2018 Volume 244 Issue 3 Pages 231-242
2018 Volume 244 Issue 3 Pages 231-242
Opportunistic infections (OIs) are the most significant complication of human immunodeficiency virus (HIV) infection. The prevalence of OIs differs among various countries in part due to different climates and socio-economic conditions. We, therefore, carried out the retrospective study at the Public Health Clinical Center of Chengdu, Sichuan to comprehensively investigate the prevalence of OIs, predictors of OIs, and risk factors for in-hospital death among HIV-infected patients. Sichuan in West China is characterized by the largest population living with HIV/Acquired immunodeficiency syndrome (AIDS) across China. In total, we reviewed 954 cases of HIV infection, admitted to the hospital during January 2014 to December 2015, and found that bacterial pneumonia (25.8%) was the most common OIs, followed by candida infection (18.3%), Pneumocystis jiroveci pneumonia (11.9%), tuberculosis (11.5%), infectious diarrhoea (9.3%), cryptococcus infection (7.3%), cytomegalovirus infection (4.9%), toxoplasmosis (4.6%), hepatitis C (4.0%), nontuberculous mycobacteria desease (2.2%) and Penicillium marneffei infection (0.3%). We also found two strongest risk factors for in-hospital mortality: CD4+T cell counts of less than 100 cells/μL and not receiving antiretroviral therapy. Moreover, the study revealed the specific pathogens causing bacterial pneumonia and/or candida infection, the effect of tuberculosis on CD4+T cell counts, and the drug resistance of Mycobacterium tuberculosis among HIV-infected and non-HIV-infected patients. The present findings may aid in the clinical diagnosis and treatment of HIV-infected patients, and could help developing efficient public health strategies in China.
Acquired immunodeficiency syndrome (AIDS) is an ever-growing public health concern. Human immunodeficiency virus (HIV) has accounted for 35 million deaths worldwide, and nearly 2 million infections occurred in 2016 (Dabis and Bekker 2017). HIV infection destroys the immune system (Barré-Sinoussi et al. 1983), rendering affected people susceptible to opportunistic infections (OIs) and malignancies. Global evidence has shown that the common OIs are tuberculosis (TB), Pneumocystis jiroveci pneumonia (PCP), candida infection, cytomegalovirus infection (CMV) (Saha et al. 2011; Fenner et al. 2013; Kim et al. 2013; Katano at al. 2014; Okome-Nkoumou et al. 2014). OIs cause substantial morbidity in HIV-infected patients, leading to increased economic and social burden. HIV science should be strengthened.
In 2003, China launched the National Free Antiretroviral Treatment Program (Zhao et al. 2012). Antiretroviral therapy (ART) has decreased the incidence of OIs which shorten the life span of HIV-infected patients in the world (Antiretroviral Therapy Cohort Collaboration 2008; Zhang et al. 2011), but OIs remain a leading cause of hospitalization (Hajiabdolbaghi et al. 2014). The prevalence of OIs differs among various countries due to different climates and socio-economic conditions (Saha et al. 2011; Fenner et al. 2013; Kim et al. 2013; Katano at al. 2014; Okome-Nkoumou et al. 2014). The analysis of OIs could provide useful information related to pathogens and causes of death in HIV-infected patients. However, the prevalence and spectrum of OIs among HIV-infected patients are rarely documented in China, and only known in East China (Xiao et al. 2013; Luo et al. 2016).
There is a deleterious and synergistic interaction between TB and HIV (van Zyl Smit et al. 2010), and the number of TB patients in China ranked third in the world (World Health Organization 2018). The effect of TB on CD4+T cell count and the drug resistance of Mycobacterium tuberculosis (MTB) among Chinese HIV-infected patients deserve attention. Additionally, pathogens causing bacterial pneumonia and/or candida infection between HIV-infected and non-HIV-infected patients in China are unknown, but such information could help clinicians diagnose and initiate the proper treatment more rapidly.
