2018 Volume 245 Issue 3 Pages 159-165
2018 Volume 245 Issue 3 Pages 159-165
Primary gastrointestinal lymphoma (PGIL) has been reported in many studies of lymphomas of the gastrointestinal tract worldwide. However, there have been few accurate population-based reports on lymphomas, and it is difficult to apply the strict definition of PGIL to all lymphomas occurring in the gastrointestinal tract. Accordingly, instead of using PGIL, this study included newly diagnosed lymphomas with biopsy or excision specimens obtained from the gastrointestinal tract (GI-related lymphomas) and aimed at presenting the incidence rate, subtype frequency, and occurrence site of GI-related lymphomas. Additionally, we examined GI-related lymphomas diagnosed using flow cytometry (FCM) analysis, cytogenetics analysis, and molecular analysis (multimetric and/or integrated analysis). We extracted data on GI-related lymphomas from 2,098 lymphoma cases registered from the entire Miyagi Prefecture in Japan. The number of GI-related lymphomas was 350, and the incidence rate was 2.97 per 100,000 persons. Diffuse large B-cell lymphoma was the most common subtype (47.4%), followed by extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (32.6%) and follicular lymphoma (8.3%). The stomach was the most common site (62.6%), followed by the large intestine (15.4%), small intestine (14.3%), and duodenum (6.0%). Of the 350 included cases, 111 were diagnosed using multimetric and/or integrated analysis, in which the proportions of positive results for FCM analysis, cytogenetics analysis, and molecular analysis were 81%, 33%, and 51%, respectively. These results may provide a representation of lymphomas occurring in the gastrointestinal tract in Japan. Multimetric and/or integrated analysis of GI-related lymphomas could enable us to acquire useful information for the diagnosis.
Many studies on lymphomas of the gastrointestinal tract have reported on primary gastrointestinal lymphoma (PGIL) (Lewin et al. 1978; Herrmann et al. 1980; d’Amore et al. 1994; Koch et al. 2001; Nakamura et al. 2003; Burke 2011; Ghimire et al. 2011; Terada 2012; Howell et al. 2012; Nakamura and Matsumoto 2013; Peng et al. 2015). PGIL is the most frequent type of extranodal malignant lymphoma, accounting for 30-40% of all extranodal lymphomas, and for about 5-20% of all non-Hodgkin lymphomas (NHLs) (Nakamura et al. 2003; Swerdlow et al. 2008). PGIL is found in whole areas of the intestinal tract, although the stomach is the most frequently involved site, accounting for 60-70% of PGIL cases, followed by the small and large intestines (Herrmann et al. 1980; Burke 2011).
Many epidemiological studies on lymphoid leukemia and/or lymphoma (LL/L) have been conducted in Japan and other countries; however, most of the data were collected from one or more selected representative institutions (mainly in large cities), and most of the studies were led by either clinicians/hematologists or pathologists. Therefore, previous results have had considerable bias (Lymphoma Study Group of Japanese Pathologists 2000; Morton et al. 2006; Sant et al. 2010; Yoon et al. 2010; Yang et al. 2011; van Leeuwen et al. 2014). The epidemiology of lymphomas occurring in the gastrointestinal tract is comparable to that of all LL/L cases; however, there has been no accurate population-based report.
Katsushima et al. (2017) registered all newly diagnosed LL/L cases in Miyagi Prefecture from 2006 to 2010 and determined an accurate incidence rate and more realistic frequencies of LL/L subtypes for the first time in Japan. Furthermore, in Miyagi Prefecture, most lymphoma cases from the 22 main hospitals are forwarded to the READ (registration-examination-analyses-description) system® (Life Science Institute, Co. Ltd., Tokyo, Japan). According to this system, the cases were diagnosed by expert hematopathologists using flow cytometry (FCM) analysis, cytogenetics analysis, and molecular analysis (multimetric and/or integrated analysis), as well as morphological examination, which consisted of the observation of hematoxylin and eosin (HE)-stained slides and immunohistochemistry (IHC) (Harigae et al. 2002; Yokoyama et al. 2012). Because some of the extracted cases in our study were diagnosed using the READ system®, we also assessed the usefulness of multimetric and/or integrated analyses such as FCM analysis, cytogenetics analysis, and molecular analysis. Similar assessments have not yet been reported.
