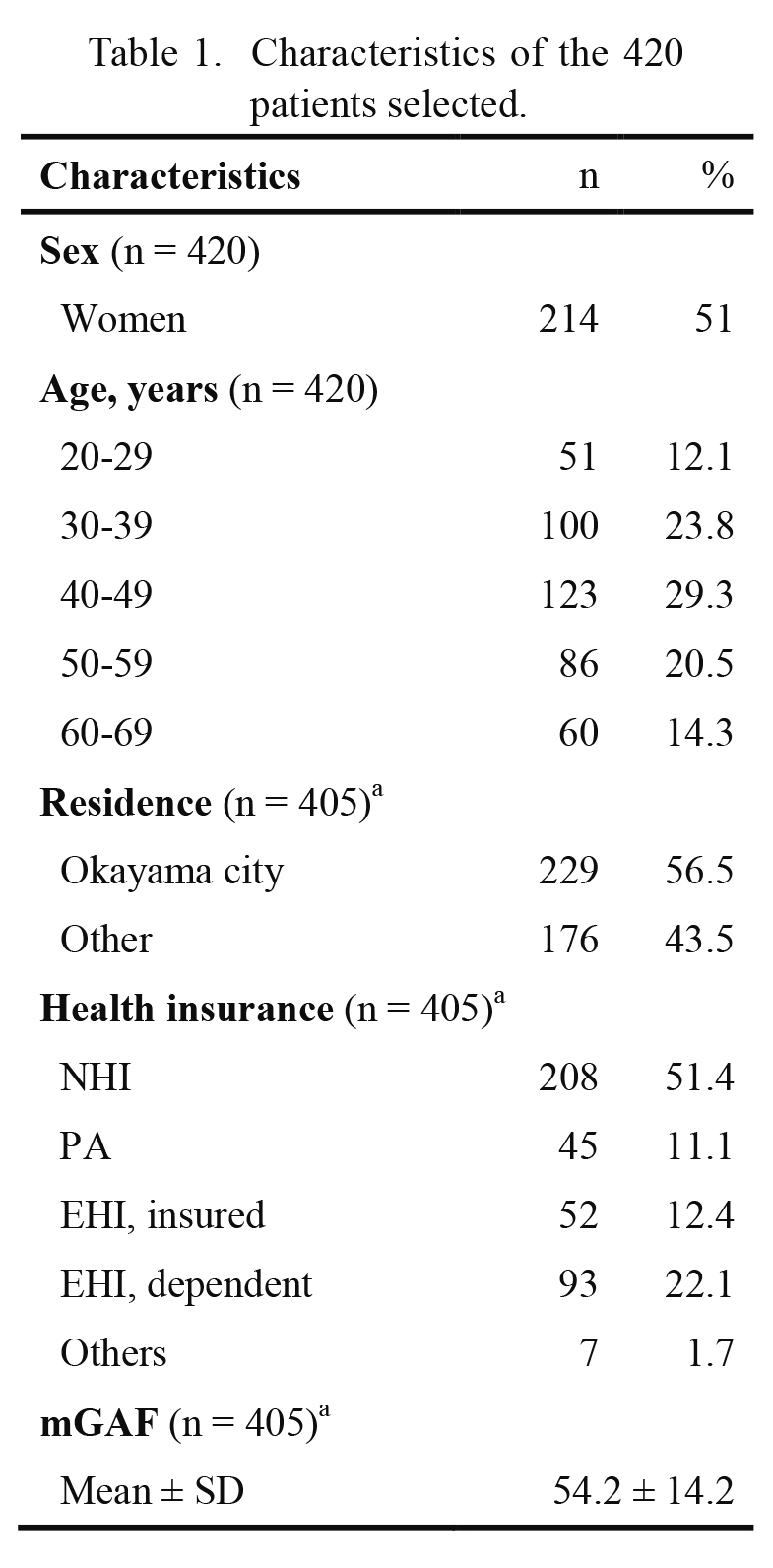
Data were analyzed using SPSS Version 22 (IBM Tokyo, Japan). We described the participant characteristics in screenings for each type of cancer (Table 1). We calculated cancer screening rates and 95% confidence intervals (CIs) for each cancer screening site. In addition, we calculated the stratified rates by symptom severity/functional disability, as assessed by the mGAF (“mild to moderate disability” vs. “severe disability”).