AIDS has converted from a death sentence to a chronic, manageable disease in the current ART era, and causes of death in HIV-infected patients have become more diverse. However, causes of death (Antiretroviral Therapy Cohort Collaboration 2010; Weber et al. 2013) and risk factors (Monge et al. 2011; Collaboration of Observational HIV Epidemiological Research Europe in EuroCoord 2012) among Chinese HIV-infected patients associated with ART are limited. By the end of 2016, there were 664,751 reported cases of people living with HIV/AIDS across China (NCAIDS et al. 2017), with 92,976 people in Sichuan province alone (The data came from the Sichuan Center for Disease Control and Prevention) (Fig. 1). Since the first case of AIDS in Sichuan was reported in 1992 (Fu et al. 1992), the number of new HIV-infected patients in Sichuan has increased every year. It is important to promote awareness and management of OIs.
The aim of this study is to provide a clear picture of OIs among HIV-infected patients in Sichuan with the largest number of HIV/AIDS patients across China. In addition, we evaluated causes of death in HIV-infected patients following the introduction of ART, at the Public Health Clinical Center of Chengdu which is the largest center for HIV/AIDS diagnosis and treatment in Sichuan. The information presented would help increase the awareness for HIV/AIDS and plan good management strategies, especially in resource limited regions.

China geographic distribution of people living with HIV/AIDS in 2014.
The data came from the China Global China Global AIDS Response Progress Report, 2015. (National Health and Family Planning Commission 2015).
Different colours indicate the number of people living with HIV/AIDS, and Sichuan Province is marked by the bold line.
This retrospective study was carried out at the Public Health Clinical Center of Chengdu. During January 2014 to December 2015, we observed 2,298 cases of HIV/AIDS in this hospital, and excluded some HIV/AIDS patients from the study. The criteria for exclusion included any one of the following: age < 16 years, without OIs, lacking CD4+T cell counts and HIV viral load data, pregnancy or individuals with other congenital immunodeficiency disease. A total of 954 patients (41.51%) matched our inclusion criteria. ART was initiated according to the national guideline (Tenofovir + lamivudine + efavirenz) (AIDS Professional Group et al. 2015), and the efficacy of ART was evaluated (Kaplan et al. 2009). The 954 HIV-infected patients were divided into two groups: patients with existing OIs at the initiation of ART (ART (−) patients) (n = 125) and patients whose OIs occurred during ART (ART (+) patients) (n = 829). In addition, we included a follow-up of HIV-infected patients without OIs matched with the HIV-infected patients by sex and age as control group (n = 200) (Fig. 2). We reviewed a series of non-HIV-infected patients who were admitted to this hospital from January 2014 to December 2015, and analyzed 2,388 respiratory tract specimens to collect the results of bacteria and candida cultures, records of CD4+T cell counts in 1,289 randomly selected patients with TB infection and 6,795 drug-resistant MTB isolated from non-HIV-infected patients in the laboratory.

Flow diagram of the study.
This work was approved by Public Health Clinical Center of Chengdu. The enrollment of ART, diagnosis of OIs and treatment strategies against OIs were taken in accordance with the guideline recommended by the United States Center for Disease Control and Prevention (Kaplan et al. 2009). The admitted patients completed a face-to-face, paper-and-pencil questionnaire eliciting data on demographics, and clinical information was collected from the laboratory. Laboratory tests were performed to detect the following: Toxoplasmosis, CMV and hepatitis C, bacterial pneumonia, TB, nontuberculous mycobacteria disease, candida infection, Penicillium marneffei infection (PM), PCP, and cryptococcus infection (AIDS Professional Group et al. 2015). The CD4+T cell count was calculated using flow cytometer, and HIV viral load was detected by PCR. We used the VITEK®2 (Automated instrument for microbial identification and antibiotic susceptibility testing) to detect drug resistance of the bacteria, and MGIT 960 (Automated mycobacterial detection system) for the growth, detection and susceptibility testing of MTB. We had differentiated immune reconstitution inflammatory syndrome (IRIS) from primary or new OIs (French et al. 2004), and monitored IRIS during the treatment (Kaplan et al. 2009). Additionally, we classified 252 records of HIV infected patients who were admitted to the hospital during 2015, into the categories specified in the Cause of Death (CoDe) project protocol associated with ART.
