2018 Volume 245 Issue 3 Pages 179-185
2018 Volume 245 Issue 3 Pages 179-185
Thoracic epidural anesthesia (TEA) and paravertebral block (PVB) have been performed for perioperative regional anesthesia in the trunk. However, TEA and PVB are associated with a risk of serious complications, such as pneumothorax, hypotension, or nerve damage. Retrolaminar paravertebral block (RLB) was introduced as a new alternative to PVB. This new approach might lower the risk of serious complications, but its use has not been well established yet. Therefore, we conducted a double-masked, placebo-controlled, randomized clinical trial to evaluate the efficacy of a double-level RLB for postoperative analgesia after breast cancer surgery. A total of 122 women who underwent breast cancer surgery with axillary lymph node dissection under general anesthesia were allocated into RLB group (60 patients) and Control group (62 patients). RLB was performed upon surgery completion with 15 ml ropivacaine (0.5%) for each lamina of the T2 and T4 vertebrae. In Control group, the same volume of normal saline was injected at each level. The time to first postoperative analgesic administration was significantly longer in RLB group than that in Control group (161.5 min vs. 64.0 min). The pain score in RLB group was significantly lower immediately after surgery. However, the number of patients requiring analgesics during the 12-hour post-surgical period was similar between RLB group (20 patients) and Control group (22 patients). In conclusion, the double-level RLB could delay the time to initial administration of analgesics, but this technique may be insufficient to reduce the analgesic requirement within the 12-hour postoperative period following breast cancer surgery.
Novel approaches to paravertebral blocks (PVB) have been the focus of many studies in recent years (Forero et al. 2016; Murouchi and Yamakage 2016; Costache et al. 2017). These new blocks are considered as compartment blocks or muscle infiltration blocks. In these approaches, the needle-tip is not advanced into the paravertebral space (PVS) beyond the superior costotransverse ligament (SCTL). Although the distribution of local anesthetics is being discussed, local anesthetics are assumed to penetrate the SCTL and reach the PVS, without having to directly inject it into the PVS. With the use of these novel blocks, the risk of serious complications such as pneumothorax, hypotension, and nerve damage can be lower than that associated with classical PVB.
The retrolaminar paravertebral block (RLB) was proposed as an easier and more straightforward alternative to the classical PVB (Pfeiffer et al. 2006). The RLB needle should contact the lamina, upon which the local anesthetic is injected. Continuous RLB has been found to be effective in controlling pain following breast cancer surgery (Juttner et al. 2011; Zeballos et al. 2013; Murouchi and Yamakage 2016). Some studies investigating single injections with the classical PVB have reported that a multi-level injection could provide more extensive spread of the local anesthetic than a single-level injection (Naja et al. 2006; Kaya et al. 2012). However, the efficacy of a single RLB injection for treating acute pain has not been studied.
Thus, we conducted this randomized clinical trial to evaluate the efficacy of a double-level RLB in patients who underwent breast cancer surgery. We have hypothesized that the double level RLB would reduce the analgesic requirement within the 12-hour postoperative period following breast cancer surgery.
This study was a prospective, randomized, double-masked, placebo-controlled study and was reported according to the Consolidated Standards of Reporting Trials (CONSORT) statement. This study was registered with the University Hospital Medical Information Network Clinical Trial Registry (UMIN-CTR: 000019982). Ethical approval for this study (Ethical Committee N° kkrtohoku-201407anes_S1_01) was provided by the Tohoku Kosai Hospital Institutional Review Board, Sendai, Japan (Chairperson Dr. K. Okamura) on the 15th July 2014. Written informed consent was obtained from all patients prior to participation in the study, and all study procedures were conducted at Tohoku Kosai Hospital (Miyagi, Japan). All aspects of the study conduct adhered to the tenets of the Declaration of Helsinki.
