2018 Volume 246 Issue 4 Pages 205-212
2018 Volume 246 Issue 4 Pages 205-212
Hip fracture is a worldwide medical problem with devastating consequences. Older adults are at higher risk for complications and have more mobility limitation. The aim of this study was to assess the impact of delay in out-of-bed functional exercise on one-year mortality and functional outcomes for elderly patients with hip fracture in China. 1,022 cases of patients with hip fracture who were older than 75 were involved in this retrospective cohort study between 2007 and 2017. One-year mortality, follow up Activities of Daily Living (ADL) score, and Harris hip score were collected. Patients with hip fracture experienced an average of 2.9 days of in-bed functional exercise, 41.4% (n = 423) taken out-of-bed functional exercise within 2 days. A Cox proportional regression model showed that after adjustment for age, sex, cardiovascular disease, and urinary disease, delayed out-of-bed functional exercise (> 2 days) associated with higher one-year mortality (OR = 1.38, 95% confidence interval [CI]: 1.09 to 1.69). Ordinary least squares regression showed that delayed out-of-bed functional exercise associated with worsen ADL scores at 1-month (difference of –3.9 points, 95% CI: –6.4 to –1.7), although the long term ADL scores did not have increased. In addition, there were no associations between out-of-bed functional exercise timing and the Harris hip score at 12 months. In conclusion, in elderly patients with hip fracture in China, delayed out-of-bed functional exercise was not associated with improved Harris hip score, but it was associated with worsen ADL capacities at 1-month postoperatively and higher one-year mortality. The present study emphasizes the benefit of early out-of-bed exercise on the majority of elderly patients with hip fracture.
Hip fracture is a worldwide medical problem with devastating consequences. There are 1.3 million and 1.6 million hip fractures reported in 1990 and 2000 worldwide, respectively (Cummings and Melton 2002; Johnell and Kanis 2004), and the amount still goes on. It was estimated that by 2050, the number of hip fractures would increase to 4.5 million worldwide (Gullberg et al. 1997). In many cases, hip fracture is a prototypical geriatric disease, with characteristics of frail, functional deterioration and comorbidities (Auais et al. 2013). Besides, a 5 to 8 fold increased risk of death was occurred among elderly patient in the months following surgery (Haentjens et al. 2010), placing a significant burden on healthcare systems (Fransen et al. 2002). After a fracture, the outcomes for elderly patients are generally poor, with increased 1-year mortality reaching 18-33% (Bentler et al. 2009), and approximately 40% of survivors do not recover from their pre-fracture ambulatory 1 year later (Braithwaite et al. 2003; Hung et al. 2012; Savino et al. 2013).
Although surgical repair is gradually considered to be the predominant treatment strategy in improving outcomes of hip fracture (Orosz et al. 2004), immobilization ascribed to surgery and hospitalization lead to an increase risk of morbidity and a decline in muscle function, especially in frail elderly patients (Suetta et al. 2007). It is reported that immobilization led to an approximately 4% declines of muscle strength per day during the first week after surgery (Wigerstad-Lossing et al. 1988). Exercise rehabilitation after operation is considered to be of the essence in improving physical function and in reducing disability (Binder et al. 2004; Handoll et al. 2011; Auais et al. 2012). Factors including the training intensity (Latham et al. 2004), care settings (home-based rehabilitation, community-based rehabilitation, inpatient rehabilitation) (Handoll et al. 2011), and exercise timing is related to the clinical outcomes after hip fracture. For instance, elderly patients who undergo hip-fracture surgery can benefit from intensive physical training that is initiated early in the post-operative phase (Suetta et al. 2004). Practice guideline recommended early mobilisation as it may prevent deep vein thrombosis and pressure damage (Kamel et al. 2003; Siu et al. 2006). It has been stated that delayed ambulation after hip fracture surgery is associated with an increased in length of hospital stay and new onset delirium (Kamel et al. 2003). Older adults are at higher risk for complications and have more mobility limitation compared with their younger counterparts. Therefore, whether in-bed functional exercise combined with out-of-bed functional exercise influence elderly patients’ mortality and quality of life need to be further investigated.
In this study, we aim to evaluate the impact of time to out-of-bed functional exercises on one-year mortality and functional outcomes in Chinese elderly patients with hip fracture. A secondary aim was to investigate whether time to out-of-bed functional exercises influence the postoperative length of hospital stay and comorbidities.