Statistical analysisData was analyzed using SPSS 19.0. Demographic characteristics were expressed in percentages. The CD4+T cell count and HIV viral load were presented as medians with standard deviation, and differences in means were compared by t test and Fisher’s test. χ2 test was applied not only in the incidence of OIs in different CD4+T cell count groups, but also in the prevalence of OIs and causes of death between different groups. We used the Logistic regression model to identify independent factors associated with death and OIs in HIV-infected patients. Predictors for mortality were assessed by univariate and multivariate Cox proportional hazards regression. P values of < 0.05 was considered statistically significant.
Data included morbidity rate of HIV infection per year in Sichuan from 2009 to 2015, was collected from the Health and Family Planning Commission of Sichuan Province (Health and Family Planning Commission of Sichuan Province 2016) (Fig. 3).

Trends of HIV/AIDS in Sichuan from 2009 to 2015.
The morbidity rate of HIV (Grey bar) and/or AIDS (Black bar) in Sichuan from 2009 to 2015 are presented, and the morbidity rate refers to the incidence of HIV/AIDS per 100 thousand population in Sichuan every year.
Of the 954 patients, 90.4% were male, 66% married, and the average age was 34 years. Heterosexuality was the major mode of transmission (52.3%), followed by homosexuality (10.2%), injectable drug use (5.1%), bisexuality (2.8%), and blood products (0.3%). About 58% of patients had been to senior high school or more. There are fifty-five minority ethnic groups in China, and minority nationality (Chinese except for the Han nationality) occupies 6.1% of the population in Sichuan (National Bureau of Statistic of the People’s Republic of China 2010). About 17% of the 954 patients were the minority nationality, which is higher than the percentage of minority population in Sichuan (Table 1). There were significant differences in median CD4+T cell count and HIV viral load on admission between ART (+) patients, ART (−) patients and HIV-infected patients without OIs (Table 2).

Characteristics of HIV-infected patients.
aMen, 196; women, 14.
bMen, 159; women, 17.
cMen, 201; women, 28.
dMen, 306; women, 33.

Laboratory results of HIV-infected patients.
*The logarithm of HIV viral load.
CD4+T cell count (cells/µL) and Log VL are expressed as mean ± standard deviation.
Bacterial pneumonia was the most common OIs in 954 clinical records examined, with a prevalence rate of 25.8%. This was followed by candida infection (18.3%), PCP (11.9%), TB (11.5%), infectious diarrhea (9.3%), cryptococcus infection (7.3%), CMV (4.9%), toxoplasmosis (4.6%), hepatitis C (4.0%), nontuberculous mycobacteria disease (2.2%), and PM (0.3%) (Table 3). The occurrence rate of IRIS among 954 patients was 13.2%.
There were 259 cases of OIs observed in 125 ART (−) patients, and 1,344 cases of OIs in 829 ART (+) patients (Table 3). The prevalence of TB, PCP, CMV and hepatitis C were significantly lower in ART (+) patients than ART (−) patients, but the prevalence of bacterial pneumonia, infectious diarrhea and PM were higher in ART (+) patients compared with ART (−) patients. There was no significant difference in the prevalence of other OIs such as candida infection, cryptococcus infection, toxoplasmosis or nontuberculous mycobacteria disease between ART (+) and ART (−) patients (Table 3).
Factors independently associated with OIs in patients included: sex (P = 0.526), age (P = 0.080), education (P = 0.074), marital status (P = 0.0541), CD4+T cell count (P < 0.001) and HIV viral load (P = 0.073). A low CD4+T cell count was found to be a risk factor for OIs. The association of OIs with CD4+T cell count is shown in Table 4. With CD4+T cell count decreasing, the incidence of OIs and the prevalence of bacterial pneumonia, candida infection, PCP, cryptococcus infection, toxoplasmosis, CMV and nontuberculous mycobacteria disease increased significantly.