PatientsAdult patients scheduled for unilateral breast cancer surgery with axillary lymph node dissection under general anesthesia were enrolled. The surgical procedures in this study included modified radical mastectomy with or without insertion of a tissue expander and breast-conserving surgery. The subjects met all the following inclusion criteria: over 20 years of age, ASA physical status class I or II, New York Heart Association (NYHA) class I, and Hugh-Jones classification I. Subjects were excluded if they met any of the following criteria: renal dysfunction (estimated glomerular filtration rate < 60 ml/min/1.73 m2); active gastrointestinal tract ulcer; body mass index > 35; presence of a skin lesion at the puncture site; history of severe postoperative nausea/vomiting; or allergy to local anesthetics, pentazocine, or non-steroidal anti-inflammatory drugs (NSAIDs).
MethodPatient assignment to the RLB and the control groups (in a 1:1 ratio) was performed using computer-generated randomization. On the morning of surgery, the chief nurse of the operating room entered the patient’s data (name, age, height, weight, and scheduled surgical procedure) into the computer software and confirmed that the allocation group was automatically assigned. She also prepared two syringes filled with 15 ml of the study solution and labeled them with the case number and patient’s name. The RLB group received 15 ml of 0.5% ropivacaine for each lamina of the T2 and T4 vertebrae. The control group received 15 ml of normal saline in the same manner. Double-masking was achieved by concealing the randomization list from all study members and participants until all study procedures and analyses were completed.
Patients were monitored with ECG, pulse oximetry, and a non-invasive blood pressure measuring device. We induced anesthesia with propofol 1-2 mg/kg, continuously infused remifentanil 0.2-0.5 μg/kg/min, and conducted tracheal intubation after administering rocuronium bromide 0.6-1.0 mg/kg. We maintained anesthesia with sevoflurane 1-1.5% and continuously infused remifentanil 0.2-0.5 μg/kg/min. Upon surgery completion, fentanyl 4 μg/kg and droperidol 0.75 mg were administered intravenously. After the drape was removed from the patient, diclofenac 50 mg was administered rectally.
Subsequently, the patient was placed in the lateral decubitus position with the surgically treated side facing up. The spinous processes of the T2 and T4 vertebrae were palpated, and the largest spinous process was defined as C7, and 1 cm lateral to the midline of each spinous process was labelled on the surgical side. After the skin was disinfected with 1.0% chlorhexidine in 83% ethanol, a 22-gauge 70-mm Cathelin needle® (TERUMO, Tokyo, Japan) was inserted at the marked site and advanced at an angle of approximately 90° to the skin until the needle tip contacted the lamina. After confirming negative aspiration, 15 ml of study medication was injected at each of the two marked sites. The patient was returned to the supine position and the administration of sevoflurane and remifentanil was discontinued. After extubation, fentanyl 50-100 μg was administered intravenously if the patient complained of postoperative pain, and if each anesthesiologist determined the need for additional analgesics.
After the patient left the operating room, a nurse in the ward, who was blinded to group allocation, assessed postoperative pain using a 0-10 Numerical Rating Scale (NRS; 0 = no pain and 10 = the worst pain imaginable) for 12 hours following surgery. Data of NRS was recorded at 0 (immediately returning the ward), 0.5, 1, 2, 3, 6, 12 hours postoperatively, as well as at discharge. Analgesics were given when the NRS pain score exceeded 4 points (unless the patients refused) and when the patient requested supplemental analgesia (regardless of NRS score). The first choice of analgesic was pentazocine 15 mg administered intramuscularly, and the second choice was diclofenac 50 mg administered rectally.
EndpointsThe primary endpoint was the number of patients requiring analgesics within the 12-hour postoperative period. Secondary endpoints included the time to first use of analgesics, the number of patients requiring antiemetics, the maximum NRS score within the 12-hour postoperative period, and the NRS score on the date of discharge. Additionally, the change in NRS score during the first three postoperative hours was also evaluated to confirm the pain intensity immediately after surgery.