In our retrospective cohort study, we aim to evaluate the effect of out-of-bed functional exercise timing on mortality and functional outcomes (Activities of Daily Living (ADL) score and Harris hip score). Between April 2007 and April 2017, people with hip fracture who were older than 75 years of age and admitted to hospital were included in this study. We accessed the historical data of the cohort from medical records from Traditional Chinese Medicine Hospital of Puning City.
Inclusion criteria were (1) patients undergoing primary hip fracture; (2) being aged 75 years or older; (3) receiving surgical repair within 1 week; (4) able to understand and communicate in Chinese; and (5) having ADL score, Harris hip score questionnaire and recorded timing of exercise. Exclusion criteria were as follows: (1) a terminal disease (survival expected to be < 1 year), (2) pathological fracture, (3) bilateral or additional fractures other than the femur, and (4) missing information or inaccurate information on the date of functional exercise and follow up data.
We compared clinical outcomes between patients taking out-of-bed functional exercise within 2 days and those who taking out-of-bed functional exercise after 2 days. The reporting of the study follows the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) Statement, using the STROBE Checklist (von Elm et al. 2007). STROBE Statement is a clinical guideline for observational studies which aimed to developed recommendations on what should be included in an accurate and complete report of an observational study. This study was approved by the Traditional Chinese Medicine Hospital of Puning City. All patients provided informed consent to participate in the study.
Hip fracture diagnosis and treatmentThe initial diagnosis of a hip fracture was made by experienced orthopedic surgeon. Hip fractures are classified as intracapsular (femoral neck fractures and transcervical fractures) or extracapsular fracture (per-, inter- and sub-trochanteric). Among them, femoral neck fractures and intertrochanteric fractures account for more than 90% of hip fractures. For both patients with femoral neck fracture and with femoral intertrochanteric fracture, mini-incision posterolateral approach in total hip arthroplasty was conducted.
Functional exercise interventionAfter surgery, three experienced physical therapists supervised the functional exercise and all the participants performed it independently in the department of rehabilitation. In-bed functional exercises include ankle dorsiflexion and extension, isometric quadriceps contraction, and straight-leg raising exercise. The duration of each exercise was 10 s, and 3 sets of 20 repetitions were performed per day. Out-of-bed exercises include sit-to-stand training using a crutch or fixture, and strengthening program (standing knee flexion, hip flexion and extension, and hip abduction). Patients able to perform either sit-to-stand training or strengthening program for 30 min (or more) were considered successful out-of-bed exercises.
At discharge, patients received a pamphlet with the description of suggested exercises described above to be continued at home and were encouraged to perform the exercises twice a day in their maximum possible range of motion at the first 3 months. All patients were encouraged to supplement the hip exercises with aerobic training by walking, and gradually return to their usual activities.
Outcome measureA blinded outcome assessor evaluated the participants’ outcome pre-operatively and at 1, 6, 12 months post-operatively. We evaluated physical function (using Barthel Index of ADL to assess fundamental skills), mortality (one-year), and hip function (using Harris hip score). ADL was measured with the score range from 0 to 100, with 100 represent the best possible score (Mahoney 1965). Harris hip score was evaluated according to a previous study reported in 1969 (Harris 1969), which covers (1) pain (pain severity), (2) function (daily activities and gait), (3) absence of deformity (hip flexion, adduction, extremity length discrepancy, and internal rotation), and (4) range of motion. Harris hip score has 10 question items and score range from 0 to 100, with higher score representing less dysfunction and better outcomes. The outcome data was collected by telephones or clinical follow-up, with Harris hip score collected by clinical follow-up only.
Sample sizeA PASS statistical software was used to estimate the minimum sample size for this study. Based on the pre-clinical experiment, participants who taken out-of-bed functional exercise within 2 days had a mortality of 10.2% one year after surgery, while delayed out-of-bed functional exercise (> 2 days) showed a mortality of 17.3% one year after surgery. Thus, using PASS statistical software (version 11), setting a two sided test with significance of 0.05, power level of 1-β = 0.80 and S1 (proportion surviving in group 1) = 0.827, S2 = 0.898, proportion in group 1 = 0.5, and proportion lost during follow up = 0, we found that a minimum of 373 patients were needed for each group. Considering a 10% dropout of sample during sample collection, we need at least 373 / (1-10%) = 415 sample for each group.