It is difficult to apply the strict definition of PGIL to all cases because we cannot completely distinguish whether the lymphoma originated in the gastrointestinal tract as a primary lesion or whether it extended to the gastrointestinal tract from the surrounding lymph nodes. Thus, instead of PGIL, this study included lymphomas newly diagnosed with biopsy or excisional specimens obtained from the gastrointestinal tract (GI-related lymphomas) and aimed at determining the incidence rate, subtype frequencies, and occurrence site of GI-related lymphomas. Additionally, we examined GI-related lymphomas diagnosed using multimetric and/or integrated analysis and considered the usefulness of multimetric and/or integrated analysis for routine diagnosis.
Of the 2,098 newly diagnosed cases of LL/L in Miyagi Prefecture from 2006 to 2010, we extracted data of 350 cases of GI-related lymphomas. These GI-related lymphomas cases were diagnosed using morphological examination (HE and IHC) together with multimetric and/or integrated analysis such as FCM analysis, cytogenetics analysis using G-banding and/or fluorescence in situ hybridization (FISH), and molecular analysis using the Southern blot analysis of immunoglobulin heavy chain (IgH)/T-cell receptor (TCR) β genes with or without polymerase chain reaction. The incidence rate was calculated by counting the number of cases (incidence) in the average population of Miyagi Prefecture, which is approximately 2.354 million in total.
In FCM analysis, cases in which abnormal cell populations (ACPs) were detected or not detected were judged to be ACP positive and negative, respectively. In cytogenetics analysis, cases in which clonal abnormalities, such as MALT1, BCL2, BCL6, CCND1, and/or MYC, were identified were regarded as clonal abnormalities positive, and where these were not identified, they were regarded as negative. In molecular analysis, cases in which rearrangement of IgH and/or TCR β genes were detected using the Southern blot analysis with or without polymerase chain reaction were defined as rearrangement positive, and if not identified, were defined as negative. Subtype classifications were carried out in accordance with the 2008 World Health Organization (WHO) classifications (Swerdlow et al. 2008).
The biopsy or excision specimens were fixed in 10% neutral buffered formalin and embedded in paraffin. Next, 4-μm-thick sections were cut and stained with HE for histological evaluation. Immunohistochemical staining was performed using formalin-fixed, paraffin-embedded tissue sections with antibodies such as CD3, CD10, CD20, CD56, CD79a, cyclin D1, BCL2, and Ki67. FCM analysis was performed using a flow cytometer according to conventional methods.
Cytogenetics analysis was performed as follows: cells from excisional or biopsy specimens were analyzed using standard G-banding with trypsin-Giemsa staining. Karyotypes were interpreted using the International System for Cytogenetic Nomenclature criteria. FISH analysis was performed using paraffin-embedded sections and/or pieces of excisional or biopsy specimens after the application of Carnoy’s fixative for detecting chromosomal translocations that involve 18q21/MALT1, 18q21/BCL2, 3q27/BCL6, 11q13/CCND1, and/or 8q24/MYC. Molecular analysis was performed as follows: Southern blotting-based IgH and TCR β gene rearrangement analysis with or without polymerase chain reaction were performed using extracted DNA from biopsy or excisional specimens. A monoclonal pattern of IgH and/or TCR β rearrangements were detected in the same specimens.
Our study was approved by the ethics committee or the applicable organization of each hospital and institution (Ethics Committee of Tohoku University Graduate School of Medicine No. 2009-28 and 2014-1-573), and the conduct of the study complied with the Declaration of Helsinki.