Sample sizeAt our institution, 185 patients underwent modified radical mastectomy with axillary lymph node dissection or sentinel lymph node biopsy in 2013. The percentage of patients requiring postoperative analgesics within the first 24 hours following surgery was 49.2% (95% confidence interval [CI], 42.3-57.2). We estimated that the ratio of patients that received analgesics was 42.3%, which was the lower limit of the CI, and assumed that a reduction by two-thirds of this ratio would prove clinical efficacy with reference to the report that demonstrated that multilevel PVB for breast cancer surgery reduced the number of patients with postoperative pain by one third (Moller et al. 2007). With the α-error set at 0.05 and the statistical power set at 0.8, the calculated sample size required for a two-sided chi-squared test was 92 patients (46 patients per group). We planned to enroll approximately 150 patients in the current study, with consideration given for drop-out due to complications or loss to follow-up.
Statistical analysisThe number of patients requiring analgesics and antiemetics was analyzed using a chi-squared test. Time-to-event methods (Kaplan-Meier survival curves, the Wilcoxon test, and Cox proportional-hazards models) were used to compare event rates for analgesic use after surgery between the RLB and control groups. The time to first use of analgesics, maximum NRS score, and NRS score at discharge were compared between groups using the Mann-Whitney U test. The change in NRS score during the 3-hour postoperative period was analyzed using a linear mixed-effects model. Demographic data are presented as the mean (standard deviation [SD]) or median (interquartile range) where appropriate.
All statistical analyses, except changes in NRS score over the 3-hour postoperative period, were performed using EZR Version 1.36 (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R Version 2.13.0 (The R Foundation for Statistical Computing, Vienna, Austria) (Kanda 2013). The changes in NRS score over the 3-hour postoperative period were analyzed with JMP® Pro Version 12.2.0 (SAS Institute Inc., Cary, NC, USA). All reported P values are two-sided; statistical significance was defined as P < 0.05.
Between September 2014 and October 2015, 149 patients were enrolled and randomly allocated to one of the two study groups on the morning of surgery. Twelve patients exhibited renal dysfunction after enrollment and were subsequently excluded; thirteen were excluded due to a change in operation or anesthetic method. One patient withdrew consent and one was excluded due to surgery postponement. Thus, a total of 122 patients were included in the final analyses. There were 60 patients in the RLB group and 62 in the control group (Fig. 1). The baseline demographic and clinical characteristics, as well as the operation method, were similar between the two groups (Table 1).
The ratio of patients requiring analgesics within the first 12 hours following surgery in the control and the RLB groups was 35.5% and 33.3%, respectively (Table 2). There was no significant difference between groups (P = 0.85). The Kaplan-Meier survival curve for time to first analgesic administration after surgery is shown in Fig. 2. There was no significant difference in analgesia-free time between the groups (Wilcoxon test, P = 0.297). An assessment of the proportional hazards assumption showed that the hazards ratio was not constant over time (P = 0.001). Therefore, we did not present the results of the Cox proportional hazards regression analysis.
The ratio of patients requiring antiemetics within the 12-hour post-surgical period in the control and the RLB groups was 16.1% and 10.0%, respectively (Table 2). There was no significant difference between the groups (P = 0.42). The maximum NRS pain score and the NRS score at discharge were similar between the control and RLB groups (P = 0.16 and P = 0.36; Table 2). The time to first use of analgesics was significantly longer in the RLB than the control group (161.5 min vs. 64.0 min; P = 0.0008).
The change in NRS pain scores within the 3-hour post-surgical period in each group is shown in Fig. 3. A significant group effect was identified with a positive coefficient (estimate = 0.7399, P < 0.001), indicating that the NRS score was significantly higher in the control group than the RLB group immediately after surgery. Conversely, a significant effect of the postoperative time was identified with a negative coefficient (estimate = –0.0042, P = 0.001), indicating that the NRS score significantly decreased with time. Additionally, a significant interaction between the group and the postoperative time was found with a negative coefficient (estimate = –0.0043, P < 0.001), indicating that the reduction rate of NRS in the control group was larger than the RLB group (Table 3).

CONSORT 2010 flow diagram.

Demographic characteristics of patients undergoing breast cancer surgery.
Data are reported as the number of patients (proportion), mean (standard deviation), or median [interquartile range].
BMI, body mass index; RLB, retrolaminar block.