Statistical analysisCategorical data are presented as percentages as well as the actual values used to calculate the percentages. Continuous data are presented as mean and standard deviation (SD). Group comparisons for categorical variables were performed using the χ2 test with the corresponding degrees of freedom, and for continuous variables Student’s t test were performed. To control for factors that might affect outcomes and functional exercise timing, we used ordinary least squares regression for continuous outcomes (such as ADL score and Harris hip score), and logistic regression for binary outcomes. In addition, Cox proportional hazards models were used to determine factors associated with one-year mortality. For all analyses, SPSS 19.0 was used for statistical analysis, and P < 0.05 was considered statistically significant.
Between April 2007 and April 2017, a total of 1,608 patients with hip fracture were consecutively enrolled in the study. Of these, 586 patients were excluded from the analysis (386 did not meeting inclusion criteria, 102 refused to participate, 57 were not possible to contact, and 41 did not have to follow up data) (Fig. 1). Of the remaining patients (n = 1,022), the mean number of days from post-operation to out-of-bed functional exercise was 2.9 ± 1.8 days (interquartile range, 1-9 days). In addition, only 5.7% (n = 58) taken out-of-bed functional exercise at day 1 postoperatively, 35.7% (n = 365) taken out-of-bed functional exercise at day 2 postoperatively, 58.6% (n = 599) taken out-of-bed functional exercise 2 days more after surgery.
As shown in Table 1, the mean age of all participants was 83.0 years (SD 4.7), and 687 of these (67.2%) were female. Compared to patients who had taken out-of-bed functional exercise within 2 days after surgery, patients who had delayed out-of-bed functional exercise were more likely to have comorbidities. There was no significant difference in length of stay (LOS) between groups, with 11.93 days (2.45) in the early out-of-bed functional exercise group, and 12.21 days (5.12) in the later out-of-bed functional exercise group. In addition, ADL score at baseline patients did not differ between the groups. Of the patients, more than 30% of the participants had femoral intertrochanteric fracture, and 70% had femoral neck fracture.

The flow chart of the enrollment and follow-up of the study patients.
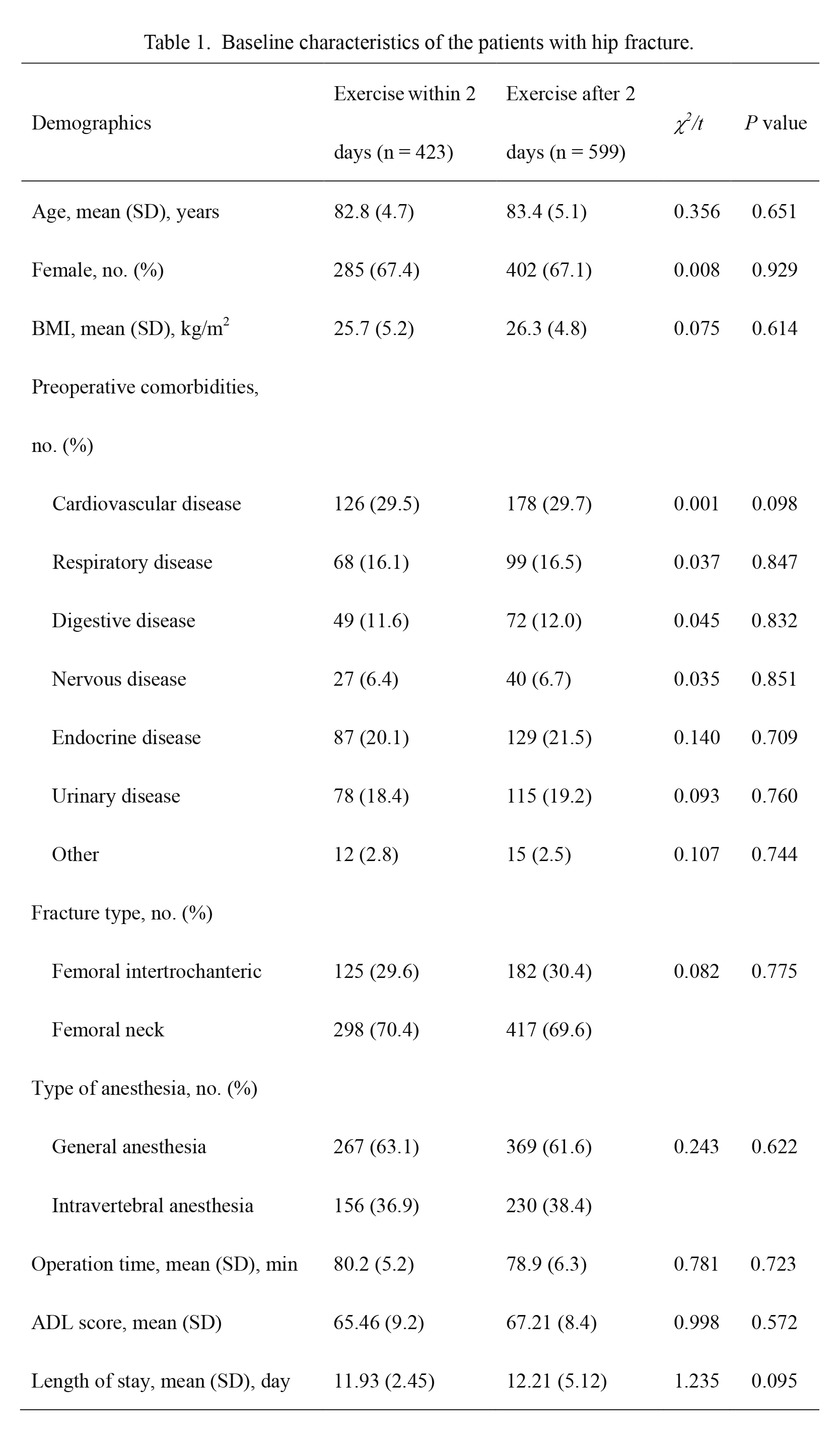
Baseline characteristics of the patients with hip fracture.