The prevalence of OIs associated with ART in HIV-infected patients.

The prevalence of OIs related to CD4+T cell count in HIV-infected patients.
The incidence cases of specific OIs are divided into three groups based on CD4+T cell count of 954 HIV-infected patients.
A total of 1,104 respiratory tract specimens were collected from 954 HIV-infected patients. The diagnosis showed that 413 of 954 HIV-infected patients were with bacterial pneumonia. The isolation rate of bacteria in respiratory tract specimens from HIV-infected patients was 10.1% (112/1,104), and from non-HIV-infected patients was 7.8% (186/2,388).
The isolation rates of Pseudomonas aeruginosa, Acinetobacter baumannii and Stenotrophomonas maltophilia were higher in HIV-infected patients than non-HIV-infected patients (Fig. 4A). There was no significant difference in the isolation rate of other bacteria such as Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, coagulase negative staphylococcus, Streptococcus pneumoniae or A. xylosoxidanssubsp.xylosoxidans between HIV-infected and non-HIV-infected patients (Fig. 4A).
There were 112 strains of bacteria in 1,104 respiratory tract specimens from 954 HIV-infected patients, and 186 strains of bacteria in 2,388 respiratory tract specimens from non-HIV-infected patients (Table 5). The rate of drug-resistant bacteria in respiratory tract from HIV-infected patients was 70.0% (75/112), and from non-HIV-infected patients was 53.8% (100/186). The difference between HIV-infected and non-HIV-infected patients was significant, and drug-resistant bacteria contained Methicillin-resistant Stphylococcus aureus, Methicillin-resistant coagulase negative staphylococcus aureus, Vancomycin-resistant enterococci and strains producing extended-spectrum beta-lactamases (Table 5).
To identify the effect of TB on CD4+T cell counts, patients were divided into three groups: the TB/HIV group included 184 HIV-infected patients with TB (median CD4+T cell count 127 ± 83 cells/μL), the HIV group included 770 HIV-infected patients without TB (median CD4+T cell count 140 ± 95 cells/μL), and the TB group included 1,289 TB patients without HIV infection (median CD4+T cell count 384 ± 286 cells/μL). The difference in CD4+T cell counts between the TB/HIV and TB groups and the HIV and TB groups were both significant. CD4+T cell counts were lower in the TB/HIV group compared with the HIV group, although the difference was not significant (Table 6).
The record showed that 6,795 drug-resistant MTB were isolated from the TB patients without HIV infection admitted in our hospital, and we isolated 155 drug-resistant MTB from 184 HIV-infected patients with TB (Table 6). The susceptibility testing toward 15 clinical medicines indicated that the drug resistance of MTB to Ofloxacin, Levofloxacin, Amikacin, Capreomycin, Moxifloxacin, Ciprofloxacin, Linezolid and Gatifloxacin had a higher rate in the TB/HIV group, and the difference towards Streptomycin, Isoniazid, Rifampin, Ethambutol, Isoniazid Aminosalicylate Tablets, Clarithromycin and Rifabutin were not significant between the TB/HIV and TB groups. Multidrug-resistant tuberculosis is a form of TB infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications, Isoniazid and Rifampin. Some forms of TB are also resistant to second-line medications like Ofloxacin, and are called extensively drug-resistant tuberculosis (CDC https://www.cdc.gov/tb/publications/factsheets/drtb/xdrtb.htm). Any drug-resistant MTB is found to be resistant to any anti-TB medication. The rates of any drug-resistant MTB, multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis were higher in the TB/HIV group than TB group (Table 6).