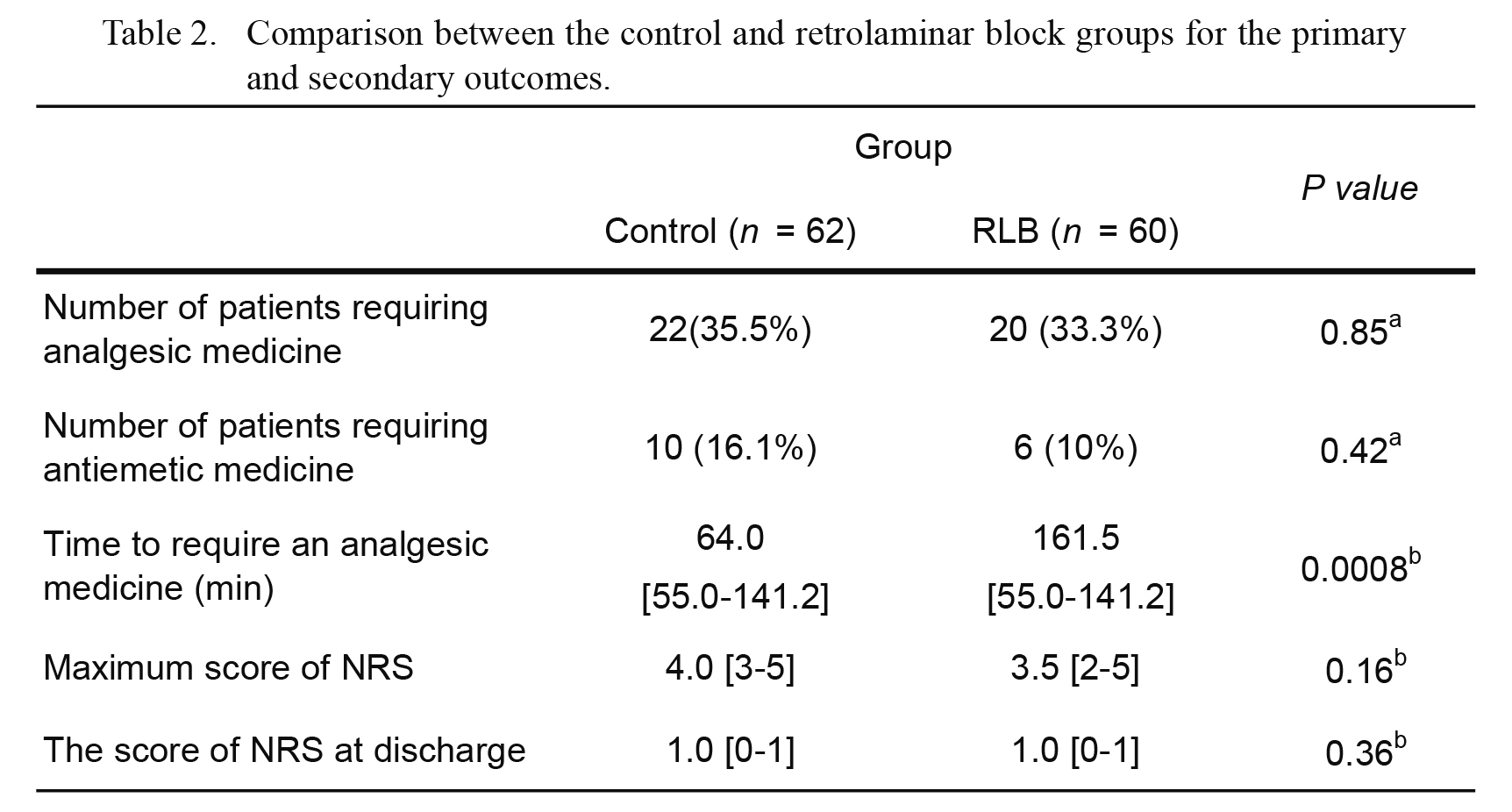
Comparison between the control and retrolaminar block groups for the primary and secondary outcomes.
Data are presented as the number of patients (proportion) or median [interquartile range].
NRS, numerical rating scale (0-10) for pain; RLB, retrolaminar block.
aFisher’s exact test, bMann-Whitney U test.

