Abstract
Antiretroviral therapy (ART) has been introduced recently and has significantly impacted morbidity and mortality, but can also engender drug resistance. To identify the prevalence of HIV-1 drug resistance (HIVDR) among patients with antiretroviral therapy failure in Sichuan during the period from 2010 to 2016, we carried out a longitudinal study in Sichuan, a province with the highest HIV/AIDS prevalence in China. The data and blood samples were collected from HIV/AIDS patients who received ART for more than half a year. Overall 5,512 sequences were completed from 7,059 ART-failure patients, and 2,499 individuals were identified as drug resistant. Among those with HIVDR mutations identified, 25.37% were against non-nucleoside reverse transcriptase inhibitors (NNRTIs), and 1.60% was against nucleoside reverse transcriptase inhibitors (NRTIs). NRTI-resistant drugs were mainly lamivudine (3TC) (57.77%) and emtricitabine (FTC), while NNRTI-resistant drugs were mainly nevirapine (NVP) (91.13%) and efavirenz (EFV) (72.81%). The most common recombination subtypes of HIV-1 in sequenced samples were CRF07_BC (circulating recombinant form, CRF) (41.42%), followed by CRF01_AE (40.77%). Moreover, drug resistance rate increased with the prolongation of treatment time (χ2 = 14.758, P < 0.05). The overall prevalence of acquired drug resistance in HIV-1 infected patients in Sichuan was 5.47%, which has remained relatively stable from 2010 to 2016. HIV-1 CRF01_AE and CRF07_BC subtypes were the main epidemic strains, and the possibility of resistance was higher in CRF01_AE subtypes. The current study highlights the importance of acquired drug resistance surveillance over a long period.
Introduction
Acquired immunodeficiency syndrome (AIDS) is a major pandemic disease (GBD 2015 HIV Collaborators 2016). More than 36 million people have been infected in the world, and 59% of these people received antiretroviral therapy (ART) (WHO, World Health Organization 2017). In 2003 the National Free Antiretroviral Therapy program was initiated by Chinese government to provide free highly active antiretroviral therapy (HAART) (Zhao et al. 2012), and about 64% of HIV-1 infected individuals were receiving ART in China (NCAIDS, The Chinese Center for AIDS Prevention and Control et al. 2016, 2018). Moreover, Sichuan province, located in West China, is characterized by the largest population having a large number of HIV/AIDS across China with 92,976 HIV/AIDS patients alone (Data and Statistics information from the Sichuan Center for Disease Control and Prevention) by the end of 2016. The increasing ART coverage there increased from 23.01% in 2010 to 74.02% in 2016. Thus, continued usage of ART programs will require understanding the emergence of HIV drug resistance patterns among individuals in whom treatment has failed and managing ART from both an individual and public health perspective (WHO 2013; Manasa et al. 2013; Xing et al. 2013).
The HIV drug resistance (HIVDR) poses a major public health challenge. In resource-limited settings where ART access is being scaled-up, the WHO recommends surveillance of HIVDR (Bennett et al. 2008; Jordan et al. 2012). Hence, ongoing surveillance of drug resistance plays a main role for the design of strategies to prevent and control the evolution and the emergence of resistance (Hecht et al. 2006). In China, some provinces and municipalities began to establish an HIV resistance surveillance network to assess and prevent HIVDR in 2003. A large number of prevalent strains observed in Sichuan clearly indicate the emergence of HIVDR (Su et al. 2014). Though an HIV-resistant strain has a low-prevalence in most areas, the resistance of patients with ART is more serious in some regions (Li et al. 2007; WHO 2012). A few studies have been documented regarding the prevalence of HIV resistance in Sichuan province towards significant epidemics in cities and counties (Zhong et al. 2003; Hallack et al. 2008; Hirsch et al. 2008), but they were conducted using a cross-sectional setting or included surveillance for only a short period of time. To the best of our knowledge, there were no data on long-term monitoring of the prevalence of in drug resistance in Sichuan with the largest HIV/AIDS population across China.
Therefore, the specific objective of the present study was for the first time to provide an overview and pooled prevalence estimate of HIV infection status and the prevalence of HIVDR over a 7-year period in HIV-infected ART-failure individuals from Sichuan province during 2010-2016. Through HIV resistance surveillance, we are able to evaluate the antiviral treatment effect of HIV/AIDS patients and predict the future development trend of HIVDR in Sichuan. Furthermore, the information presented can also inform antiretroviral regimen choices, improve guidelines for drug resistance testing, and identify potential gaps in treatment and prevention strategies, especially in resource limited regions.
Methods
Ethical statement
The study protocol was approved by the National Natural Science Foundations of China Review Board (81502801 and 81473020) and National Mega Projects of Science and Technology in 13th Five-Year Plan of China: Technical Platform for Communicable Disease Surveillance Project (No. 2017ZX10103010-002).
Participants and specimens
A study was carried out at the Sichuan Provincial Center for Disease Control and Prevention. The information about epidemiological characteristics of HIV/AIDS from 2010 to 2016 in Sichuan Province was collected with the AIDS comprehensive prevention and treatment information system of China Center for Disease Control and Prevention. Data on demographic characteristics were collected during the interview. The EDTA-K2 anticoagulated plasma of HIV-1 patients who received ART for more than half a year in Sichuan Province (except Liangshan Yi Autonomous Prefecture) were collected and separated. Real-time molecular beacon detection was applied to detect the viral load of HIV (NucliSens EasyQ Analyzer, BioMerieux, Lyon, France).
Nucleic acid extraction, amplification, and sequencing
The viral nucleic acid was extracted from 200-μl plasma of patients with a viral load of more than 1,000 copies/ml (according to WHO guideline, we defined viral load ≥ 1,000 copies/ml after 6 months of treatment with ART as virological failure) by using an automatic extraction machine (MagNA Pure LC 2.0 system, Roche, Branchburg, NJ, USA) according to the approved guidelines. The full-length protease gene in Pol region (1.3-kb fragment) and the first 300 codons of the reverse transcriptase gene were amplified by RT-PCR, as described previously (Liao et al. 2007). The PCR products were tested by electrophoresis with 1% agarose gel. The products of about 1,300 base pairs were sent to Beijing Genomics Research Center Ltd. for purification and gene sequencing.
Sequencing and Drug-resistance analyses
The obtained sequence was analyzed by using the analysis software ChromasPro1.33. The BioEdit Sequence Alignment Editor (Ibis Biosciences, Carlsbad, CA, USA) was used to edit and correct the sequence. DNAStar (Madison, Wisconsin, USA) software was used to determine the subtype. Drug-resistance profiles of ART patients were analyzed based on genotypic and phenotypic interpretations defined by the Surveillance Drug Resistance Mutation list recommended by the World Health Organization, and the Stanford University HIV Drug Resistance Database (http://hivdb.stanford.edu), which can analyze resistant mutations and species online, as well as HIV virus sensitivity to antiviral drugs.
Statistical analysis
Data were entered in a spreadsheet (MS Excel 2010) and analyzed using SPSS V22.0 (SPSS, Chicago, IL, USA). The demographic characteristics (sex, age, ethnicity, vocation, and transmission category) were expressed in percentage. The χ2 test and Fisher’s exact probabilities methods were used to compare the difference in the frequency of occurrence of drug-resistant loci and the frequency of high drug resistance among different subtypes of strains. Trend χ2 test was used to analyze the relationship between treatment time and drug resistance. A P value < 0.05 was considered statistically significant.