Results
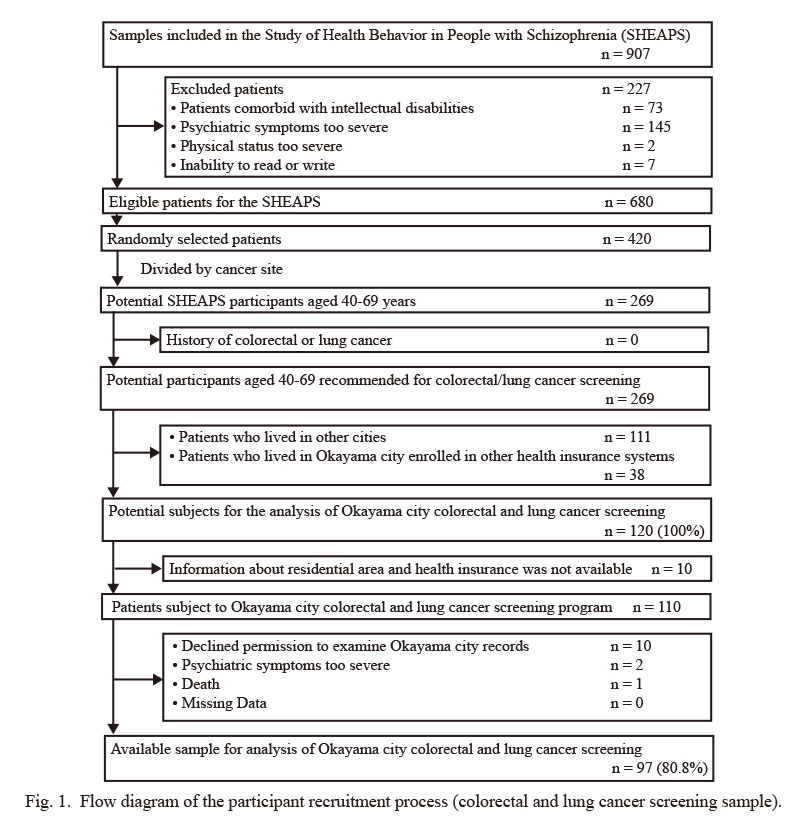
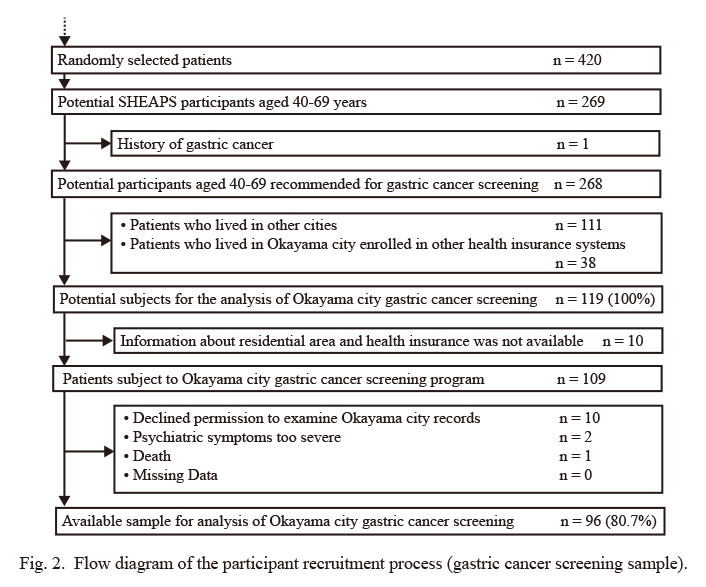
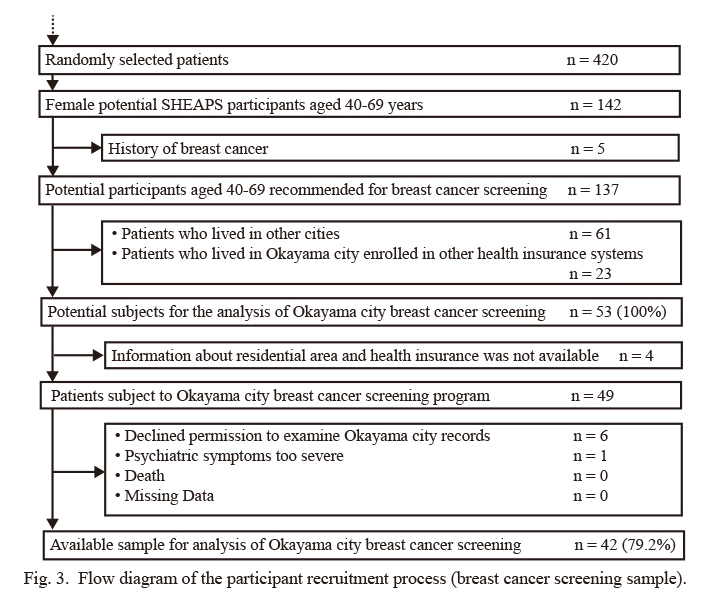
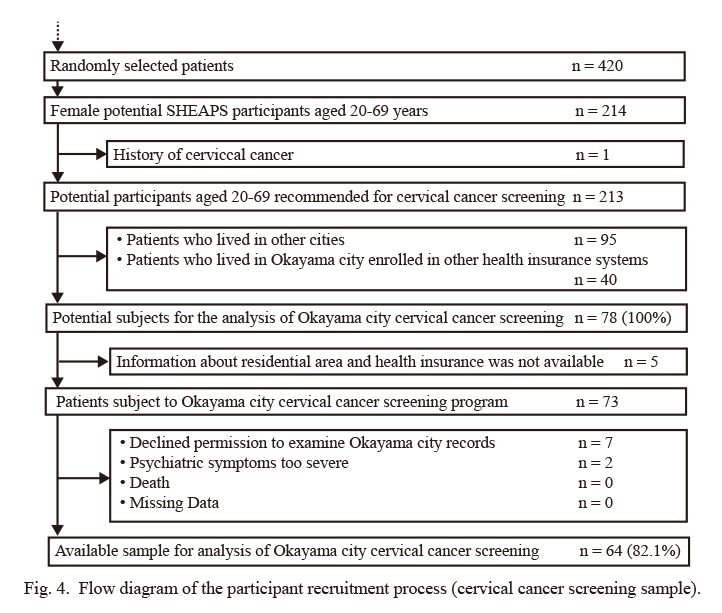
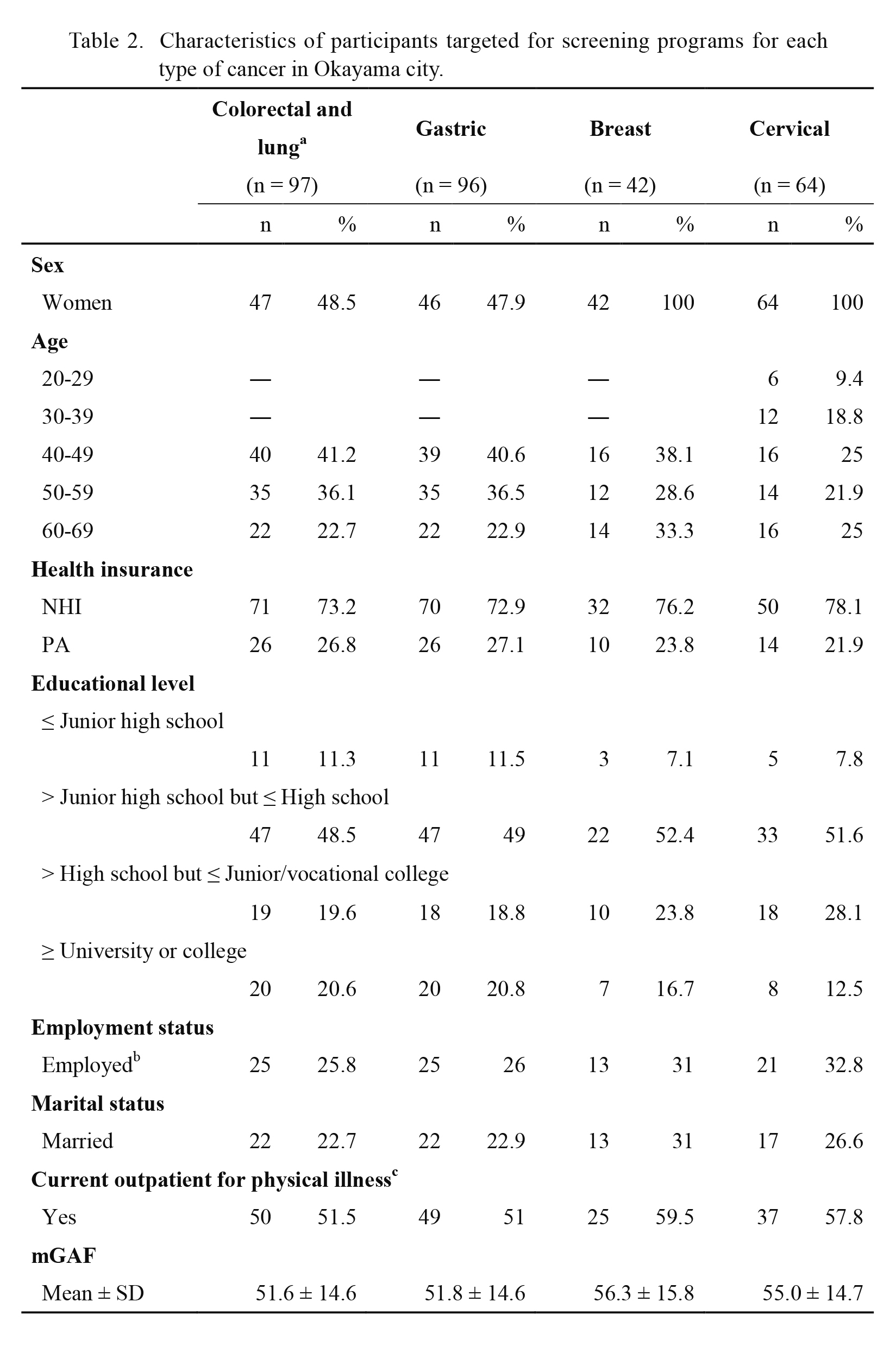
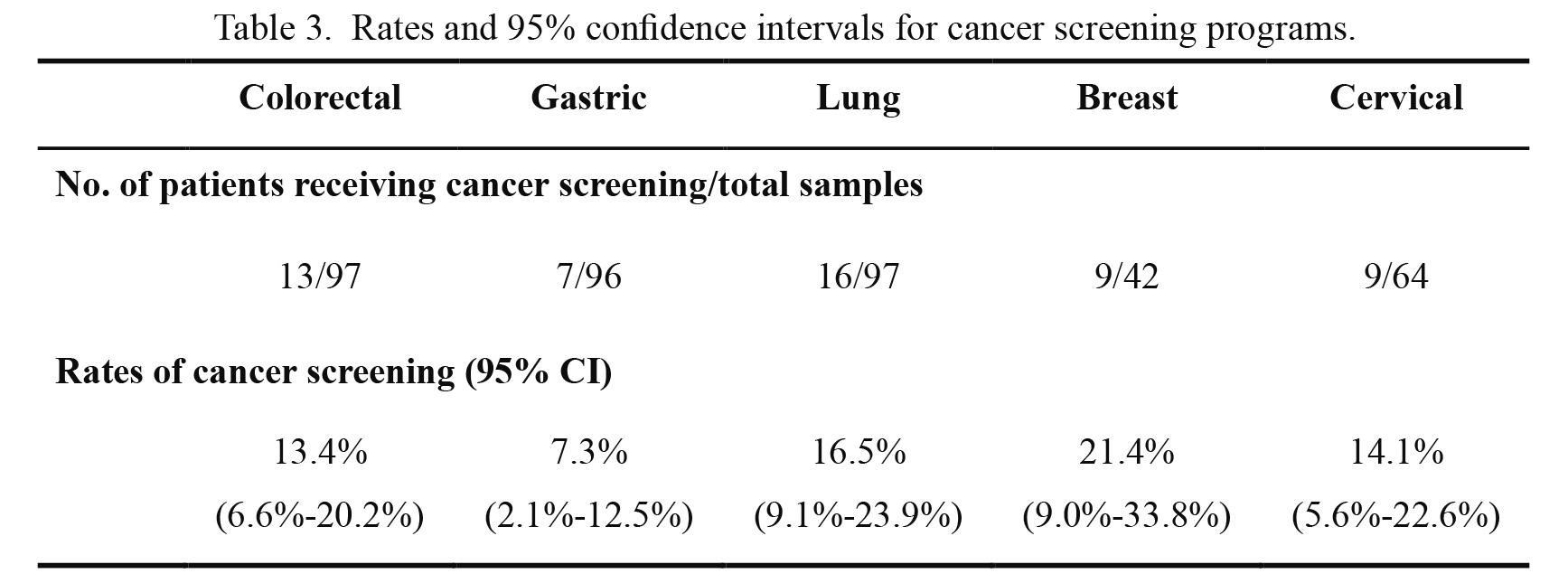
The study recruitment process is shown in Figs. 1, 2, 3 and 4. Table 1 shows the characteristics of the 420 patients selected. Among these patients, 51.0% were women, the average age was 44.8 years, and 62.2% were enrolled in NHI or PA. Among the 260 patients who were not selected, 51.5% were women, the average was 44.0 years, and 68.5% were enrolled in NHI or PA. There were no significant differences in these variables between the selected and non-selected patients (data not shown). Data were analyzed for 97 participants who were subject to colorectal and lung cancer screening, 96 participants subject to gastric cancer screening, 42 participants subject to breast cancer screening, and 64 participants subject to cervical cancer screening (e.g., female patients aged 50 years were subject to all five cancer screenings); study participation rates were 80.8%, 80.7%, 79.2%, and 82.1%, respectively. Table 2 shows the background characteristics of participants in the four groups. Table 3 shows rates and 95% CIs for cancer screening programs. Of the five types of cancer, the breast cancer screening rate was the highest, although the rate was only 21.4% (95% CI: 9.0%-33.8%). The lowest screening rate was 7.3% (95% CI: 2.1%-12.5%) for gastric cancer.