Exercise, out-of-bed functional exercise; BMI, body mass index; ADL, activities of daily living.
Cardiovascular disease include coronary atherosclerotic heart disease (such as angina and myocardial infarction), hypertension, cardiomyopathy, and heart arrhythmia; Respiratory disease include Chronic bronchitis, pulmonary infection, and tuberculosis; Digestive disease include Hepatobiliary disease, pancreas and gastroduodenal diseases, and hypoalbuminemia; Nervous disease include Cerebral infarction, cerebral hemorrhage, transient ischemic attack, and Alzheimer’s disease; Endocrine disease include Diabetes, and thyroid disorders; Urinary disease include Nephritis, bladder disease, and prostate disease.
One-year mortality was 15.5% (n = 158) in the overall sample, 11.1% (n = 47) in the 423 patients who had out-of-bed functional exercise within 2 days and 16.9% (n = 101) in 599 patients who had delayed out-of-bed functional exercise. In bivariate (unadjusted) analyses, increasing age (hazard ratio (HR) = 1.42, 95% confidence interval (CI): 1.34 to 1.51), female sex (HR = 1.12, 95% CI: 1.05 to 1.20), cardiovascular disease (HR = 1.54, 95% CI: 1.46 to 1.65), urinary disease (HR = 1.38, 95% CI: 1.21 to 1.59) and out-of-bed functional exercise (HR = 1.57, 95% CI: 1.11 to 2.23) were associated with increased one-year mortality (Table 2). After adjustment for age, sex, cardiovascular disease, and urinary disease (Table 3), delayed out-of-bed functional exercise was associated with higher one-year mortality (odds ratio (OR) = 1.38, 95% CI: 1.09 to 1.69).

Unadjusted associations between selected characteristics of patients and one-year mortality.
HR (95%CI), hazard ratio at 95% confidence interval.

Comparison of outcomes for patient taken out-of-bed exercise within 2 days and after 2 days.
Adjusted for age, sex, cardiovascular disease, urinary disease and pre-operative ADL score (or pre-operative HHP).
ADL, activities of daily living; HHP, Harris hip score; OR (95%CI), odds ratio at 95% confidence interval.
Multiple linear regression analysis showed that time-to-out-of-bed functional exercise was not associated with Harris hip score at 12 months (–0.9 points; 95% CI, –3.1 to 1.2 points). Compared with patients with early out-of-bed functional exercise in adjusted analyses, patients with delayed out-of-bed functional exercise had worsen ADL score at 1 month (–3.9 points; 95% CI, –6.4 to –1.7 points; with higher values indicating better function), but no significant difference in ADL score by 6 months (–1.6 points; 95% CI, −3.1 to 0.2 points) and 12 months (–1.2 points; 95% CI, −2.9 to 0.7 points).