Results
The HIV/AIDS epidemic in Sichuan from 2010 to 2016
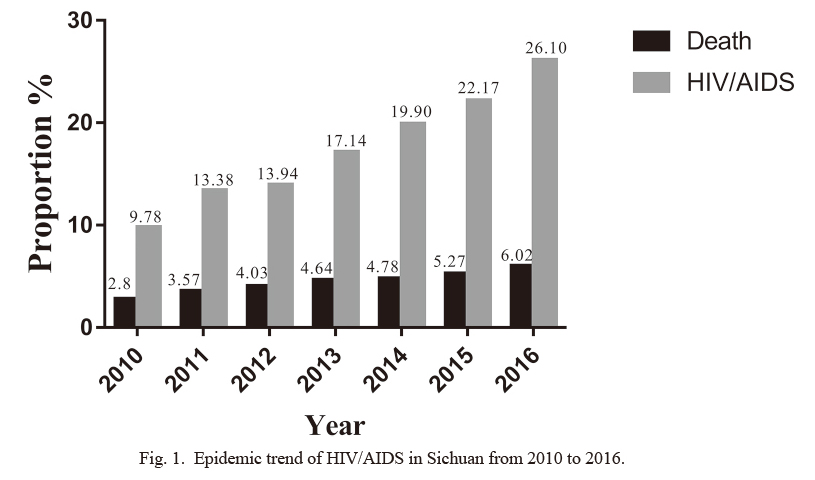
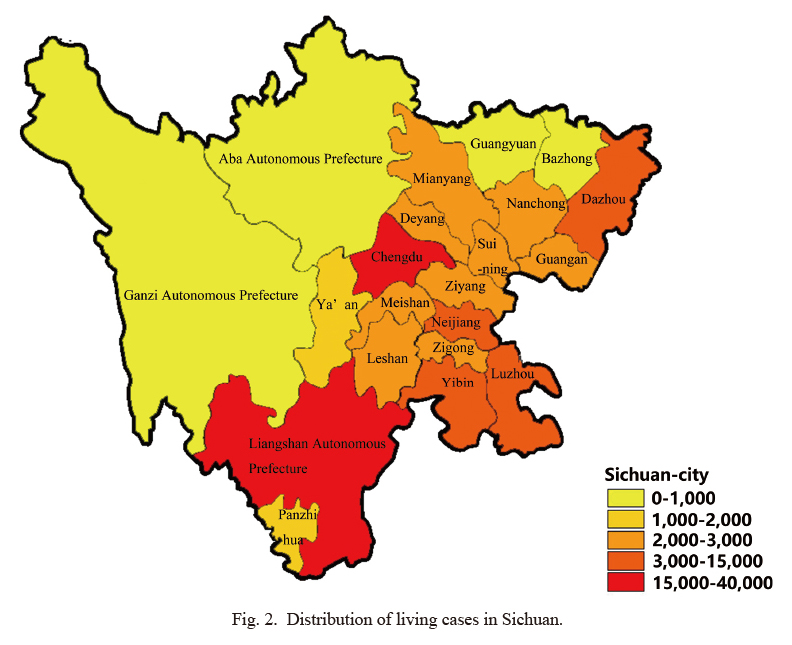
Data included a population of HIV/AIDS infection and death per year in Sichuan from 2010 to 2016. By the end of December 2016, there were 92,976 AIDS cases, and the epidemic situation exists in 183 districts (cities and counties) in Sichuan province. Over the past seven years, the number of patients in Sichuan has increased along with the number of deaths (Fig. 1). The epidemic situation of AIDS in Sichuan was serious in some areas. Of all the subjects, 31,764 (34.16%) were in Liangshan Yi Autonomous Prefecture, and 19,415 (20.88%) were in Chengdu, with relatively low numbers in Ganzi (0.3%) and Aba (0.84%) Autonomous Prefecture. At the end of 2016, the distribution of living cases in Sichuan province is shown in Fig. 2.
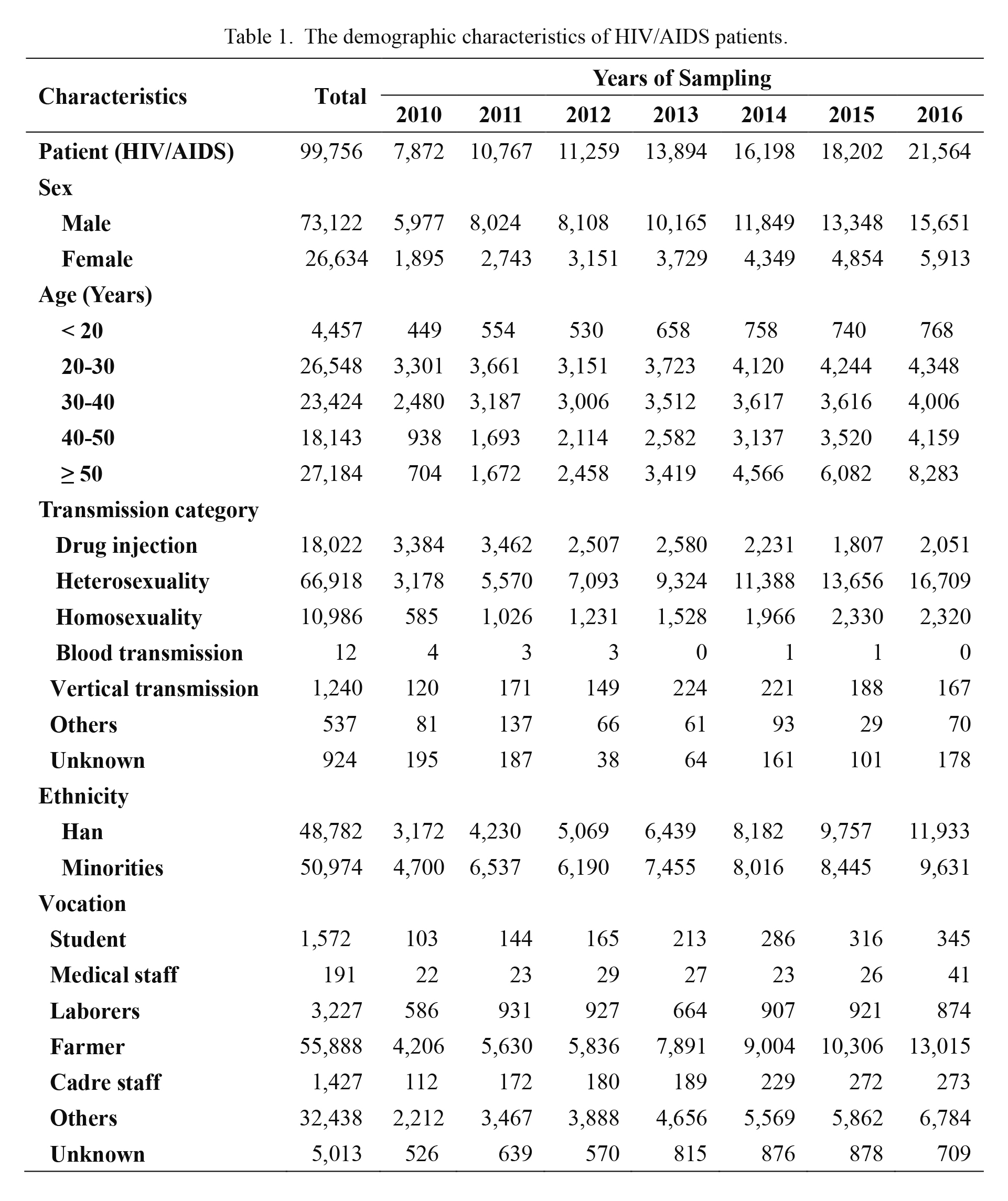
Demographic profiles
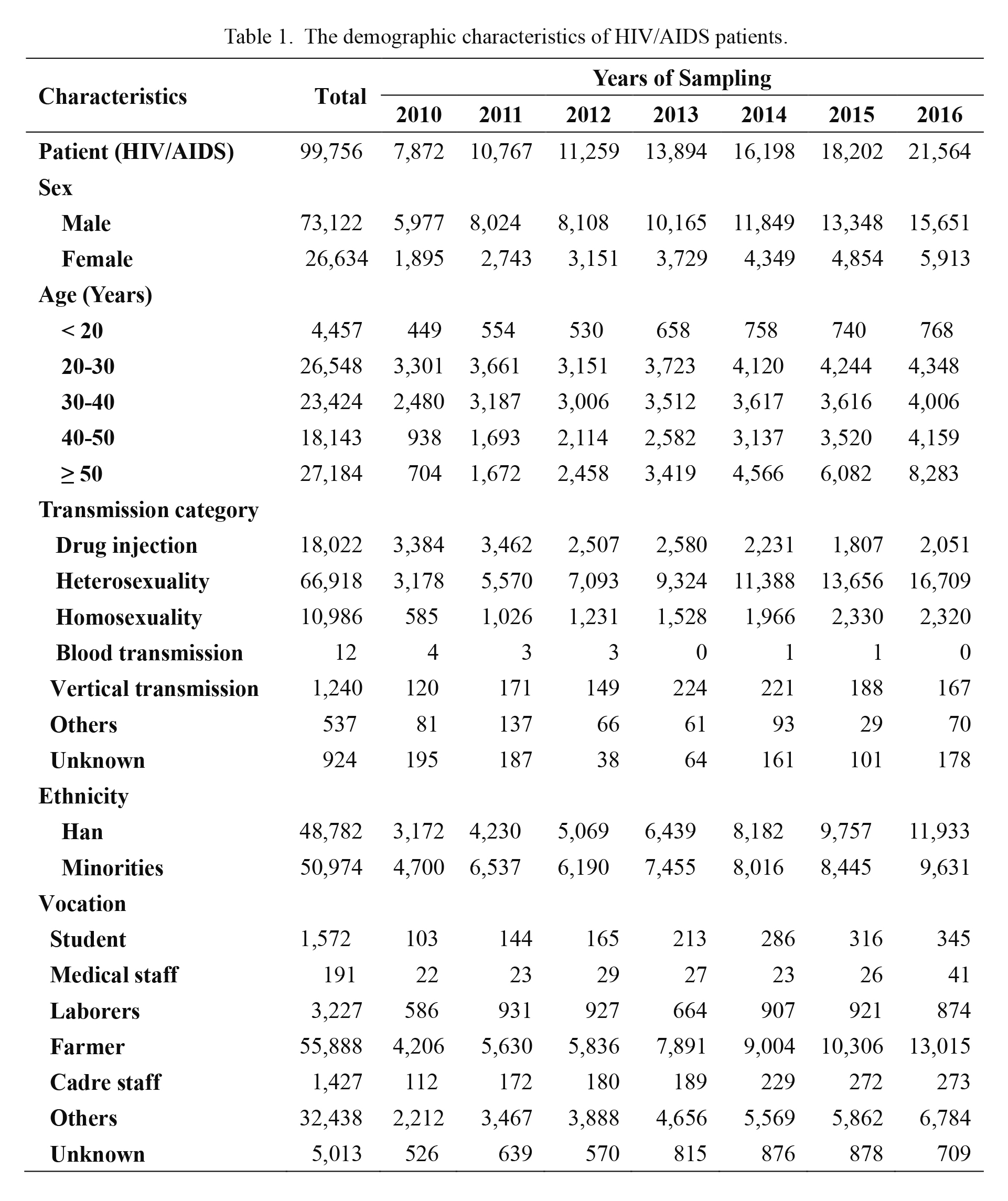
Of the 92,976 patients from 2010 to 2016, 58,897 (63.35%) were HIV infected patients, 34,079 (36.65%) were AIDS patients, and 73,122 (78.65%) were males (Table 1). There are fifty-five minority ethnic groups in China, and minority nationality (Chinese except for the Han nationality) occupies 6.1% of the population in Sichuan (National Bureau of Statistics of China 2011). About 51% of the HIV/AIDS patients belong to minority nationality, which is occupying more than half of the infected individuals in