Of the 2,098 cases registered in the 5-year period, the number of GI-related lymphomas (incidence) was 350 (160 men and 190 women), and the incidence rate was 2.97 per 100,000 persons. The proportion of GI-related lymphomas among all the lymphomas was 16.7%. Of the 350 cases, 324 cases (92.6%) were of B-cell lineage and 26 cases (7.4%) were T/natural killer-cell lineage. Diffuse large B-cell lymphoma (DLBCL) was the most common subtype (166 cases, 47.4%), followed by extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT) (114 cases, 32.6%), follicular lymphoma (FL) (29 cases, 8.3%), enteropathy-associated T-cell lymphoma, type II (9 cases, 2.6%), peripheral T-cell lymphoma (PTCL), not-otherwise specified (9 cases, 2.6%), and mantle cell lymphoma (MCL) (6 cases, 1.7%). The details of the subtype frequencies are shown in Table 1.
Concerning the site of the gastrointestinal tract where the biopsies or excisions were performed (occurrence site distribution), the stomach was the most common site (219 cases), followed by the large intestine (54 cases of which 7 were in the cecum, 33 in the colon, and 14 in the rectum), the small intestine (50 cases) excluding the duodenum (21 cases), esophagus (1 case), appendix (1 case), and multiple sites (4 cases). The details of the occurrence site distribution of all the subtypes are shown in Table 2.
Of the above mentioned 350 cases, 111 were reported in the READ system® and diagnosed using the multimetric and/or integrated analysis. In FCM analysis (Fig. 1), 70 cases were positive, and 20 cases were borderline because ACPs were seen in a very small number of cells but could not be confirmed. On the other hand, 18 cases were negative, and 1 case was not analyzed because of shortage of specimens (Insufficiency). In addition, 2 cases were not analyzed, because examinations were not requested from the clinical side. Thus, among the 109 cases, the proportion of ACP-positive cases and borderline cases was 81% (90 of 109 cases). The relationship between the proportion and the major subtypes is also shown in Fig. 1.
In cytogenetic analysis (Fig. 2), 33 cases were positive and 3 cases were borderline, while 43 cases were negative, and 30 cases were not analyzed because of shortage of specimens. In 2 cases, examinations were not requested for from the clinical side. Thus, the total number of positive and borderline cases was 36, and the proportion of cases with clonal abnormalities was 33% (36 out of 109 cases). The relationship between the proportion and the major subtypes is also shown in Fig. 2.
In molecular analysis (Fig. 3), 52 cases were positive, 5 cases were negative, 44 cases were not analyzed because of shortage of specimens, and 10 cases were not analyzed because of no request from the clinical side. Thus, the proportion of cases in which rearrangement was observed was 51% (52 out of 101 cases). The relationship between the proportion and the major subtypes is also shown in Fig. 3.

Incidence, incidence rate, and subtype frequencies of GI-related lymphomas.
Incidence rate shows the number of cases per 100,000 persons.
GI-related lymphomas, lymphomas newly diagnosed via biopsy or excision specimen obtained from the gastrointestinal tract; DLBCL, diffuse large B-cell lymphoma; MALT, extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue/marginal zone lymphoma; FL, follicular lymphoma; MCL, mantle cell lymphoma; IVL, intravascular large B-cell lymphoma; BL, Burkitt lymphoma; NOS, not-otherwise specified; EATL, enteropathy-associated T-cell lymphoma, type II; PTCL, peripheral T-cell lymphoma, NOS; ATL, adult T-cell leukemia/lymphoma; ALCL, anaplastic large cell lymphoma; AITL, angioimmunoblastic T-cell lymphoma.

Occurrence site distribution of all subtypes of GI-related lymphomas.