A total of 294 HIV-infected patients (248 ART (+) patients, 46 ART (−) patients) had candida infection in this study. Out of 1,283 throat swabs from HIV-infected patients, 560 samples were positive (43.6%). Records revealed that 503 samples from 2,388 non-HIV-infected patients’ throat swabs were positive (21.1%). The prevalence of candida infection was higher in HIV-infected patients than non-HIV-infected patients. The isolation rate of Candida glabrata was higher than Candida tropicalis in HIV-infected patients, while the isolation rate of Candida glabrata was less than Candida tropicalis in non-HIV-infected patients (Fig. 4). In addition, dual or triple co-infections were more prevalent in HIV-infected patients (21 cases) compared with non-HIV-infected patients (4 cases). The most common co-infection was Candida albicans with Candida glabrata.

Distribution of the pathogens between HIV-infected and non-HIV-infected patients.
(A) The specific pathogens causing bacterial pneumonia were identified in HIV-infected and non-HIV-infected patients. Black bar, the specific pathogens in HIV-infected patients (n = 112); Grey bar, the specific pathogens in non-HIV-infected patients (n = 186). (B) The specific pathogens causing candida infection were identified in HIV-infected and non-HIV-infected patients. Black bar, the specific pathogens in HIV-infected patients (n = 581); Grey bar, the specific pathogens in non-HIV-infected patients (n = 508).

Drug-resistant bacteria of respiratory tract isolates.
A total of 1,104 respiratory tract specimens were obtained from 954 HIV-infected patients, and the record of 2,388 respiratory tract specimens in non-HIV-infected patients was collected from the laboratory in our hospital.
aMethicillin-resistant Stphylococcus aureus.
bMethicillin-resistant coagulase negative staphylococcus aureus.
cVancomycin-resistant enterococci.
dExtended Spectrum Beta-Lactamases.

The drug resistance and CD4+T cell count associated with TB in HIV-infected patients.
There are 6,795 drug-resistant MTB from the TB patients without HIV infection (collected from the laboratory) and 155 drug-resistant MTB from 184 HIV-infected patients with TB. All drug-resistant MTB are tested susceptibility toward 15 clinical medicines, and the result of drug resistance is any drug-resistant MTB, multidrug-resistant tuberculosis or extensively drug-resistant tuberculosis. Moreover, the CD4+T cell count was calculated in the TB group (TB patients without HIV infection), the TB/HIV group (HIV-infected patients with TB), and the HIV group (HIV-infected patients without TB).
CD4+T cell count is expressed as mean ± SD.
There were 74 deaths in 252 records of HIV-infected patients admitted to the hospital during 2015. Of the 74 deaths, 59 patients had not received ART. A total of 122 cases of OIs occurred in 59 ART (−) patients (206.8%), compared with 15 ART (+) patients with 19 cases of OIs (126.7%).
All causes of the 74 deaths are summarized in Table 7. Major causes of death were AIDS-related infections (75.7%) of which bacterial pneumonia, CMV and PCP were the common OIs and AIDS-related malignancies (6.8%) like non-Hodgkin lymphoma and Kaposi sarcoma. Liver disease (6.8%) and renal failure (5.4%) were the leading causes of non-AIDS related death. Other causes of non-AIDS related death were malignancies (1.4%) and cardiovascular disease (1.4%). All injury related deaths were suicide (2.7%).
The incidence of AIDS-related death was significantly higher in ART (−) patients than ART (+) patients (P = 0.003). Death caused by liver disease was more common in ART (+) patients than ART (−) patients (P = 0.022). Other causes of death between the two groups were not significantly different.
COX regression results of univariate analysis showed that CD4+T cell count ≤ 100 cells/μL, ART (−) and PM were independently associated with the death of HIV-infected patients. These factors were further analyzed using multivariate analysis. The risk factors are CD4+T cell count ≤ 100 cells/μL and ART (−) (Table 8), and ART (−) made a bigger difference in survival rates than CD4+T cell count ≤ 100 cells/μL (Fig. 5).

Causes of death in HIV-infected patients during 2015.