Sichuan. Heterosexual transmission was the major route of disease spread (71.97%), followed by injection drug use (19.38%), homosexuality (11.82%), mother-to-child transmission (1.33%) and blood products (0.01%). Spread of HIV through heterosexual contact has significantly increased as compared with injection drug and vertical transmission (Yuan et al. 2015). The professions of patients were widely distributed; they were mostly farmers (60.11%). The age distribution was still mainly in young adults aged 20-40 years old (53.75%), but the proportion of the older population, aged 50 years and over, has increased.
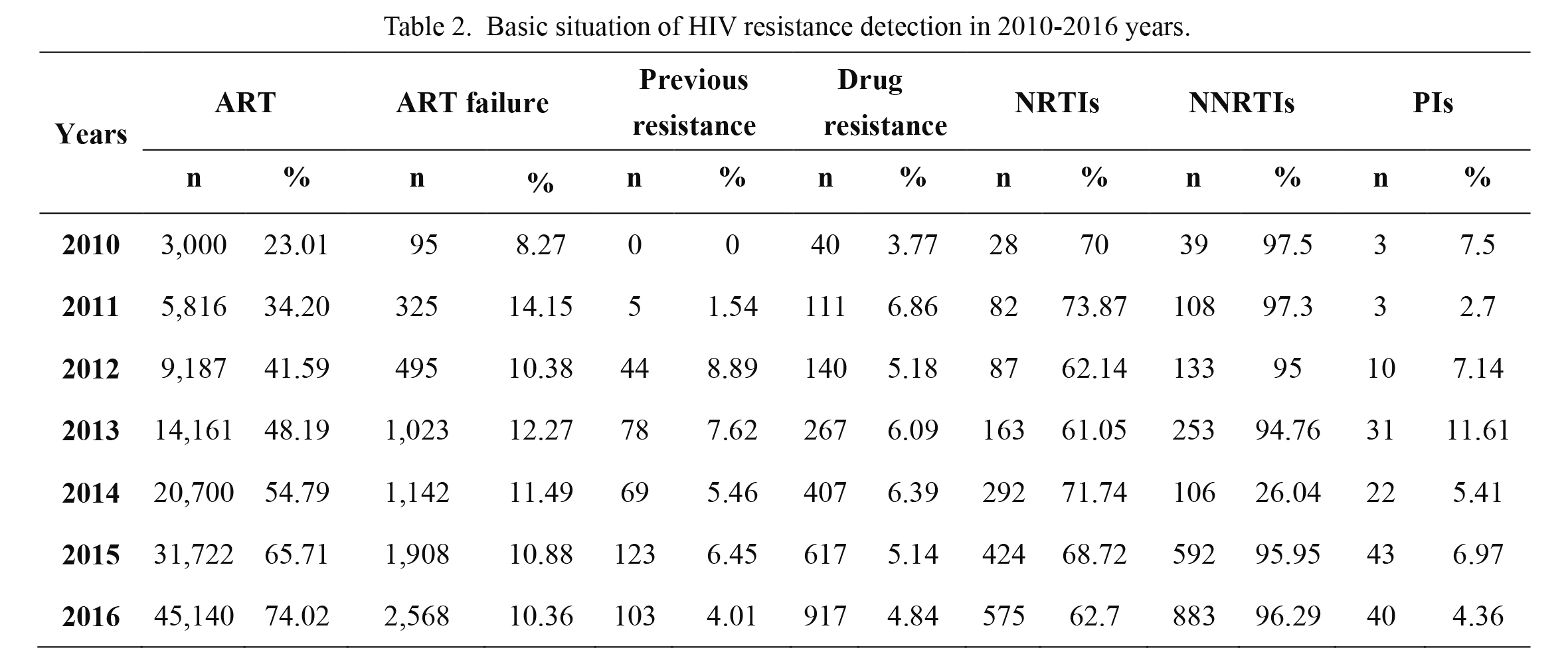
Among the 7,095 individuals with viral load were greater than 1,000 copies/mL (ART-failure), we obtained the complete sequences of both PR and RT in 5,512 individuals. The annual drug resistance rates were 3.77%, 6.86%, 5.18%, 6.09%, 6.39%, 5.14% and 4.84%, respectively (Table 2), and there were 2,499 cases of different degrees of drug resistance from 2010 to 2016. According to the WHO list of mutations, most patients had a strain with one or more resistant mutations. Among those with HIVDR mutations identified, 634 (25.37%) in non-nucleoside reverse transcriptase inhibitors in treatment-experienced (NNRTIs), 40 (1.60%) individuals were against nucleoside reverse transcriptase inhibitors (NRTIs), and 36 (1.44%) were against protease inhibitors (PIs), including 1,781 (71.27%) against both NRTIs and NNRTIs (Table 2).