Recently, several studies indicated that regular exercise (aerobic and/or resistive) is related to improved physical performance (e.g., gait, strength) (Resnick et al. 2010), walking speed (Hauer et al. 2002), and mobility (Tinetti et al. 1999; Sherrington et al. 2004). Binder et al. (2004) conducted a randomized control trial of a 6-month supervised physical training, and found an improvement in muscle strength and quality of life, suggesting the importance of exercise post-operatively. Besides that, practice guideline suggested early mobilisation post-operation. Functional exercise contains in-bed exercise and out-of-bed exercise. However, some of the studies limited by small sample size (Kamel et al. 2003, Oldmeadow et al. 2006), as well as lack of long-term follow-up with examining the results available at the initial post-operative (i.e., Six days after surgery) (Morri et al. 2018). In addition, many of patients with hip fracture in China prefer to take in-bed functional exercise rather than out-of-bed ones in the first few days after operation. Thus, this study was performed to investigate the effect of timing of out-of-bed functional exercise on clinical outcomes for elderly patients with hip fracture in China. In this retrospective cohort study, we found that compared with patients who initiating out-of-bed functional exercise within 2 days post-operatively, patients with delayed out-of-bed functional exercise have lower ADL scores at early stage of post-operative and higher one-year mortality.
We also have found that mortality during hospitalization was 2.5% in the overall sample, which was somewhat lower than the value of 4.5% reported by Kim et al. (2012). This study showed that the one-year mortality was 15.5% in the overall sample, 11.1% in the early out-of-bed functional exercise group and 16.9% in the late functional exercise group, which is in accordance with previous reports that one-year mortality have varied from 14% to 30% among patient with hip fracture (Simunovic et al. 2010; Cenzer et al. 2016). In addition, we found that time-to-out-of-bed functional exercise was associated with the one-year mortality, even after adjusting for age, sex, cardiovascular disease, and urinary disease. Our results are consistent with a previous study which showed that delay in getting the patient out of bed is associated with worsened 6-month survival (Siu et al. 2006).
For functional outcomes, it had been reported that the mean HHS at six months post-arthroplasty is 93 scores, while increased to 96 scores at three years (D’Antonio et al. 1992), with small differences of clinically relevant in HHS. However, other study argues this finding since ceiling effects limit the validity of HHS in arthroplasty research on outcomes (Wamper et al. 2010). The present study showed that time-to-out-of-bed functional exercise was not associated with Harris hip score at 12 months (–0.9 points; 95% CI, –3.1 to 1.2 points). The Harris hip score was chosen as the outcome measure mainly because it’s more responsive as compared with the test of walking speed and pain in patients with hip fracture (Hoeksma et al. 2003). On the other hand, Harris hip score is a clinician-based outcome measure administered by a qualified health care professional, while other hip fracture function measurement, such as Oxford Hip Score, as well as Hip Disability and Osteoarthritis Outcome Score are patient-reported. The discrepancy of the questionnaire results of total hip arthroplasty increased when the patient was not satisfied with the outcome. Therefore, the use of patient-reported questionnaires as well as clinician-based assessments may provide a more complete evaluation of the results of total hip arthroplasty (Lieberman et al. 1996). In addition, the present study indicated that early out-of-bed functional exercise group enjoyed an improved ADL capacity at the 1-month follow-up, but not at 6 or 12-months follow-up. This finding was in agreement with previous study showing that delayed ambulation after hip fracture is associated with the onset of delirium and pneumonia postoperatively (Kamel et al. 2003). However, a Cochrane review of 9 heterogeneous trials of 1,400 patients comparing exercise interventions summarized that there was insufficient evidence to recommend physical intervention after hip fracture (Crotty et al. 2010). The main reasons for these discrepancies are that studies have varied greatly with regard to program content and type of exercises (aerobic, resistance training, and functional training); delivery site (gym, clinic, or patient’s home); time of initiation after fracture; intensity and duration of program.
There are several potential limitations in our study. First, as it was not possible to delay out-of-bed functional exercise intentionally, corresponding randomized trial is not likely to be done. It is possible that we did not adjust for some other factors (for example, the psychometric characteristics) that might affect the results; the factors were chosen to the best of our current knowledge. Second, we lacked data on pre-fracture ADL score and Harris hip score, which may have affected follow-up ADL score and Harris hip score. Instead, we adjusted for pre-operation ADL score and Harris hip score.
In conclusion, in elderly patients with hip fracture, delayed out-of-bed functional exercise after 2 days was not associated with improved Harris hip score at 12 months. However, it was associated with worsen ADL scores during the early post-operative period, and higher one-year mortality. Our data emphasizes that early out-of-bed exercise should be a goal for the majority of elderly patients with hip fracture.
This study was supported by Guangdong Provincial Science and Technology Project (2011A032100001), and by Youth Research Project of Guangdong Second Provincial General Hospital (YQ2017-011).
The authors declare no conflict of interest.