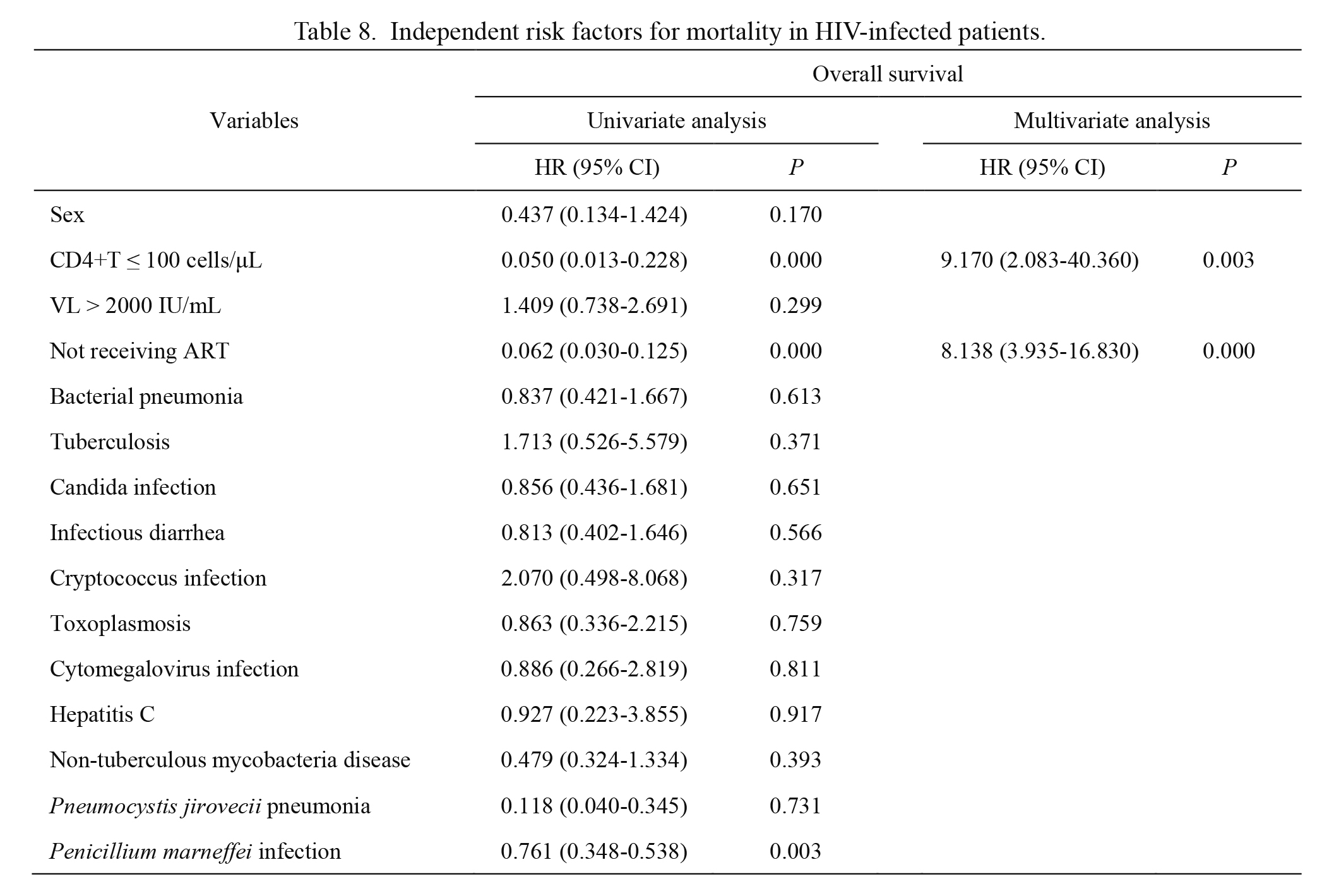
Independent risk factors for mortality in HIV-infected patients.

Survival analysis of HIV-infected patients.