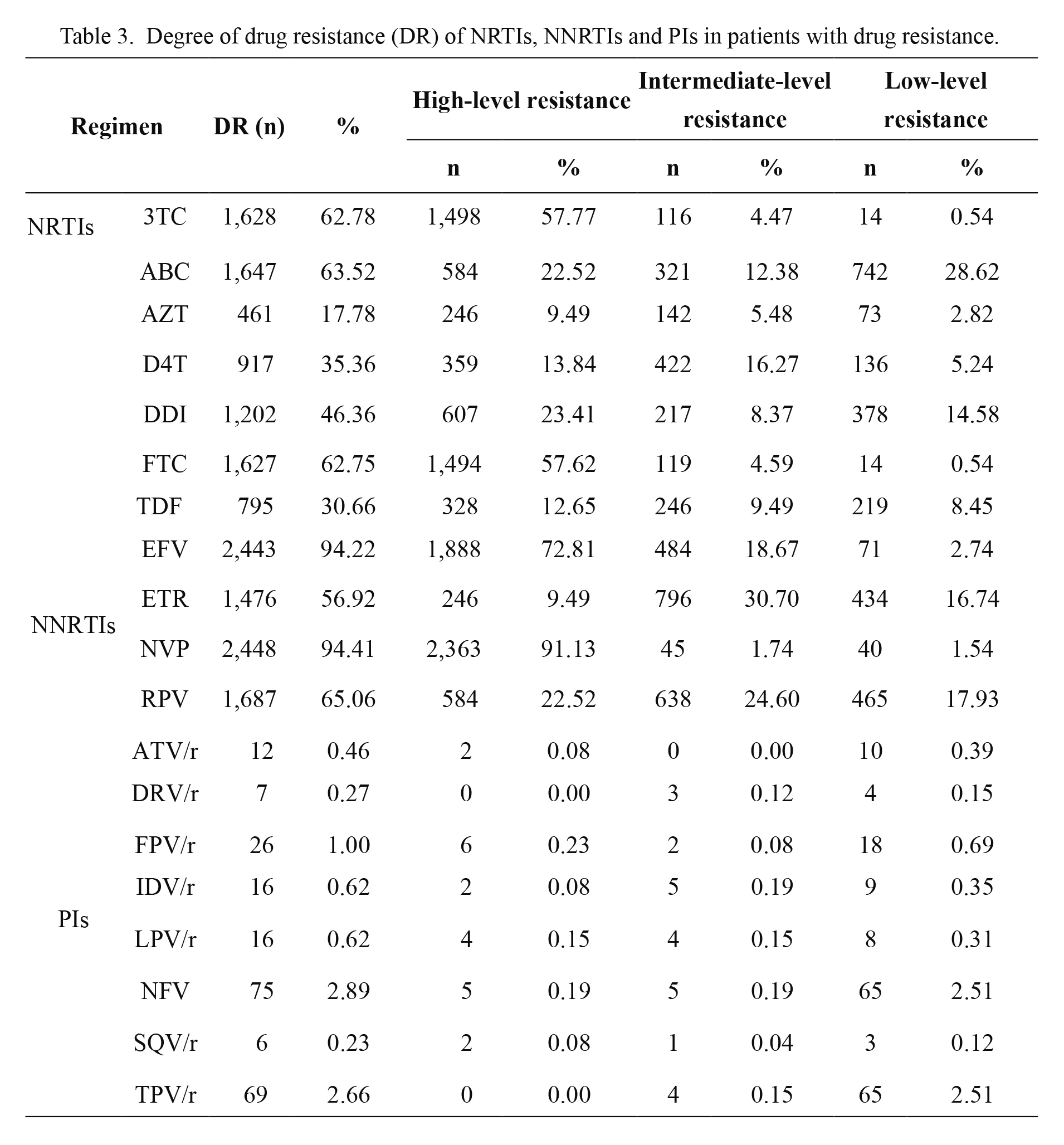
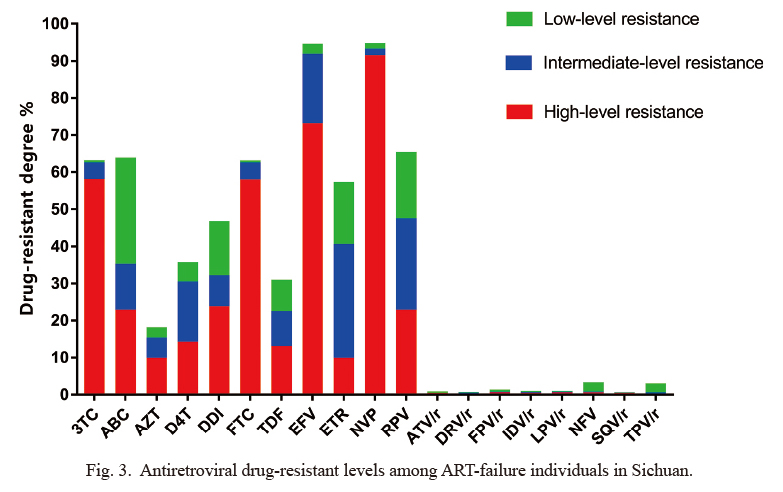
Among the genetic mutations of newly resistant patients from 2010 to 2016, the proportion of those showed the highest resistant to NRTIs and also the NNRTIs. High-level resistant drugs of NRTIs were mainly lamivudine (3TC) (57.77%) and emtricitabine (FTC) (57.62%) (Table 3, Fig. 3), although of NNRTIs was mainly nevirapine (NVP) (91.13%) and efavirenz (EFV) (72.81%). The proportion of protease inhibitor resistance remains low in general. There was high resistant to fosamprenavir with ritonavir (FPV/r) (0.23%), lopinavir with ritonavir (LPV/r) (0.15%) and nelfinavir (NFV) (0.19%) in 6, 4 and 5 cases respectively, and low resistant to FPV/r (0.69%), nelfinavir (NFV) (2.51%) and tipranavir with ritonavir (TPV/r) (2.51%) in 18 and 65 (Table 3, Fig. 3).