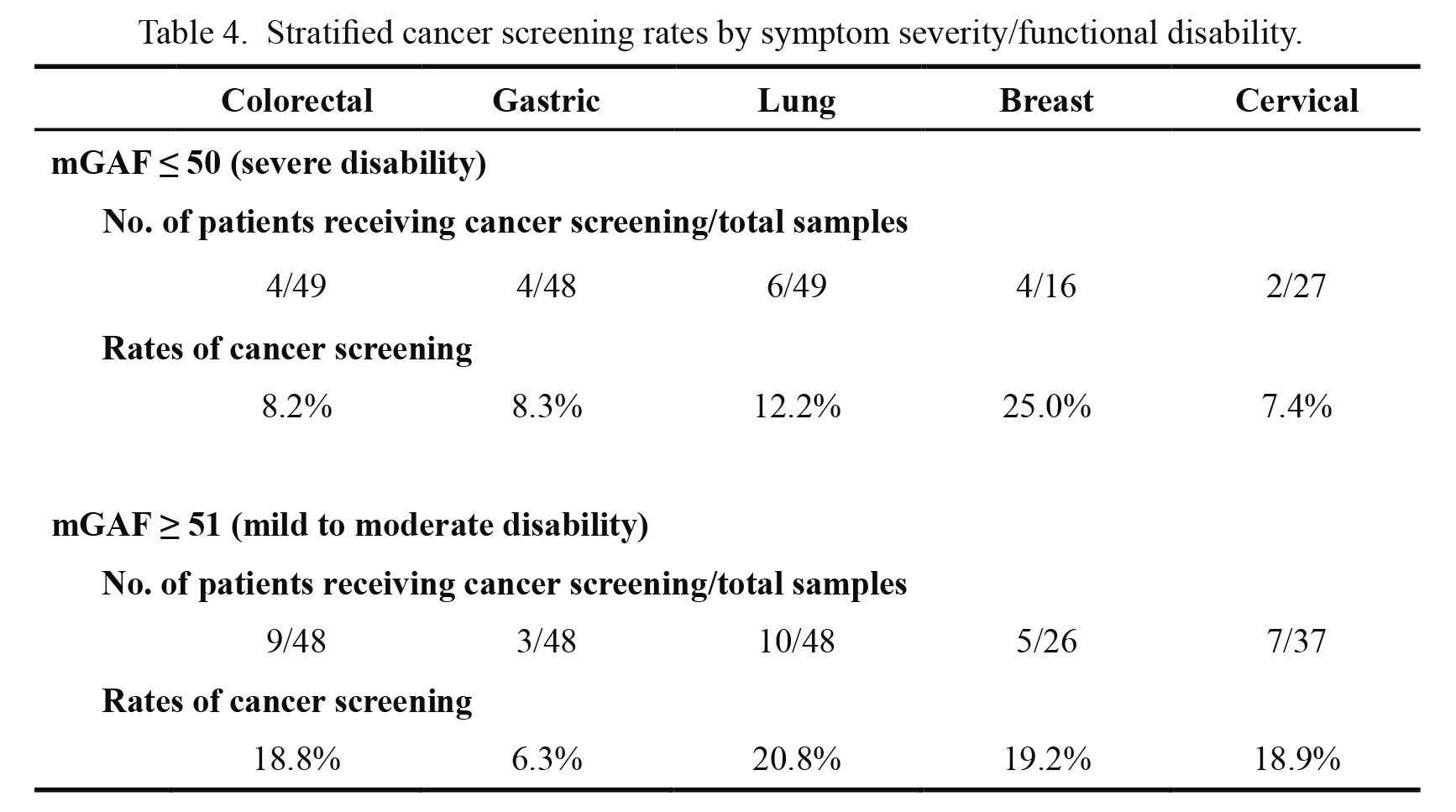
Table 4 shows the stratified rates by symptom severity/functional disability. Because the number of stratified samples was small, we did not perform any statistical tests of the difference in screening rates between patients with severe disability and those with mild to moderate disability. However, the screening rates for colorectal, lung, and cervical cancer in patients with severe disability were approximately one-half the cancer screening rates in those with mild to moderate disability.
Discussion
The present findings showed that only one-fifth or fewer outpatients with schizophrenia subject to municipal cancer screening programs received cancer screenings. Although the 95% CIs of cancer screening rates were wide because of the small sample size, the upper limits of CIs were 12.5% (gastric cancer) to 33.8% (breast cancer). Even the upper limits were lower than the recommended target rate of 50%, as discussed below. To the best of our knowledge, this is the first study to report local government record-based cancer screening rates among people with severe mental illness in Japan.
