2018 Volume 246 Issue 1 Pages 45-50
2018 Volume 246 Issue 1 Pages 45-50
Hearing loss is a common disease in older adults. In order to lower the prevalence of hearing loss, it is important to identify its risk factors. Although some studies have found a relationship between dental status and hearing acuity, few studies have investigated the relationship between unilateral chewing and hearing acuity. This study aimed to assess the effects of unilateral chewing on hearing acuity, with a focus on the risk of hearing loss. Eighty-one participants (aged 51-87 years) were included in the present study. Their chewing habits were determined by visual inspection. The participants were divided into two groups: the Unilateral Chewing Group (UCG; n = 43) and the Bilateral Chewing Group (BCG; n = 38). The preferred chewing side was identified for the UCG. Hearing acuity was determined using pure tone audiometry in a noise-free chamber, conducted at frequencies of 500, 1,000, 2,000, and 4,000 Hz. Hearing loss was defined as a lower hearing threshold greater than 50 dB in either ear at any frequency. Mean hearing thresholds at frequencies of 2,000 and 4,000 Hz were significantly higher, by 5.12 and 15.75 dB, respectively, for the UCG compared to the BCG (P < 0.05). The UCG had a 3.78-fold higher likelihood of suffering from hearing loss (95% confidence interval [CI]: 1.81-7.88). The results suggest that bilateral chewing could be beneficial for preventing hearing loss. This study may provide evidence to support clinical interventions aimed at reducing the risk of hearing loss in patients with unilateral chewing habits.
According to the World Health Organization (WHO), 360 million people around the world (5.3% of the world’s population) are suffering from hearing loss (World Health Organization 2012). In particular, the prevalence of hearing loss in adults aged 50 years and over is high (20-40%) (Gates et al. 1990; Wallhagen et al. 1997; Cruickshanks et al. 1998; Reuben et al. 1998). However, it can be difficult for older adults to recognize that they have hearing loss because of its relatively slow progression rate (Chou et al. 2011). Long-term hearing impairment can have a significant impact on a patient’s quality of life. Specifically, hearing loss can lead to problems with verbal communication, an increased susceptibility to depression and anxiety, and hostile behavior (Monzani et al. 2008). Therefore, it is important to identify the risk factors and reduce the prevalence of hearing loss.
The risk factors of hearing loss are varied, ranging from aging and noise exposure to systemic diseases like diabetes and cardiovascular disease. Moreover, dental status may also affect hearing acuity (Daniel 2007). Schell et al. (1999) compared hearing acuity in edentulous patients to that of fully dentulous patients. They found that fully dentulous patients had greater sound perception compared to edentulous patients. Similarly, Peeters et al. (2004) reported that patients without occlusal vertical dimension due to lack of prosthetic support had higher rates of hearing impairment. Likewise, in a longitudinal study (Lawrence et al. 2001), it was observed that participants who went from having ≥ 17 teeth to < 17 teeth had 1.64 times increased odds of suffering from hearing loss during a 20-year follow-up period.
To date, the majority of previous studies are limited to the relationships between dentition and hearing acuity. There are few studies exploring the association between masticatory habits and hearing acuity. In one example, Nagasaka et al. (2002) suggested that there is a relationship between unilateral chewing and hearing ability. In this study, patients were provided with proper occlusal treatment and chewing instructions to curb their unilateral chewing habits. Subsequently, their left and right side hearing acuity was equalized. Nevertheless, this study could not identify the risk of hearing loss associated with unilateral chewing. Alternatively, assessing the risk to hearing acuity associated with unilateral chewing could verify this relationship by quantifying its effect on hearing loss. Moreover, this quantitative data could be used to inform recommendations regarding clinical interventions for proper chewing habits. To our knowledge, no previous study has investigated the risk of hearing loss due to unilateral chewing. Hence, the present study aimed to assess the effects of unilateral chewing on hearing acuity, with a focus on the risk of developing hearing loss. The null hypotheses of this study were as follows: (i) there is no difference in hearing acuity between the Unilateral Chewing Group (UCG) and the Bilateral Chewing Group (BCG); (ii) left and right side hearing acuity is equal for the UCG; and (iii) there is no difference in risk of hearing loss for the UCG and BCG.