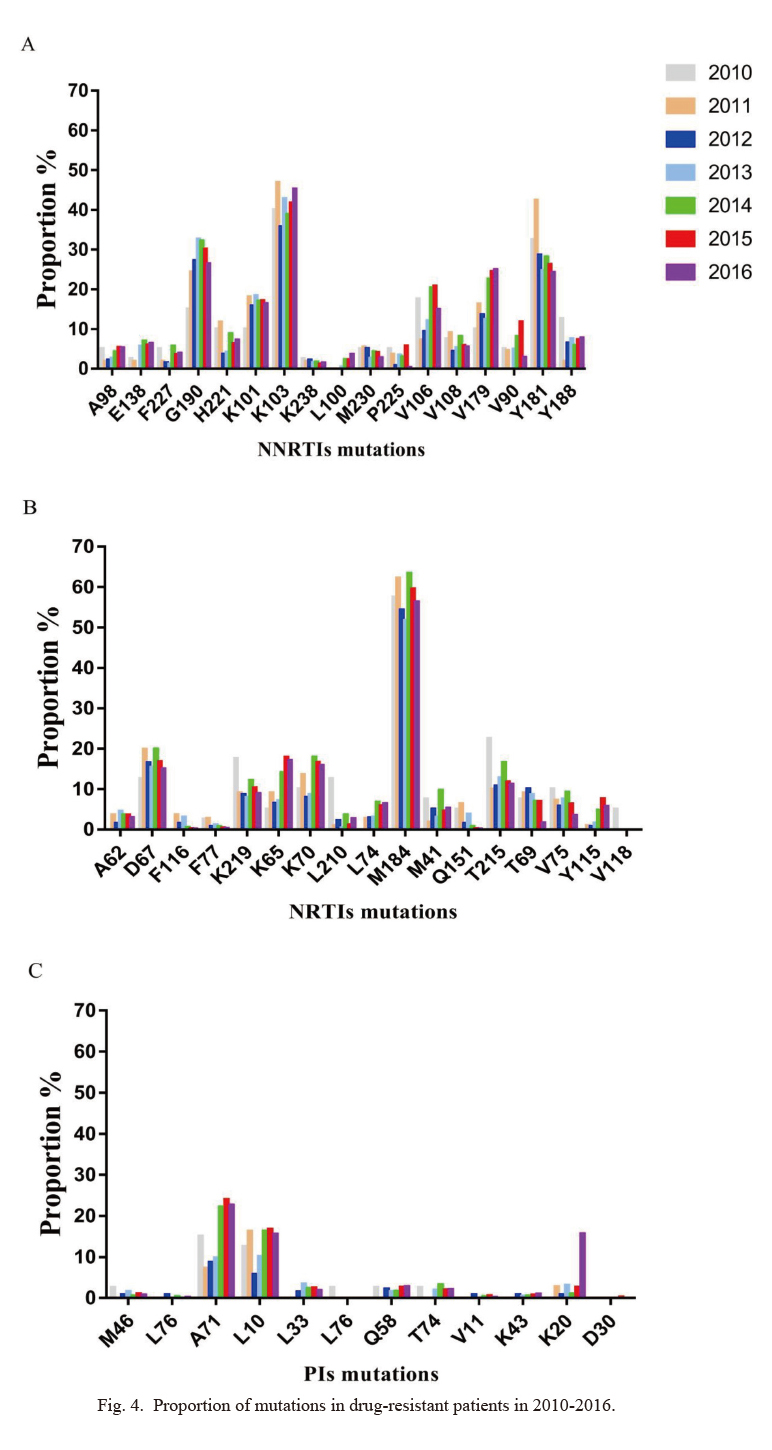
The most common NNRTIs mutation was K103 (42.42%), followed by G190 (28.65%), Y181 (26.53%) and V179 (21.87%) (Fig. 4A). The most common NRTIs mutation was M184 (the amino acid at position 184 of the nucleoside is mutated from M to another amino acid) (57.93%), followed by D67 (16.51%), K65 (14.58%) and K70 (14.96%) (Fig. 4B). By contrast, the mutation rate of main mutation sites of PIs was low (Fig. 4C). Between the main drug resistant sites, 20 cases (0.77%) showed M46 mutation, 3 cases (0.12%) showed L76 mutation, and the most common minor site mutations of PIs were A71 (19.94%) and L10 (14.81%).
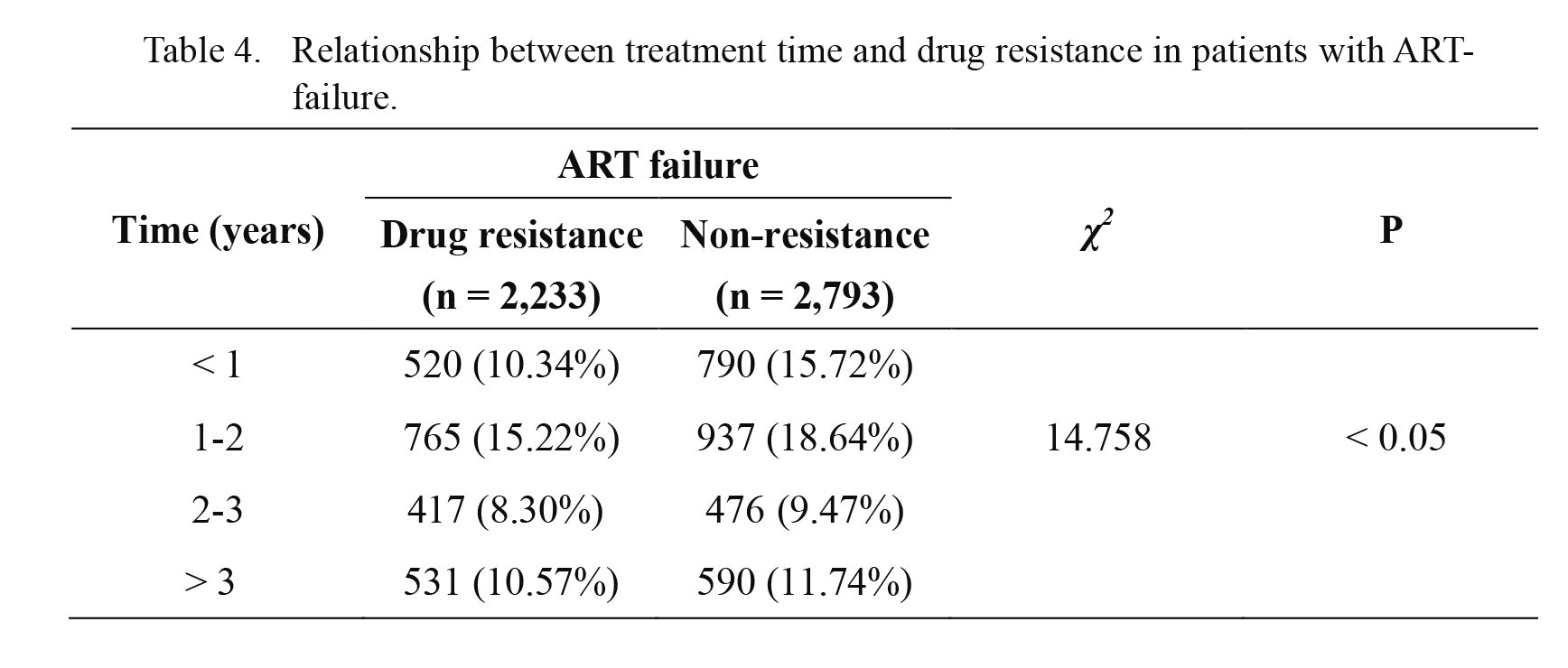
In the same period of time, it was also designated 5,026 HIV/AIDS patients with definite treatment time who failed antiviral therapy. It was observed that there was a correlation between the treatment time and ART-failure patients and it was linear, which indicates the drug resistant rate was raised with the prolongation of treatment time, and the difference was statistically significant (χ2 = 14.758, P < 0.05) (Table 4).