GI-related lymphomas, lymphomas newly diagnosed via biopsy or excision specimen obtained from the gastrointestinal tract; DLBCL, diffuse large B-cell lymphoma; MALT, extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue/marginal zone lymphoma; FL, follicular lymphoma; MCL, mantle cell lymphoma; IVL, intravascular large B-cell lymphoma; BL, Burkitt lymphoma; NOS, not-otherwise specified; EATL, enteropathy-associated T-cell lymphoma, type II; PTCL, peripheral T-cell lymphoma, NOS; ATL, adult T-cell leukemia/lymphoma; ALCL, anaplastic large cell lymphoma; AITL, angioimmunoblastic T-cell lymphoma.
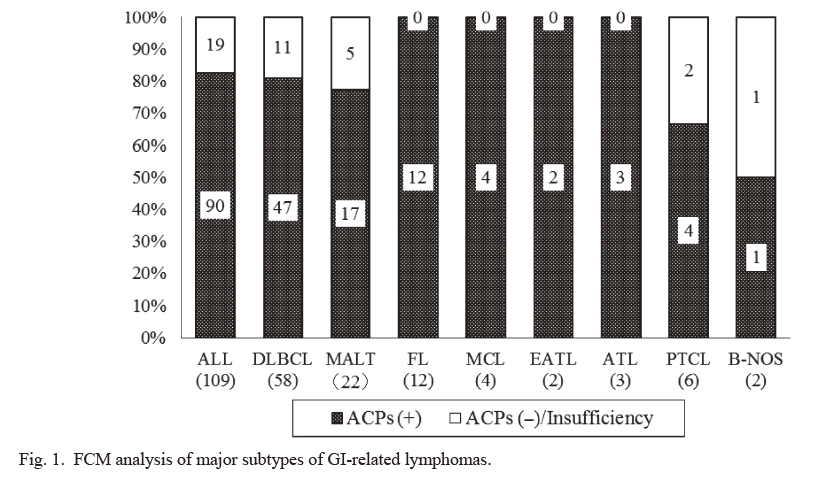
FCM analysis of major subtypes of GI-related lymphomas.
FCM, flow cytometry; GI-related lymphomas, lymphomas newly diagnosed via biopsy or excision specimen obtained from the gastrointestinal tract; DLBCL, diffuse large B-cell lymphoma; MALT, extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue/marginal zone lymphoma; FL, follicular lymphoma; MCL, mantle cell lymphoma; EATL, enteropathy-associated T-cell lymphoma, type II; ATL, adult T-cell leukemia/lymphoma; PTCL, peripheral T-cell lymphoma, not-otherwise specified; B-NOS, B-cell lymphoma, not-otherwise specified; ACPs, abnormal cell populations.
ACPs (+) consisted of cases in which ACPs were detected (positive cases) and cases in which ACPs were seen in very small number of cells but could not be confirmed (borderline cases). Insufficiency included one case which was not analyzed because of shortage of specimen. The proportion of ACPs (+) was 81% (90 out of 109 cases). The results showed ACPs (+) for 81% of DLBCL, 77% of MALT, 100% of FL, MCL, EATL, and ATL, and 67% of PTCL.

Cytogenetic analysis of major subtypes of GI-related lymphomas.
GI-related lymphomas, lymphomas newly diagnosed via biopsy or excision specimen obtained from the gastrointestinal tract; DLBCL, diffuse large B-cell lymphoma; MALT, extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue/marginal zone lymphoma; FL, follicular lymphoma; MCL, mantle cell lymphoma; EATL, enteropathy-associated T-cell lymphoma, type II; ATL, adult T-cell leukemia/lymphoma; PTCL, peripheral T-cell lymphoma, not-otherwise specified; B-NOS, B-cell lymphoma, not-otherwise specified.
Clonal Abnormalities (+) consisted of cases in which clonal abnormalities were detected (positive cases) and cases in which they were seen in few proportions but could not be confirmed (borderline cases). Insufficiency included 30 cases which were not analyzed because of shortage of specimens. The proportion of clonal abnormalities (+) was 33% (36 out of 109 cases). The results showed abnormalities for 19% of DLBCL, 23% of MALT, 83% of FL, and 100% of MCL.