This study was approved by the Institutional Review Board of Gachon University (IRB No. 1044396-201612-HR-105-01) and was conducted in accordance with the Declaration of Helsinki. Eighty-one participants (aged 50 years and over) voluntarily participated in the present study between December 2016 and February 2017; participants were recruited from a healthcare center, which is a public gym for community dwellers, at Gachon University in Incheon, Republic of Korea. All participants were informed of the purpose of this study and gave informed consent. Participants without a history of ear disease, who had more than 20 functional teeth and who had complete occluding pairs in the posterior area were included in this study, as determined by questionnaire and oral examination. Participants who were identified as having a systemic disease (uncontrolled hypertension and diabetes), temporomandibular disorder (TMD), malocclusion, or oral pain, those who wore complete or partial dentures, and those who were edentulous, were excluded from the study.
Identifying participants’ chewing habitsVisual inspection, as described by Mc Donnell et al. (2004), was used to assess participants’ chewing habits. Participants were asked to chew sugar free gum naturally. A single examiner recorded the position of the gum every 15 seconds, and the procedure was repeated seven times. Participants who chewed consistently (7/7 times) or predominantly (5/7 or 6/7 times) on the same side were determined to have unilateral chewing habit. Participants were subsequently divided into two groups: the UCG and BCG (Fig. 1). For unilateral chewers, their preferred chewing sides (PCS) were identified.
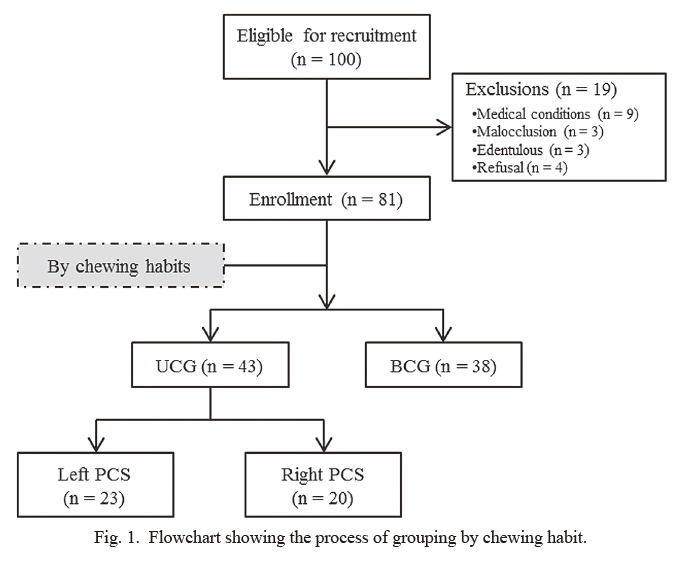
Flowchart showing the process of grouping by chewing habit.
UCG, unilateral chewing group; BCG, bilateral chewing group; PCS, preferred chewing side.
Hearing acuity was determined using pure tone audiometry (PTA) with an audio generator (DB-15000; Dongbo, Incheon, Korea) in a noise-free chamber by a single examiner who was blinded to the participants’ chewing habits. PTA measures the minimum pure tone threshold that participants can hear at a range of specified frequencies. Frequency indicates how high a sound is. PTA was conducted in speech frequency ranges (500, 1,000, 2,000, and 4,000 Hz); 500 Hz is low frequency, 1,000 and 2,000 Hz are middle frequencies and 4,000 Hz is high frequency. Pure tone thresholds were obtained over an intensity range of 50 to 100 dB in 10 dB increments. Using this system, a higher hearing threshold corresponds with lower hearing acuity. Hearing loss was defined as a hearing threshold greater than 50 dB in either ear at any frequency. The average hearing threshold at all frequencies was calculated according to the method prescribed by the Ministry of Health and Welfare, the Government of the Republic of Korea (2009). The formula is as follows: a + 2 × (b + c) + d, where a is the threshold at 500 Hz, b at 1,000 Hz, c at 2,000 Hz, and d at 4,000 Hz.
Statistical analysesThe age and sex distributions of groups were analyzed using a chi-square test. Differences in hearing threshold between groups were identified using an independent t-test. The Shapiro-Wilk test was used to test for normality for hearing thresholds in each ear. As the data were not normally distributed, Wilcoxon’s signed rank test was used to compare the hearing thresholds between ears. Logistic regression analysis was used to evaluate the effects of chewing habits on hearing loss. All statistical analyses were performed using IBM SPSS 23 software (IBM Corp., Armonk, NY, USA) with the statistical significance set at α = 0.05.