Our previous study showed that the self-reported rates of cancer screenings among schizophrenic outpatients were 19.4%-30.8%, and that these rates were approximately one-half those among the general population (Fujiwara et al. 2017). These rates included any type of cancer screening, regardless of provider (municipal cancer screening, collective opportunistic cancer screening, and individual opportunistic screening). The present study extended our previous work by focusing on municipal cancer screening, and the findings revealed very low screening rates. The municipal cancer screening rates found here were lower than those found in our previous study, which included all types of cancer screening. For example, the rate for gastric municipal cancer screening was 7.3% in the present study; in contrast, this rate (including gastric screening performed by any provider) was 21.5% in the previous study. The rates may be lower in the present study for several reasons: (i) the present participants were enrolled only in the NHI or PA systems, which cover unemployed people, so this subgroup may have comprised participants who had the greatest disabilities in the previous study; (ii) the present cancer screening rates were based on cancer screening records rather than self-reports, which can overestimate screening rates (Rauscher et al. 2008). It is difficult to compare the rates for patients with schizophrenia in the present study with rates for the general population. There are no available data on municipal cancer screening rates calculated using health insurance data.
In the general population, people enrolled in the NHI or PA are at high risk of non-participation in cancer screenings (Tabuchi et al. 2012). The lower screening rates of this population may stem from complex factors, such as disparities in access to and use of cancer information, difficulty in taking time off to participate in cancer screening, and economic difficulties (Tabuchi et al. 2012). Moreover, people with schizophrenia enrolled in the NHI or PA may be at higher risk of non-participation in cancer screenings than those covered by other health insurance systems. In addition, people with schizophrenia tend to have impaired social and vocational functioning, which may result in unemployment and NHI or PA coverage. In fact, 63% of SHEAPS participants were enrolled in the NHI or PA. Therefore, it is important to target this high-risk population. Effective strategies are needed to promote cancer screening for individuals with schizophrenia enrolled in the NHI or PA systems.
In the present study, point estimations of participation rates in screening for colorectal, lung, and cervical cancer among individuals with high symptom severity/functional disability were lower than for those with mild to moderate disability. The present study confirmed previous findings suggesting that patients with schizophrenia who have high levels of disability are less likely to participate in cancer screenings (Fujiwara et al. 2017). Gastric cancer screening rates were lower than 10%, regardless of disability (see Table 3: 8.3% for those with severe dysfunction vs. 6.3% for those with less severe dysfunction). Therefore, people with schizophrenia (even those with less severity/higher function) were less likely to participate in gastric cancer screening. These low screening rates may mask the influence of severity/function. One reason why the gastric cancer screening rate was much lower than the screening rates for other sites in this study might be that patients tend to be hesitant about undertaking complex additional procedures before and after upper gastrointestinal X-ray itself, such as overnight fasting and laxative use to clear the barium. In addition, some patients with schizophrenia who had chronic constipation, which is a common side effect of antipsychotics (De Hert et al. 2011), might have not been recommended for upper gastrointestinal X-ray with barium because chronic dysmotility related to drug effects is a factor contributing to intestinal obstruction from inspissated barium (barolith) (Kurer et al. 2008); however, this remains unclear. Strong support and careful consideration may be needed to encourage patients with schizophrenia to receive upper gastrointestinal X-ray with barium.
In contrast, the point estimation of the breast cancer screening participation rate for individuals with high disability was paradoxically higher than for those with mild to moderate disability. Compared with sample sizes for the analyses of other cancer screening rates in the present study, the sample for analysis of the breast cancer screening rate was much smaller (only 16 patients with severe disability and 26 with mild to moderate disability); this may have resulted in increased error. Therefore, the association between disability and cancer screening participation found here was unclear, especially for breast cancer screening. Further investigation is needed to confirm these findings.
The cancer screening rates for the present samples were substantially lower than the recommended targets of the Basic Plan to Promote Cancer Control Programs of Japan, which are 50% or more. Taken together with our previous findings (Fujiwara et al. 2017), the present results indicate a need to develop proactive behavioral interventions to increase cancer screenings rates among people with schizophrenia. Because people with schizophrenia use municipal mental health services, including the Payment for Services and Supports for Persons with Disabilities, local governments can encourage the promotion of cancer screening within these services. In addition, outpatient clinics could be ideal places for individual interventions. For an appropriate individual approach, it is desirable to establish a system to encourage patient participation in cancer screening that is based on an accurate record of such participation rather than self-reporting (Rauscher et al. 2008) because people with schizophrenia might not understand cancer screening and might not accurately recall their cancer screening participation history.
The present study had several limitations. First, the small sample sizes for the preliminary subgroup analyses make it difficult to draw firm conclusions from the findings. Second, participants were limited to residents of Okayama city and recruited from a single outpatient clinic in a psychiatric hospital; it is unclear whether our results are generalizable to people with schizophrenia in different settings. Third, because the primary interest of the present study was the cancer screening rates among individuals with schizophrenia enrolled in the NHI or PA, the current findings have limited generalizability to people with schizophrenia enrolled in other types of health insurance. Fourth, some of the present participants might have been subject to individual opportunistic screening rather than municipal cancer screening programs, which could lead to underestimation of the true cancer screening rates. Fifth, patients with very severe symptoms were excluded, which might lead to overestimation of the cancer screening rates. Sixth, there was a timing gap between the mGAF ratings and participation in cancer screenings, which may have been up to 2 years for breast and cervical cancer screening. Seventh, the present study did not include patients aged over 69 years, in agreement with the policy of government statistics on cancer screening rate. Finally, the true clinical endpoint is cancer mortality among people with schizophrenia, not cancer screening rates.