Molecular analysis of major subtypes of GI related lymphomas.
GI-related lymphomas, lymphomas newly diagnosed via biopsy or excision specimen obtained from the gastrointestinal tract; DLBCL, diffuse large B-cell lymphoma; MALT, extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue/marginal zone lymphoma; FL, follicular lymphoma; MCL, mantle cell lymphoma; EATL, enteropathy-associated T-cell lymphoma, type II; ATL, adult T-cell leukemia/lymphoma; PTCL, peripheral T-cell lymphoma, not-otherwise specified; B-NOS, B-cell lymphoma, not-otherwise specified.
Rearrangement (+) consisted of cases in which rearrangement of immunoglobulin heavy chain / T-cell receptor β genes were detected (positive cases). Insufficiency included 44 cases which were not analyzed because of shortage of specimens. The proportion of rearrangement (+) was 51% (52 out of 101 cases). The results showed rearrangement for 51% of DLBCL, 32% of MALT, 66% of FL, and 75% of MCL.
Many studies on lymphomas of the gastrointestinal tract focused on PGIL. Dawson et al. (1961) suggested that PGIL has the following five characteristics: (i) the absence of peripheral lymphadenopathy at the time of disease onset; (ii) no evidence of enlarged mediastinal lymph nodes; (iii) normal total and differential white blood cell counts; (iv) a predominance of bowel lesions at laparotomy with only the lymph nodes obviously affected in the immediate vicinity; and (v) no lymphomatous involvement of the liver and spleen. However, we consider it difficult to apply this strict definition of PGIL to all cases because it is more difficult to completely distinguish whether the lymphoma originated in the gastrointestinal tract as a primary lesion or whether it has advanced to the gastrointestinal tract from the surrounding lymph nodes and other organs. Therefore, we decided to extend the target of our study to GI-related lymphomas, which we often encounter during routine work (diagnosis).
The incidence rate of GI-related lymphomas in our study was 2.97 per 100,000 persons. According to previous reports, the incidence rate of PGIL ranged from 0.58 to 1.73. The most recent report in 2009 showed an incidence rate of 2.10 (Howell et al. 2012). Our study showed a higher rate compared with other studies. We registered and extracted all lymphoma cases from a population base of approximately 2.354 million people (Katsushima et al. 2017), and we did not limit the subject of extraction to PGIL. However, as the proportion of PGIL in NHL or all lymphomas is reported to be 5-20% (Nakamura et al. 2003; Swerdlow et al. 2008), considering our result of 16.7%, the incidence rate seems reasonable.
Regarding subtype frequencies, some reports showed that the proportion of B cell lymphoma accounts for approximately 90% of PGIL and that the combined proportions of MALT and DLBCL account for 80%, despite some differences in the proportions of MALT or DLBCL (Howell et al. 2012; Terada 2012; Nakamura and Matsumoto 2013). Our study also shows quite similar results. Regarding the occurrence site distribution, some reports showed that the stomach is the most common site, accounting for 40-75% of all cases; in contrast, the large intestine is a relatively uncommon site for PGIL (Lewin et al. 1978; Herrmann et al. 1980; d’Amore et al. 1994; Koch et al. 2001; Nakamura et al. 2003; Howell et al. 2012; Terada 2012; Nakamura and Matsumoto 2013). Our study also showed that the stomach is the most common site, while the proportion occurring in the large intestine suggested that our cases might have included those that have advanced to the gastrointestinal tract from the surrounding lymph nodes and other organs. It is well known that the incidence of FL in the small intestine, including the duodenum, is high (Yamamoto et al. 2010; Moy et al. 2016). We observed that 45% of FLs (13/29) in our study were diagnosed using specimens obtained from the duodenum and that 69% of lymphomas diagnosed using specimens obtained from the duodenum (13/21) were FL.