Kaplan-Meier survival curve for time to first analgesic administration following surgery.
There is no significant difference in the time to first analgesic administration after surgery between the control and retrolaminar block groups (Wilcoxon test, P = 0.297). The continuous and dotted lines indicate the probability of not requiring analgesics in the control and RLB groups, respectively.

The change in the numerical rating scale pain score during the 3-hour post-surgical period.
The numerical rating scale (NRS) pain score in the retrolaminar block (RLB) group is significantly lower than that in the control group within two hours after surgery (P < 0.001). The continuous and dotted lines indicate the NRS scores of the RLB and control groups, respectively. The error bar with each plot indicates the standard error.

Effect of group and postoperative time on the change of NRS score.
CI, confidence interval; NRS, numerical rating scale (0-10) for pain.
In this study, we aimed to evaluate the effect of a double-level RLB for acute postoperative analgesia following breast cancer surgery. We found that the number of patients requiring analgesics within the first 12 hours postoperatively was similar between the RLB and control group. The time to initial postoperative administration of analgesics was significantly longer in the RLB group than the control group. The NRS score in the RLB group remained significantly lower than that in the control group during the acute postoperative phase. However, the duration of the double-level RLB in our study was not long enough for postoperative analgesia after breast cancer surgery, unlike the continuous RLB reported previously.
The RLB was introduced as a new approach to the PVB (Fig. 4A) (Pfeiffer et al. 2006). However, the distribution of local anesthetic injected during RLB has been unclear. Several case reports have shown the efficacy of RLB for breast cancer surgery (Juttner et al. 2011; Zeballos et al. 2013) and rib fracture (Voscopoulos et al. 2013; Yoshida et al. 2015). Local anesthetics injected upon the laminae were assumed to penetrate the PVS. In contrast, Murouchi and Yamakage (2016) reported that the analgesic effect of continuous RLB was weaker than that of continuous classical PVB. A radiographic study reported that 20 ml of initial RLB injection did not spread into the PVS (Satoh 2013). Additionally, although Agarwal et al. (2015) described that single-injection PVB with long-acting local anesthetics like ropivacaine could last for 24 hours, the analgesic duration of the double-level RLB was shorter. Thus, the RLB may have a mechanism of action different from that of the classical PVB.
In breast cancer surgery, the lateral cutaneous and anterior branches arising from the intercostal nerve play an important role in the conduction of postoperative pain signals. The position of the needle tip (Fig. 4B) suggests that RLB is an interfascial plane block, spreading between the laminar and transversospinalis muscles. Recently, Elsharkawy et al. (2018) described, based on anatomy, that a retrolaminar space continued laterally to the interfacial plane between the serratus anterior and external intercostal muscles, in which the lateral cutaneous branch runs. Blockade of the lateral cutaneous branch by RLB might partially provide postoperative analgesia for breast cancer surgery. In the current study, to conceal the block effect from the anesthetist, we could not confirm accurate distribution of the local anesthetic with a sensory check procedure. The extent of cutaneous sensory loss after local anesthetics injected is needed to clarify the mechanism of action of RLB.
Another problem related to RLB is that the optimal local anesthetic dose of RLB is not known. In previous reports, an initial dose of 20-30 ml of local anesthetic was injected, followed by continuous injection or intermittent bolus injections through a catheter (Juttner et al. 2011; Zeballos et al. 2013; Voscopoulos et al. 2013; Yoshida et al. 2015; Murouchi and Yamakage 2016). In the current study, we attempted to provide postoperative analgesia with an initial dose of local anesthetic. That is because in the preliminary study, most patients needed postoperative analgesics within 12 hours after breast cancer surgery. We thought that a single-shot RLB could provide sufficient analgesia for early postoperative analgesia. Moreover, we injected 15 ml of anesthetic at two different sites to provide more extensive spread of the local anesthetic: T2 for axillary lymph node dissection and T4 for a mastectomy. However, we could not demonstrate the efficacy of double-level RLB for analgesia within 12 hours after surgery. Our results suggest that a multi-level injection procedure may not be an advantageous technique for RLB. A recent anatomical study on pigs demonstrated that the local anesthetic distribution from the retrolaminar space to the paravertebral space was volume dependent (Damjanovska et al. 2018). We cannot directly apply their results to humans due to anatomical differences between the species. However, 15 ml of the local anesthetic injected in our study might not be sufficient to reach the PVS. Injection of 30ml of the local anesthetic in one site might be more effective than injection in two sites. Providing continuous injection or a higher cumulative dose of local anesthetic may be important for increasing the analgesic effect of RLB. Estimation of an optimal local anesthetic dose and search for an optimal combination of injection sites will be important to establish an appropriate RLB method in the future.