In conclusion, we found extremely low cancer screening rates among individuals with schizophrenia who are subject to municipal cancer screenings in Japan. Strategies to promote municipal cancer screenings among people with schizophrenia are urgently needed.
Acknowledgments
We thank Ms. Kimiko Takaoka, a research assistant who helped to conduct the questionnaire survey; Ms. Megumi Miki for assistance with data management; Ms. Shoko Yoshimoto for continued assistance with logistics; Dr. Hiroaki Matsuoka, Dr. Tomoe Kodama, Ms. Satomi Takemoto, and Ms. Shizuko Yamamoto, who gave us kind suggestions about the study and queried the database for records of cancer screenings in the Okayama City Health Center; and all the staff of the outpatient service at the Okayama Psychiatric Medical Center. We also thank Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
This work was supported by the Okayama Health Foundation, Novartis Pharma Research Grants, Research for Promotion of Cancer Control Programs (H26-political-general-002), and JSPS KAKENHI, grant number JP17K09112.
Conflict of Interest
Dr. Inagaki reports personal fees from Pfizer, Mochida, Shionogi, Sumitomo Dainippon, Daiichi-Sankyo, Meiji Seika, Takeda, Nippon Hyoron-Sha, Nanzando, Seiwa Shoten, Igaku-shoin, and Technomics outside the submitted work. Dr. Fujiwara reports personal fees from Mochida, Sentan Igaku-Sha, Igaku-shoin, and Seiwa Shoten outside the submitted work. Dr. Fujimori reports personal fees from Mochida, Igaku-Shoin, Chugai-Igakusha, Nankodo, and Kongo-Shuppan outside the submitted work. Dr. So reports personal fees from Kagakuhyronsha, Medical Review, and Otsuka outside the submitted work. Dr. Kakeda reports personal fees from Mochida outside the submitted work. Dr. Kodama reports personal fees from Janssen, Otsuka, MSD, Eisai, Yoshitomiyakuhin, and Eli Lilly outside the submitted work. Dr. Uchitomi reports personal fees from Mochida, Eisai and other fees from QOL Co., outside the submitted work; annual fees under JPY 500,000 from companies are not disclosed. Dr. Yamada reports grants from Daiichi Sankyo, Eisai, Otsuka, Astellas, MSD, and Pfizer, and personal fees from UCB Japan, Tsumura, Sumitomo Dainippon, Daiichi-Sankyo, MSD, Pfizer, Eisai, Meiji Seika, and Mochida outside the submitted work. The remaining authors declare no conflicts of interest.
References
-
Abrams,
M.T.,
Myers,
C.S.,
Feldman,
S.M.,
Boddie-Willis,
C.,
Park,
J.,
McMahon,
R.P. &
Kelly,
D.L.
(2012) Cervical cancer screening and acute care visits among Medicaid enrollees with mental and substance use disorders. Psychiatr. Serv., 63, 815-822.
-
American Psychiatric Association
(2013) Diagnostic and Statistical Manual of Mental Disorders: Diagnostic and Statistical Manual of Mental Disorders, 5th ed., American Psychiatric Publishing, Arlington, VA.
-
Carney,
C.P. &
Jones,
L.E.
(2006) The influence of type and severity of mental illness on receipt of screening mammography. J. Gen. Intern. Med., 21, 1097-1104.
-
Chochinov,
H.M.,
Martens,
P.J.,
Prior,
H.J.,
Fransoo,
R. &
Burland,
E.
(2009) Does a diagnosis of schizophrenia reduce rates of mammography screening? A Manitoba population-based study. Schizophr. Res., 113, 95-100.
-
Chou,
F.H.,
Tsai,
K.Y.,
Wu,
H.C. &
Shen,
S.P.
(2016) Cancer in patients with schizophrenia: what is the next step? Psychiatry Clin. Neurosci., 70, 473-488.
-
De Hert,
M.,
Hudyana,
H.,
Dockx,
L.,
Bernagie,
C.,
Sweers,
K.,
Tack,
J.,
Leucht,
S. &
Peuskens,
J.
(2011) Second-generation antipsychotics and constipation: a review of the literature. Eur. Psychiatry, 26, 34-44.
-
Dickerson,
F.B.,
McNary,
S.W.,
Brown,
C.H.,
Kreyenbuhl,
J.,
Goldberg,
R.W. &
Dixon,
L.B.