HIV-1 subtypes and mutations
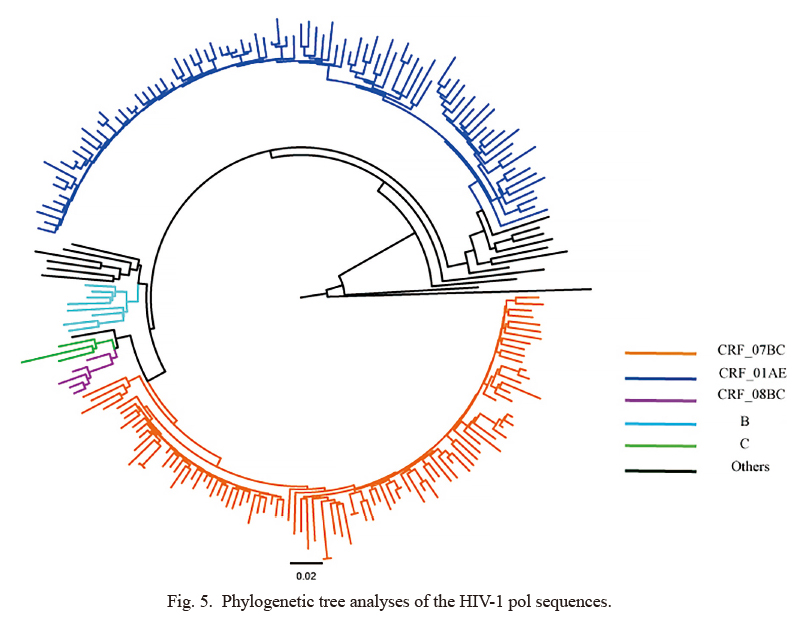
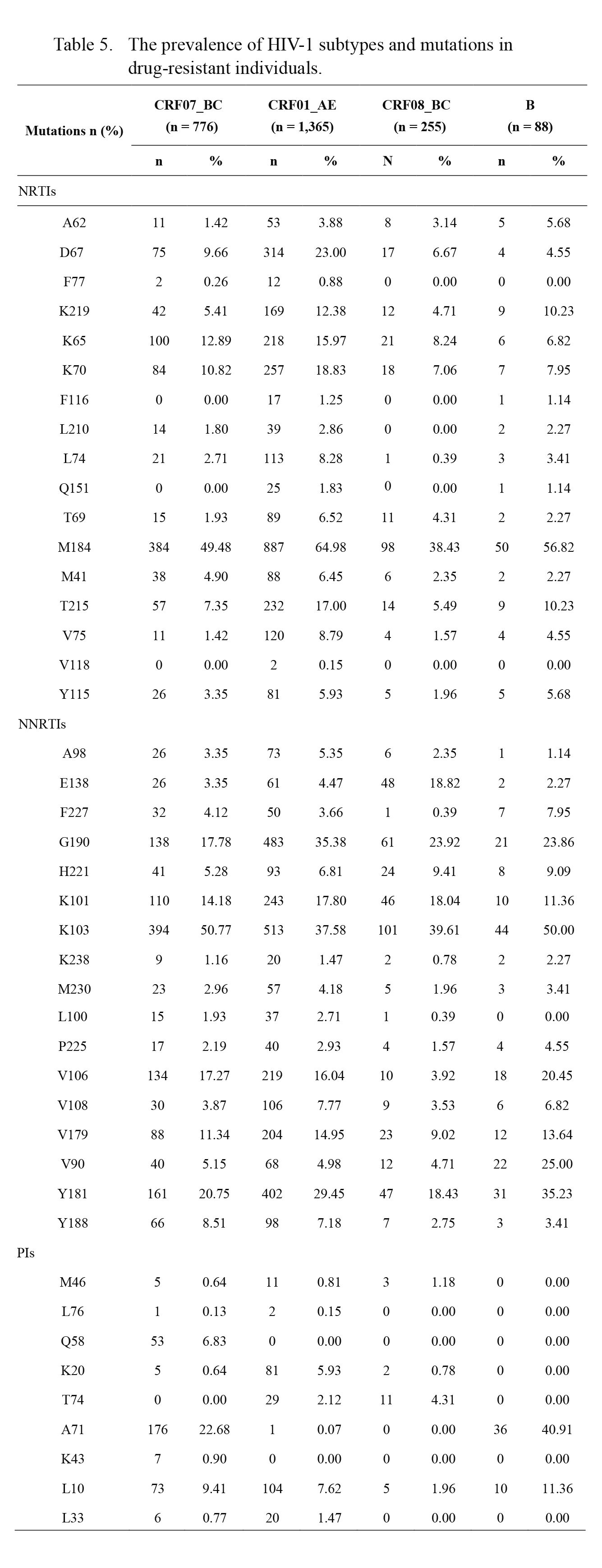
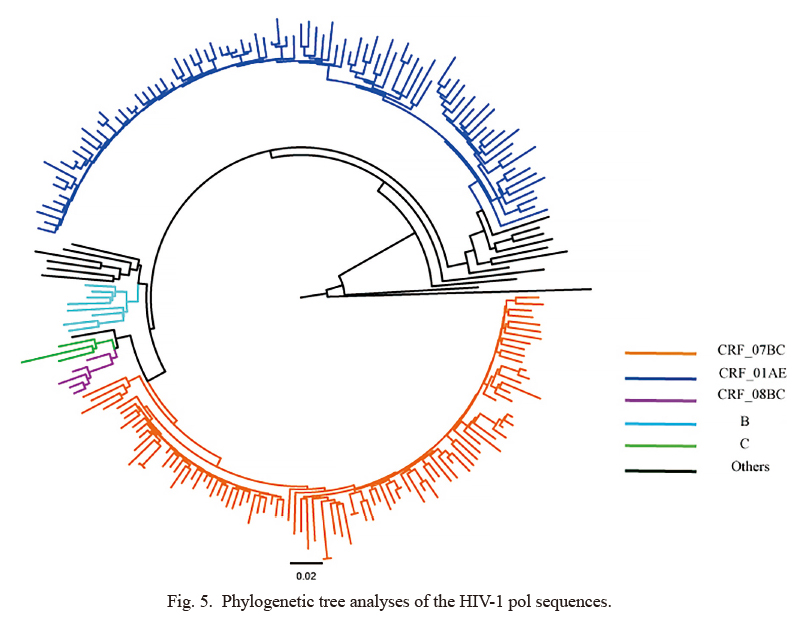
From the results of successful sequencing samples, it was found that CRF07_BC (41.42%) and CRF01_AE (40.77%) recombinant subtypes were the most common subtypes, followed by CRF08_BC (12.10%), B (2.81%) and C (1.32%). In addition, 2 cases of non-Sichuan province-specific subtype CRF02_AG (0.03%) and 89 cases (1.55%) of unknown subtypes were found (Fig. 5). It was also found that the drug-resistant proportion of CRF07_BC, CRF08_BC, CRF01_AE, B, C, CRF2_AG and unknown subtype strains were 32.66%, 37.72%, 58.01%, 54.65%, 38.16%, 50% and 64.04%, respectively. Comparison of the drug resistant rates of relatively large numbers of CRF07_BC, CRF08_BC, CRF01_AE and subtype B strains showed a statistically significant difference (χ2 = 327.865, P < 0.05), suggesting that the possibility of drug resistance of CRF01_AE subtype strains in ART-failure patients with failed virus inhibition was higher. The CRF07_BC, CRF08_BC, CRF01_AE and subtype B strains showed no significant change in the trend of drug resistant rate over the past seven years, and the possible reason may be that the resistant rate of each subtype was stable and the sample size was insufficient. However, there were some differences in the major mutation sites in each subtype of drug-resistant patients. The main mutation sites in patients resistant to CRF07_BC subtype were: K103 (50.77%), M184 (49.48%), A71 (22.68%), and Y181 (20.75%); in patients resistant to CRF01_AE subtype were: M184 (64.98%), K103 (37.58%), G190 (35.38%), Y181 (29.45%) and D67 (23%); in patients resistant to CRF08_BC subtype were: K103 (39.61%), M184 (38.43%) and G190 (23.92%); and in patients resistant to subtype B were: M184 (56.82%), K103 (50%), A71 (40.91%), Y181 (35.23%), V90 (25%), G190 (23.86%) and V106 (20.45%) (Table 5). Some drug-resistant mutation sites had significant differences among different subtypes.