One hundred participants (aged 51-87 years) were recruited for this study. Nineteen participants were excluded because of medical conditions (n = 9), malocclusion (n = 3), edentulous condition (n = 3), or refusal to participate (n = 4). Thus, 81 participants were included in the final analysis. Thirty-eight (46.9%) of the participants included in this study had bilateral chewing habits and 43 (53.1%) had unilateral chewing habits. Among the UCG, 23 (53.5%) had left PCS and 20 (46.5%) had right PCS (Fig. 1). The mean participant age was 69.86 ± 8.29 years, with participants in their 70s accounting for the largest portion (49.4%). Age and sex distributions were balanced between the UCG and BCG; hence, there were no significant associations between chewing habits and age or sex (Table 1). Moreover, there was no significant difference in the hearing acuity according to age or sex (data not shown), indicating that age and sex did not act as confounding factors in this study.
The differences in hearing thresholds between participant groups are summarized in Table 2. Mean values for UCG hearing thresholds at frequencies of 2,000 and 4,000 Hz were significantly higher compared to the BCG (P < 0.05), by 5.12 and 15.75 dB, respectively.
Table 3 summarizes the differences in left and right side hearing thresholds. For participants with a left PCS, the left side hearing threshold (median 51.67 dB, interquartile range [IQR] = 50.00-58.33 dB) was significantly higher (P < 0.05), compared to their right side hearing threshold (median 50.00 dB, IQR = 50.00-53.33 dB). There were no statistically significant differences between left and right side hearing thresholds (P > 0.05) for the BCG or participants with right PCS.