(A) Kaplan-Meier analysis indicated the survival rates of HIV-patients associated with CD4+T cell count. Blue line, survival rate of the CD4+T cell count of ≤ 100 cells/μL group (n = 140); Green line, survival rate of the CD4+T cell count of > 100 cells/μL group (n = 112). (B) Kaplan-Meier analysis indicated the survival rates of HIV-patients associated with ART. Blue line, survival rate of the not receiving ART group (n = 67); Green line, survival rate of the receiving ART group (n = 185).
OIs are the most significant complication of HIV infection, and public health efforts to understand OIs should be valued. However, a picture of OIs in China is still unknown due to lack of surveillance data. Some data on OIs are available in Beijing and Shanghai (Xiao et al. 2013; Luo et al. 2016), but the prevalence of OIs in these regions could not apply to Sichuan in West China. Sichuan is the most hard-hit area with limited resources. Understanding the spectrum of OIs in Sichuan could help us develop successful and efficient public health strategies. Therefore, we conducted a retrospective review with the objective of describing the spectrum of OIs in HIV-infected patients at the Public Health Clinical Center of Chengdu. The findings presented would assist clinicians to make a diagnosis and empirical treatment sooner and help generating a more successful HIV management strategy. These types of OIs reported in this study were consistent with a retrospective study from 2002 to 2011 which was also conducted by our hospital, but the prevalence of OIs was lower than that study (He et al. 2014). Drug-resistant HIV in Sichuan was in a low level, and first-line drugs of ART perhaps was effective (Liu et al. 2014). Our study proved that the wide use of ART had gradually restored the immune systems of HIV-infected patients in Sichuan.
In this study, bacterial pneumonia was the most prevalent OIs in HIV-infected patients, followed by candida infection, PCP and TB. Bacterial pneumonia was rarely reported separately before. One reason might be the difficulty of culture, isolation and identification of pathogens in respiratory tract. We isolated the pathogens and compared them with those isolated from non-HIV-infected patients, and found that isolation rates of P. aeruginosa, A. baumannii and Stenotrophomonas maltophilia were significantly higher in HIV-infected patients than non-HIV-infected patients (Fig. 4A). This information may aid in the clinical diagnosis and treatment of HIV-infected patients.
Previous studies have shown that candida infection, PCP, TB and CMV were the common OIs among HIV-infected patients in China. The prevalence rates of candida infection, PCP and TB among HIV-infected patients (954 patients) were 18.3%, 11.9% and 11.5% respectively in this study. Compared to the prevalence rates of candida infection (29.3%), PCP (22.4%) and TB (32.5%) in Beijing (Xiao et al. 2013), lower prevalence rates of these infections were observed in Sichuan. Additionally, the prevalence rate of CMV (4.9%) was lower in our study than Shanghai (Luo et al. 2016). With such a large number of HIV-infected patients, a lower prevalence of OIs in Sichuan which is a province with limited medical resources was unanticipated. The identification of immune correlates of HIV control is essential for clinical treatment evaluation. Although the low CD4+T cell count in ART (+) patients which could be caused by OIs or ART failure were observed, and we found that the CD4+T cell count was higher in ART (+) patients than ART (−) patients. ART was proved to be active and well-accepted in Sichuan, suggesting that further expanding the HIV screening test and improving the treatment coverage across China are necessary.
ART as the most effective treatment for HIV infection has been widely applied (Zhang et al. 2011). However, there is little research about the relationship between ART and OIs in China. We measured the prevalence of OIs among HIV-infected patients, combined with the influence of ART. The prevalence of TB, PCP, CMV, and hepatitis C were significantly lower in ART (+) patients than ART (−) patients, demonstrating that ART reduced the incidence of some OIs. Although the incidence of OIs was lower in ART (+) patients than ART (−) patients, the prevalence of pneumonia, infectious diarrhea and PM were higher in ART (+) patients compared with ART (−) patients. The unique finding in China revealed that OIs should be monitored regardless of whether the patients are receiving ART or not.