Discussion
The epidemic situation in Sichuan Province showed a low overall prevalence of HIV/AIDS; however, the prevalence was higher in some areas, such as Liangshan Prefecture and Chengdu city, where the epidemic situation was more serious, accounting for more than half in Sichuan. By HIV resistance surveillance, we found that the main routes of transmission of AIDS in Sichuan Province were sexual transmission and injection drug users. In contrast, the rate of heterosexual transmission has significantly increased, whereas the spread of injecting drug use was on the contrary. The epidemic spread from high-risk groups to the general population, and the proportion of the older population that is aged 50 years and over has increased. It is suggested that propaganda and education on HIV/AIDS interventions for the general population should be strengthened, especially for the elderly whose number of patients increased rapidly. Meanwhile, we also found the prevalence of acquired drug resistance during a relatively long period (from 2010 to 2016) in rapid scale-up of ART program in Sichuan. By the end of 2016, the total number of people living with HIV and patients in Sichuan was 92,976; it was the first ranking in China. In recent years, the number of people receiving ART has increased each year. The findings revealed that the increasing rate of ART coverage in our province from 23.01% in 2010 to 74.02% in 2016, but there was a still large gap to achieving the 90% target of the infected people receiving ART.
HIVDR is one of the major problems with ART program, as affecting the clinical outcomes of ART, especially in countries with limited access to ART. Our results indicated that the overall incidence of acquired drug resistance was 5.47% similar to discussed earlier in Sichuan, and drug resistance rate reach the threshold in low-incidence according to the definition of WHO (5%) in 2011 (6.86%), 2012 (5.18%), 2013 (6.09%), 2014 (6.39%) and 2015 (5.14%) (Jordan et al. 2012). There are two types of internationally recognized initial treatment options of NRTIs plus one NNRTI or one PI which has added ritonavir (RTV). Numerous studies have shown that the most common cause of ART failure was drug resistance mutation (Hirsch et al. 1998; Durant et al. 1999; Vandamme et al. 1999; Clevenbergh et al. 2000). In this study, we found that the majority of the drug-resistant patients were resistant to NRTIs and NNRTIs were basically the same by the surveillance and emerging data sources of HIV resistance in China (Xing et al. 2013). Amongst the drug-resistant patients, 3TC and FTC were the most important NRTIs drugs responsible for high resistance, and NVP and EFV were the main NNRTI drugs producing high level of resistance.
The ART program in Sichuan province consisted of two nucleosides and one non-nucleoside reverse transcriptase inhibitor, the main therapy was AZT+3TC+NVP/EFV or D4T+3TC+NVP/EFV, which account for more than 80% of entirely antiviral treatment, resulting in NNRTIs and NRTIs-based drug-resistant mutations throughout the course of treatment. The mutation rate of M184 site was 57.93% in the new drug-resistant patients from 2010 to 2016, which represents the highest frequency of drug resistance in NRTIs. M184 was also considered as a major mutation site responsible for drug resistance to 3TC, and it can also lead to high resistance to FTC and low resistance to ABC (Kulkarni et al. 2012). The use of NNRTIs caused mutations in K103 (42.42%), G190 (28.65%) and Y181 (26.53%), respectively, which is consistent with NNRTIs resistant mutations in Yunnan Province (Chen et al. 2014).
Based on the above analysis, the main mutation sites of drug-resistant patients in Sichuan province were M184, Y181, K103, G190 and V179. Although some single sites do not cause DR, their accumulation may increase the adaptability of drug-resistant strains and increase their replication level. Later ART would accelerate the emergence of other drug-resistant mutations and increase the level of drug resistance (Johnson et al. 2003; van Maarseveen et al. 2006). There were some patients increasing resistant to the unused drugs, such as FTC, ETR, FPV/r, IDV/r, NFV, and TPV/r, which may be interrelated to the use of similar drugs causing cross resistance; therefore, the sensitivity of strain to another drugs of the similar type was also reduced. Meanwhile PIs are second-line drugs, there are relatively fewer patients using second-line regimen in Sichuan, and the incidence of PIs drug resistance was also lower. Though the number of drug-resistant patients has been increased, the patients are switching to second-line regimen.
It is noteworthy among the dataset of successful sequencing samples, CRF07_BC and CRF01_AE were the main subtypes of HIV-1 epidemic strains in patients with failed antiviral therapy, followed by CRF08_BC, B, and C. The main epidemic subtypes in Sichuan were different from the single B and C subtypes in 2010 (Shao et al. 1999; Yuan et al. 2015), which may relate to the genetic polymorphism of HIV epidemic strains and the variations of main transmission routes. As compared with other provinces, the main endemic subtype of drug-resistant strains was CRF01_AE in Fujian and Guangdong (Deng et al. 2014; Chen et al. 2018; Lan et al. 2018), subtype B in Liaoning province, and subtype C and subtype B in Dehong prefecture, Yunnan province (Duan et al. 2017). The main HIV-1 subtypes of patients with ART-failure in some areas of Sichuan province were different. For example, in Dazhou City of Sichuan patients with ART-failure in 2013, this was mainly caused by CRF01_AE, which was mostly spread by the intravenous drug abuse and heterosexual route of transmission. However, in the study of drug resistance in Butuo County of Liangshan Prefecture in 2013, 23 of the 24 were successful sequencing samples CRF07_BC (95.83%) for subtype. Though the number of samples was smallest, the conclusion was consistent with the molecular epidemiological survey of Liangshan Prefecture in 2009 (Li et al. 2015). The most of infected people in Butuo County were the Yi people, and most of them were farmers, whose education level was low.
This study showed that the frequency of drug resistance was higher in HIV-1 CRF01_AE subtypes, and the mutation sites were diverse in different subtypes of drug-resistant patients. It has been reported that the mutation A71V is present only in subtype B (Ariyoshi et al. 2003). Among the drug-resistant mutations against PIs, A71 was detected in 176 cases (22.68%) of CRF07_BC subtype, which was statistically different from CRF01_AE and CRF08_BC, and detected in 36 cases (40.91%) of B subtypes, which was statistically different from CRF01_AE and CRF08_BC too. It can be considered that the proportion of A71 mutations in CRF07_BC and B subtypes is higher than that of CRF01_AE and CRF08_BC subtypes. CRF07_BC is a recombinant form of subtype B, and the protease region in the pol gene region is derived from subtype B and some of these resistant characteristics have common as subtype B, thus inferring that A71 mutation is also present in CRF07_BC. Among the drug-resistant mutations against NRTIs, M184 was the highest mutation frequency in different subtypes, and M184 was the main mutation leading to drug resistance to 3TC, which can interfere with triphosphorylation of lamivudine into the accurate position of catalytic site, resulting in highly resistant to 3TC. There were 424 cases of M184 alone in this study, which showed high resistance to 3TC, low resistance to ABC, and sensitivity to AZT and D4T. The M184 was together with 2-5 adenosine resistant mutations. F116 and Q151 were not detected in CRF07_BC and CRF08_BC. K65 and K70 showed higher mutation ratios in CRF01_AE belonging to different three subtypes.
Among the drug-resistant mutations against NNRTI, K103 had the highest mutation frequency in different subtypes. It has been shown that K103N was the most common and important mutation in patients treated with NNRTI, which caused 20-50 times resistance to all NNRTIs (Condra et al. 1995; Kozal et al. 1996). The earliest drug-resistant mutation in EFV was K103, but Y188 can also be seen. G190 had a higher proportion of mutations in CRF01_AE than other subtypes. Therefore, sites with significant different between subtypes and causing low resistance cannot be ignored, and their resistant sites were not only affected by drug selection pressure, but also related to strain subtypes.
In conclusion, we found that the prevalence of acquired drug resistance in Sichuan province was low during rapid scale-up of ART from 2010 to 2016 and rapid development of NNRTIs resistance among patients. It would be much better to determine PI-based treatment regimen that might benefit patients more than NNRTIs. Although our results highlight the importance of ADR surveillance over a long period, an in-depth study on the mutation of HIV-1 genotype is suggested.