Thirty-four participants within the UCG (79.1%) and 21 within the BCG (55.3%) had hearing loss (Table 4). Furthermore, a statistically significant association was found between chewing habits and hearing loss (P < 0.05). The UCG had an approximately 4 times higher risk of hearing loss compared to the BCG (odds ratio [OR]: 3.78, 95% confidence interval [CI]: 1.81-7.88).
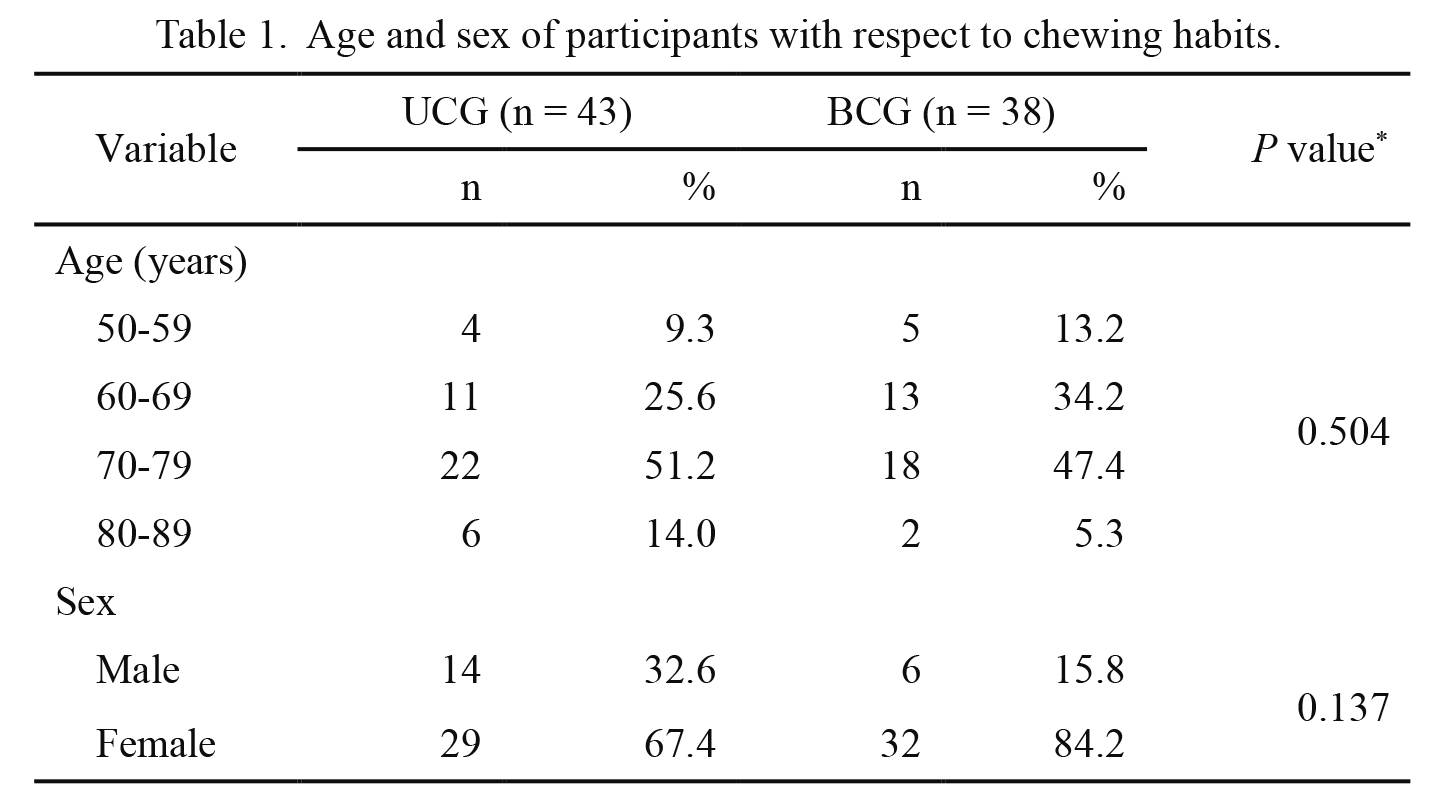
Age and sex of participants with respect to chewing habits.
UCG, unilateral chewing group; BCG, bilateral chewing group.
*Results were obtained by chi-square test.

Mean values of hearing threshold at different frequencies by chewing habits.
UCG, unilateral chewing group; BCG, bilateral chewing group.
Values are presented as mean ± standard deviation.
*P < 0.05, all p-values were obtained by independent t-test.
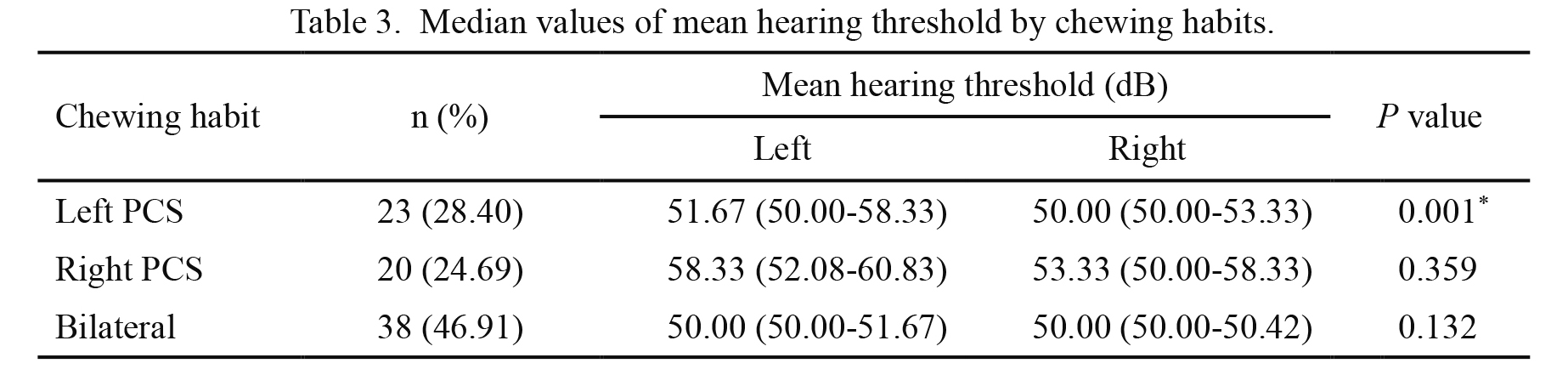
Median values of mean hearing threshold by chewing habits.
PCS, preferred chewing side.
Values are presented as median (1st quartile-3rd quartile).
*P < 0.05, all p-values were obtained by Wilcoxon’s signed rank test.

Risk of hearing loss by chewing habits.
*P < 0.05, results were obtained by logistic regression analysis.
Several studies have reported an association between oral function and hearing acuity owing to the anatomical correlation between the maxillofacial region and auditory system (Schell et al. 1999; Lawrence et al. 2001; Peeters et al. 2004). However, few studies have investigated the relationship between chewing habits and hearing acuity. Therefore, the present study aimed to assess the effects of unilateral chewing on hearing while focusing on the risk of hearing loss.