Nakamura and Matsumoto (2013) reported that among 49 cases of T-cell lymphoma belonging to PGIL, 11 cases (22%) were identified at multiple sites. In contrast 17 (3%) out of 595 cases of B-cell lymphoma belonging to PGIL were identified at multiple sites. Even in our study, despite the small number of subjects, our findings suggested that T-cell lymphoma might often be found at multiple sites.
Among the extracted 350 cases, 111 (32%) were diagnosed using HE and IHC, together with multimetric and/or integrated analysis such as FCM analysis, cytogenetic analysis, and molecular analysis. In FCM analysis (Fig. 1), the proportion of cases in which ACP was observed, including the cases that were borderline, was very high at 81% (88 out of 109 cases). As the biopsy specimen obtained from the gastrointestinal tract is generally small, pathologists are often faced with the difficulty of making a diagnosis using only HE and IHC. On the other hand, pathologists can usually confirm and use the result of FCM analysis within one business day after submission of specimen. Considering the results of our study, the use of FCM analysis together with HE and IHC is very useful for diagnosis, and contributes to shortening of the time to diagnosis. In cytogenetics analysis, 36 out of 109 cases (33%) showed clonal abnormalities, including those that were borderline (Fig. 2). Abnormalities were reported in 20-30% of DLBCL, 10-20% of MALT, 60-80% of FL, and almost 100% of MCL (Swerdlow et al. 2008). Although, 30 out of 109 cases could not be analyzed because of shortage of specimens, the results in our study showed abnormalities for 19% of DLBCL, 23% of MALT, 83% of FL, and 100% of MCL, thus showing that cytogenetics analysis using biopsy specimen obtained from the gastrointestinal tract could contribute to the diagnosis. In molecular analysis, 52 out of 101 cases (51%) were positive. Considering that 40 of 101 cases could not be analyzed because of insufficient volume, molecular analysis can also contribute significantly to diagnosis. On the other hand, it may be necessary to establish a close relationship with endoscopists and to ask them to submit sufficient specimen for diagnosis.
The multimetric and/or integrated analysis has the disadvantage that cytogenetics and molecular analyses could not be completed in 30-40% of cases because of shortage of specimen volume; this was inevitable because most specimens were obtained using biopsy and were small in volume. However, our study showed that there were many cases in which more accurate diagnosis could be performed using multimetric and/or integrated analysis. Findings from our study confirmed that the combined use of FCM analysis can be very effective. On the other hand, the rate of use with multimetric and/or integrated analysis has remained low at 32% of the total number of cases of GI-related lymphomas despite having 69% of all LL/Ls diagnosed using multimetric and/or integrated analysis in our previous report (Katsushima et al. 2017). Further utilization of multimetric and/or integrated analysis should be considered.
In summary, we present the exact number of cases (incidence) and incidence rate, subtype frequencies, and occurrence site of GI-related lymphomas. It is expected that our results can provide a representative index of lymphomas occurring in the gastrointestinal tract in Japan. Furthermore, although we showed that multimetric and/or integrated analysis in GI-related lymphomas enabled us to acquire useful information for the diagnosis, efforts to increase the submission of specimen for multimetric and/or integrated analysis are needed.
This work was supported by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS KAKENHI No. 24590677/15K08609) and by the Public Interest Incorporated Foundation of Ichinohasama Memorial READ Blood Academy (Sendai, Japan, No. 2015-002).
The authors declare no conflict of interest.
F.F., H.K., and R.I. designed the study; F.F., H.K., N.F., and R.I. collected and extracted lymphoma cases; N.F. collected the clinical information of the cases as needed; F.F., H.K., S.K-F, Y.N., H.S., and R.I. diagnosed the lymphoma cases pathologically and reviewed the pathological slides; F.F, H.K., N.F., and R.I. reviewed and interpreted multimetric and/or integrated analysis; F.F. and H.K. mainly drafted the manuscript with some help by Y.N. and R.I. All authors approved the final draft submitted. F.F. and H.K. contributed equally to this work.