Recently, Forero et al. (2016) described an ultrasound-guided erector spinae plane (ESP) block for thoracic neuropathic pain and thoracoscopic surgery. They injected local anesthetics into the interfascial space between the erector spinae muscles and transverse processes. The injection site for this technique was close to that of RLB. The evaluation of the association between the injection site and the distribution of local anesthetics is also needed to establish these novel approaches of PVB.
A transient increase in plasma concentration of local anesthetics may have resulted in acute postoperative analgesic effects in this study. Karmakar et al. (2005) described the pharmacokinetics of a single bolus injection of ropivacaine (2 mg/kg) for a thoracic paravertebral block. They reported that the time to peak plasma concentration of ropivacaine was 7.5 minutes. Plasma concentration of ropivacaine in providing analgesia for breast cancer surgery has not been reported in RLB. Murouchi and Yamakage (2016) demonstrated that the time to peak levobupivacaine concentrations was 15 minutes after the initial dose of 0.375% levobupivacaine (75 mg, 20 ml). In our study, we used 150 mg of ropivacaine, which was close to the maximum dose. We could not conclude whether the plasma concentration of ropivacaine affected acute postoperative analgesia in this study. However, the systemic local anesthetic effect of the higher dose of ropivacaine used in our method might contribute to the lower NRS score noted within two hours postoperatively.
In our prior study, which is currently unpublished, 49% of patients who underwent breast cancer surgery with general anesthesia required postoperative analgesia within 12 hours following surgery. However, in the current study, we found that the ratio of patients requiring analgesics within the first 12 postoperative hours in the control group was 35.5%, which was lower than that in the prior study. The decrease in the ratio of patients requiring analgesics may have been caused by the improved, minimally invasive operative method. Consequently, we might not have been able to show the effectiveness of a double level RLB for postoperative analgesia in this study. The Kaplan-Meier survival curves for time to first analgesic administration could not demonstrate the difference between the groups.
This study had some limitations. First, we did not investigate the location of pain resulting from different surgical procedures. Investigation of the analgesic effect of RLB for each surgical method is required. Second, to ensure double-masking, we could not confirm whether the blocks themselves were effective using a sensory check procedure. Therefore, variation in the sensory block area was likely to influence the results. Third, we did not use an ultrasonographic imaging device to administer the RLB. Insertion of the RLB needle perpendicular to the skin helps avoid intralaminar puncture. This method of needle insertion is the same as a paramedian approach in epidural anesthesia, in which the local anesthetics were injected into the lamina. However, the position of the needle-tip was not confirmed with imaging; therefore, there might be variation in the spread of local anesthetics.
In summary, this study is the first double-masked, randomized control trial investigating the efficacy of RLB. We found that the RLB prolonged the time to initial administration of analgesics following breast cancer surgery and reduced the NRS pain score during the early postoperative period. However, the distribution of local anesthetics in a double-level RLB might be insufficient to provide postoperative analgesia after breast cancer surgery. The optimal dose of local anesthetic and the method of RLB (single-level or multi-level, single injection or continuous injection, and injection site) require further investigation in the future.

Schematic image of the retrolaminar block and axial view of the thoracic vertebra.
The needle is inserted 1 cm lateral to the spinous process and is advanced until it contacts the lamina. Local anesthetics injected upon the lamina (light blue area) spread to both the posterior branch and ramus cutaneous medialis (A), or to only the posterior branch (B).
The authors declare no conflict of interest.