We found that the hearing threshold for the UCG was higher than that of the BCG at frequencies of 2,000 and 4,000 Hz (Table 2), which implies that hearing acuity was worse for the UCG. Hearing acuity can be measured at various frequencies; however, it is important to assess high frequency hearing loss to estimate difficulties in speech discrimination (Gunnar 1974). Hence, the result that the UCG had higher hearing thresholds at frequencies of 2,000 and 4,000 are relevant to participants’ hearing in everyday life. Importantly, these findings imply that unilateral chewing could result in poorer speech discrimination and subsequent difficulties with communication, which could lead to reduced quality of life (Dalton et al. 2003; Davis et al. 2007).
Participants in the UCG who had a left PCS had unbalanced hearing acuity; specifically, the hearing acuity for the chewing side was significantly worse than the right side (Table 3). It could, therefore, be concluded that unilateral chewing could make the hearing acuity of the chewing side worse. This finding is consistent with a previous study that suggested bilateral chewing instruction could decrease the gap in hearing thresholds between the left and right sides (Nagasaka et al. 2000). However, in the present study, there was no significant difference in hearing acuity between the sides for participants in the UCG with a right PCS. This could be due to a specific trend in hearing acuity of South Koreans. For South Koreans of older than 50 years, hearing is better for the right side (Ministry of Health and Welfare, the Government of the Republic of Korea 2012); therefore, the effects of unilateral chewing on hearing impairment may be less significant.
The present study showed that there was a significant association between unilateral chewing and hearing loss (Table 4). The risk of hearing loss for the UCG was approximately four-fold greater than for the BCG (OR: 3.78, 95% CI: 1.81-7.88). This suggests a strong association between unilateral chewing and hearing loss. This association can be explained by several mechanisms. First, hearing acuity could be impaired by temporomandibular joint (TMJ) sounds. Unilateral chewing is known as a risk factor for TMJ sound (Miyake et al. 2004), and individuals with unilateral chewing habits are more prone to unilateral joint clicking (Diernberger et al. 2008). Because repeated exposure to noise is a major cause of hearing loss (Rabinowitz 2000), TMJ sounds caused by unilateral chewing could potentially contribute to its development. Second, masticatory muscle overload resulting from unilateral chewing and subsequent nerve compression could damage hearing. It has been shown using electromyography that muscle activity on the chewing side increases significantly during mastication (Naeije et al. 1989; Kumai 1993). If masticatory muscle activity is unbalanced between the two sides due to unilateral chewing, subsequent unilateral muscle overload could place strain on the surrounding nerves and, hence, worsen hearing loss. Excessive strain on nerves surrounding the TMJ (e.g., chorda tympani and auriculotemporal nerves) can result in ear symptoms such as tinnitus and hearing impairment (Costen 1934). In addition, abnormal pressure on the nerves around the TMJ due to unilateral chewing could induce Eustachian tube dysfunction (Myrhaug 1964) and subsequent hearing loss (Robinson and Hazell 1989). Third, altered brain activity during unilateral chewing could have an effect on hearing acuity. An association between unilateral chewing and cerebral cortex activity has been identified in several studies (Jiang et al. 2010, 2015). Moreover, unilateral chewing inhibits the response of the primary auditory area (Kobayashi et al. 2004), thus contributing to hearing loss.
The present study has several limitations that need to be considered. First, because hearing thresholds were measured over a range of 50-100 dB, hearing loss might be underestimated due to the absence of a lower hearing threshold. Nonetheless, 50 dB is the point at which people have difficulty with normal conversation (Daniel 2007). Therefore, our finding could be applied to people who have trouble communicating with others due to hearing loss. Second, causal relationships cannot be established based on cross-sectional studies. Hence, follow-up studies are required to demonstrate this relationship more definitively.
Based on the present study, we found an association between chewing habits and hearing acuity. This finding suggests that bilateral chewing could be beneficial for preventing hearing loss. To our knowledge, this is the first study to quantify the risk of hearing loss induced by unilateral chewing. Although further studies are needed to verify the causal relationship, this study may provide important evidence to support clinical interventions aimed at reducing the risk of hearing loss in patients with unilateral chewing habits.
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (grant No. 2016R1D1A1B03934754).
The authors declare no conflict of interest.