As expected, the incidence of OIs went up with CD4+T cell count decreasing. A noteworthy observation is that the degree of low CD4+T cell counts varies depending on types of OIs. One reason is that effects of different pathogens on CD4+T cell count are different. CD4+T cell count and the ratio of CD4+T to CD8+T declined significantly after hepatitis C, PCP, TB and other bacterial infections (Durante-Mangoni et al. 2013; Kolls 2013; Napoli et al. 2013). In contrast, they changed little after CMV (Hanley et al. 2009). Another reason might be the different baseline levels of CD4+T cell count or different stages of infection in HIV-infected patients. The observation could help clinicians to use CD4+T cell count as a helpful tool for the diagnosis and detection of OIs in areas with limited resources.
Importantly, the rate of drug-resistance bacteria in HIV-infected patients was significantly higher than non-HIV-infected patients, which confirmed the antibiotic resistance in Sichuan (Table 5).
The strategy for treatment of HIV/TB is initiated using empiric treatment (Kaplan et al. 2009) before MTB diagnostic work-up completed which usually takes 7-8 weeks, and genetic methods for detecting MTB may be beneficial to early initiation of accurate treatment in HIV/TB patients. The existing data have shown that CD4+T cell counts are associated negatively with viral load (Papasavvas et al. 2015), and CD4+T cell counts are responsible for the development of most OIs among HIV-infected individuals (Okome-Nkoumou et al. 2014). In this study, CD4+T cell counts in the HIV group were lower than those in the TB group, but the difference between the TB/HIV and HIV groups was not significant. HIV infection increased the chance of TB infection, and TB further destroyed the immune system (Fenner et al. 2013). Our observation was unexpected. The CD4+T cell counts in HIV/TB patients associated with ART worth further investigation. The rates of any drug-resistant MTB and multidrug-resistant tuberculosis isolated from TB group were found to be lower than in Heilongjiang Province (Li et al. 2016). Of note, MTB had various resistance rates to different medicines between HIV-infected and non-HIV-infected patients. Except the drug resistance to first-line medicines (Isoniazid and Rifampin), MTB was observed to have high resistance rates to second-line medications like Ofloxacin. These findings could guide the clinical medication.
The prevalence of candida infection in HIV-infected patients was higher than non-HIV-infected patients. The spectrum of candida in HIV-infected patients is helpful for clinical identification of pathogens.
OIs, non-AIDS related infections and hepatitis were the three leading causes of death among Chinese HIV-infected patients (Feng et al. 2013). In our study, AIDS-related OIs and AIDS-related malignancies were the leading causes of death in HIV-infected patients in Sichuan, and bacterial pneumonia was the most common causes of death. The overall in-hospital mortality rate of HIV-infected patients was 29.36 per 100 person-years. ART (−) patients accounted for a higher proportion (79.7%) of the total deaths. There are a relation between decreased mortality and ART use.
Notably, liver disease death was found to be less in ART (−) patients than ART (+) patients. Antiretrovirals-induced hepatotoxicity is a risk of death from liver disease in HIV-infected patients (Núñez 2006), reminding that we should attach more importance to liver toxicity during ART among HIV-infected patients.
In addition, a point worth noting is that all the injury related deaths were suicides, indicating that the psychological factors of HIV-infection should be noticed (Guimarães et al. 2014). Understanding causes of death in HIV-infected patients could provide information about the severity of HIV infection, and lead to improvement of the clinical management of people living with HIV/AIDS.
CD4+T cell counts of ≤ 100 cells/μL and not receiving ART are risk factors for in-hospital death among HIV-infected patients in Sichuan. Therefore, carrying out ART and improving CD4+T cell counts can effectively reduce the mortality of HIV-infected patients. To further decrease mortality, patients with HIV found eligible for treatment should be treated as soon as possible, before having severe OIs. Therefore, expanding the HIV screening test is required in China.
There were some limitations of the study. We looked into the clinical records of the disease in a hospital, and the prevalence rate could not be deducted just from a hospital, not from a general population.
This study was completed with the support of Public Health Clinical Center of Chengdu.
The authors declare no conflict of interest.