(2003) Somatic healthcare utilization among adults with serious mental illness who are receiving community psychiatric services. Med. Care, 41, 560-570.
-
Eguchi,
S.,
Koike,
S.,
Suga,
M.,
Takizawa,
R. &
Kasai,
K.
(2015) Psychological symptom and social functioning subscales of the modified global assessment of functioning scale: reliability and validity of the Japanese version. Psychiatry Clin. Neurosci., 69, 126-127.
-
Fujiwara,
M.,
Inagaki,
M.,
Nakaya,
N.,
Fujimori,
M.,
Higuchi,
Y.,
Hayashibara,
C.,
So,
R.,
Kakeda,
K.,
Kodama,
M.,
Uchitomi,
Y. &
Yamada,
N.
(2017) Cancer screening participation in schizophrenic outpatients and the influence of their functional disability on the screening rate: a cross-sectional study in Japan. Psychiatry Clin. Neurosci., 71, 813-825.
-
Hall,
R.C.
(1995) Global assessment of functioning. A modified scale. Psychosomatics, 36, 267-275.
-
Ishikawa,
H.,
Yasunaga,
H.,
Matsui,
H.,
Fushimi,
K. &
Kawakami,
N.
(2016) Differences in cancer stage, treatment and in-hospital mortality between patients with and without schizophrenia: retrospective matched-pair cohort study. Br. J. Psychiatry, 208, 239-244.
-
Jensen,
L.F.,
Pedersen,
A.F.,
Bech,
B.H.,
Andersen,
B. &
Vedsted,
P.
(2016) Psychiatric morbidity and non-participation in breast cancer screening. Breast, 25, 38-44.
-
Kodl,
M.M.,
Powell,
A.A.,
Noorbaloochi,
S.,
Grill,
J.P.,
Bangerter,
A.K. &
Partin,
M.R.
(2010) Mental health, frequency of healthcare visits, and colorectal cancer screening. Med. Care, 48, 934-939.
-
Kurer,
M.A.,
Davey,
C. &
Chintapatla,
S.
(2008) Intestinal obstruction from inspissated barium (Barolith): a systematic review of all cases from 1950 to 2006. Colorectal Dis., 10, 431-439.
-
Lin,
H.C.,
Yang,
L.Y. &
Chiu,
W.T.
(2010) Cervical cancer screening of women with schizophrenia in Taiwan. Psychiatr. Serv., 61, 327-328.
-
Lindamer,
L.A.,
Buse,
D.C.,
Auslander,
L.,
Unutzer,
J.,
Bartels,
S.J. &
Jeste,
D.V.
(2003) A comparison of gynecological variables and service use among older women with and without schizophrenia. Psychiatr. Serv., 54, 902-904.
-
Martens,
P.J.,
Chochinov,
H.M.,
Prior,
H.J.,
Fransoo,
R. &
Burland,
E.
(2009) Are cervical cancer screening rates different for women with schizophrenia? A Manitoba population-based study. Schizophr. Res., 113, 101-106.
-
Mo,
P.K.,
Mak,
W.W.,
Chong,
E.S.,
Shen,
H. &
Cheung,
R.Y.
(2014) The prevalence and factors for cancer screening behavior among people with severe mental illness in Hong Kong. PLoS One, 9, e107237.
-
Rauscher,
G.H.,
Johnson,
T.P.,
Cho,
Y.I. &
Walk,
J.A.
(2008) Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiol. Biomarkers Prev., 17, 748-757.
-
Ruggeri,
M.,
Leese,
M.,
Thornicroft,
G.,
Bisoffi,
G. &
Tansella,
M.
(2000) Definition and prevalence of severe and persistent mental illness. Br. J. Psychiatry, 177, 149-155.
-
Tabuchi,
T.,
Nakayama,
T. &
Tsukuma,
H.
(2012) Disparity in cancer screening rates in Japan: impact of the type of medical insurance. Japan Medical Journal, 4605, 84-88 (in Japanese).
-
Woodhead,
C.,
Cunningham,
R.,
Ashworth,
M.,
Barley,
E.,
Stewart,
R.J. &
Henderson,
M.J.
(2016) Cervical and breast cancer screening uptake among women with serious mental illness: a data linkage study. BMC Cancer, 16, 819.
-
Yen,
S.M.,
Kung,
P.T. &
Tsai,
W.C.
(2015) Mammography usage with relevant factors among women with mental disabilities in Taiwan: a nationwide population-based study. Res. Dev. Disabil., 37, 182-188.
-
Zhuo,
C.,
Tao,
R.,
Jiang,
R.,
Lin,
X. &
Shao,
M.
(2017) Cancer mortality in patients with schizophrenia: systematic review and meta-analysis. Br. J. Psychiatry, 211, 7-13.