Acknowledgments
This work was financially supported by the National Natural Science Foundations of China (81502801 and 81473020) and National Mega Projects of Science and Technology in 13th Five-Year Plan of China: Technical Platform for Communicable Disease Surveillance Project (No. 2017ZX10103010-002).
The authors are thankful to Public Health and Preventive Medicine Provincial Experiment Teaching Center, Sichuan University, Food Safety Monitoring and Risk Assessment Key Laboratory of Sichuan Province and Sichuan Provincial Center for Disease Control and Prevention for providing support and cooperation.
Author Contributions
Dan Yuan and Ke Dong designed and conducted the data collection, planned the data analysis, and conceptualized and drafted the paper; Xiaofang Pei contributed to the discussion and provided edits to the paper; Shu Liang contributed to the discussion and provided edits to the paper; Saira Baloch contributed to the discussion and provided edits to the paper and Li Ye, Yun Leng, Liao Feng, Hong Yang, Ling Su, Yiping Li, Fangting He, Dan Yuan and Ke Dong conducted the statistical analysis, wrote the statistical analysis section, and provided edits to the paper.
Conflict of Interest
The authors declare no conflict of interest.
References
-
Ariyoshi,
K.,
Matsuda,
M.,
Miura,
H.,
Tateishi,
S.,
Yamada,
K. &
Sugiura,
W.
(2003) Patterns of point mutations associated with antiretroviral drug treatment failure in CRF01_AE (subtype E) infection differ from subtype B infection. J. Acquir. Immune Defic. Syndr., 33, 336-342.
-
Bennett,
D.E.,
Bertagnolio,
S.,
Sutherland,
D. &
Gilks,
C.F.
(2008) The World Health Organization’s global strategy for prevention and assessment of HIV drug resistance. Antivir. Ther., 13 Suppl 2, 1-13.
-
Chen,
M.,
Wang,
J.,
Xing,
H.,
Ma,
Y.,
Yao,
S.,
Chen,
H.,
Yang,
J.,
Li,
Y.,
Duan,
S. &
Jia,
M.
(2014) Study on HIV-1 related genetics and threshold on drug resistance in Dehong prefecture of Yunnan province in 2012. Zhonghua Liu Xing Bing Xue Za Zhi, 35, 909-912.
-
Chen,
Z.W.,
Liu,
L.,
Chen,
G.,
Cheung,
K.W.,
Du,
Y.,
Yao,
X.,
Lu,
Y.,
Chen,
L.,
Lin,
X. &
Chen,
Z.
(2018) Surging HIV-1 CRF07_BC epidemic among recently infected men who have sex with men in Fujian, China. J. Med. Virol., 90, 1210-1221.
-
Clevenbergh,
P.,
Durant,
J.,
Halfon,
P.,
del Giudice,
P.,
Mondain,
V.,
Montagne,
N.,
Schapiro,
J.M.,
Boucher,
C.A. &
Dellamonica,
P.
(2000) Persisting long-term benefit of genotype-guided treatment for HIV-infected patients failing HAART. The Viradapt Study: week 48 follow-up. Antivir. Ther., 5, 65-70.
-
Condra,
J.H.,
Schleif,
W.A.,
Blahy,
O.M.,
Gabryelski,
L.J.,
Graham,
D.J.,
Quintero,
J.C.,
Rhodes,
A.,
Robbins,
H.L.,
Roth,
E.,
Shivaprakash,
M.,
Titus,
D.,
Yang,
T.,
Tepplert,
H.,
Squires,
K.E.,
Deutsch,
P.G, et al.
(1995) In vivo emergence of HIV-1 variants resistant to multiple protease inhibitors. Nature, 374, 569-571.
-
Deng,
Y.,
Zhang,
C.,
Yan,
Y.,
Yan,
P. &
Wu,
S.
(2014) Genetic subtype and epidemiological feature of HIV-1 circulating strains among recently infected patients in Fujian province. Zhonghua Liu Xing Bing Xue Za Zhi, 35, 714-719.
-
Duan,
X.,
Wang,
K.R.,
Wang,
J.B.,
Yang,
T.,
Wang,
Y.K.,
Yang,
J.,
Ye,
R.H.,
Yang,
Y.C.,
Yao,
S.T.,
Duan,
S. &
He,
N.
(2017) HIV subtype in newly reported HIV infected cases in Dehong prefecture of Yunnan province, 2015. Zhonghua Liu Xing Bing Xue Za Zhi, 38, 1107-1112.
-
Durant,
J.,
Clevenbergh,
P.,
Halfon,
P.,
Delgiudice,
P.,
Porsin,
S.,
Simonet,
P.,
Montagne,
N.,
Boucher,
C.A.,
Schapiro,
J.M. &
Dellamonica,
P.
(1999) Drug-resistance genotyping in HIV-1 therapy: the VIRADAPT randomised controlled trial. Lancet, 353, 2195-2199.
-
GBD 2015 HIV Collaborators
(2016) Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980-2015: the Global Burden of Disease Study 2015. Lancet HIV, 3, e361-e387.
-
Hallack,
R.,
Doherty,
L.E.,
Wethers,
J.A. &
Parker,
M.M.
(2008) Evaluation of dried blood spot specimens for HIV-1 drug-resistance testing using the Trugene HIV-1 genotyping assay. J. Clin. Virol., 41, 283-287.
-
Hecht,
F.M.,
Wang,
L.,
Collier,
A.,
Little,
S.,
Markowitz,
M.,
Margolick,
J.,
Kilby,
J.M.,
Daar,
E.,
Conway,
B. &
Holte,
S.;
AIEDRP Network
(2006) A multicenter observational study of the potential benefits of initiating combination antiretroviral therapy during acute HIV infection. J. Infect. Dis., 194, 725-733.
-
Hirsch,
M.S.,
Conway,
B.,
D’Aquila,
R.T.,
Johnson,
V.A.,
Brun-Vezinet,
F.,
Clotet,
B.,
Demeter,
L.M.,
Hammer,
S.M.,
Jacobsen,
D.M.,
Kuritzkes,
D.R.,
Loveday,
C.,
Mellors,
J.W.,
Vella,
S. &
Richman,
D.D.
(1998) Antiretroviral drug resistance testing in adults with HIV infection: implications for clinical management. International AIDS Society-USA Panel. JAMA, 279, 1984-1991.
-
Hirsch,
M.S.,
Gunthard,
H.F.,
Schapiro,
J.M.,
Brun-Vezinet,
F.,
Clotet,
B.,
Hammer,
S.M.,
Johnson,
V.A.,
Kuritzkes,
D.R.,
Mellors,
J.W.,
Pillay,
D.,
Yeni,
P.G.,
Jacobsen,
D.M. &
Richman,
D.D.
(2008) Antiretroviral drug resistance testing in adult HIV-1 infection: 2008 recommendations of an International AIDS Society-USA panel. Clin. Infect. Dis., 47, 266-285.
-
Johnson,
V.A.,
Brun-Vezinet,
F.,
Clotet,
B.,
Conway,
B.,
D’Aquila,
R.T.,
Demeter,
L.M.,
Kuritzkes,
D.R.,
Pillay,
D.,
Schapiro,
J.M.,
Telenti,
A. &
Richman,
D.D. ;
International AIDS Society-USA Drug Resistance Mutation Group
(2003) Drug resistance mutations in HIV-1. Top. HIV Med., 11, 215-221.
-
Jordan,
M.R.,
Bennett,
D.E.,
Wainberg,
M.A.,
Havlir,
D.,
Hammer,
S.,
Yang,
C.,
Morris,
L.,
Peeters,
M.,
Wensing,
A.M.,
Parkin,
N.,
Nachega,
J.B.,
Phillips,
A.,
De Luca,
A.,
Geng,
E.,
Calmy,
A.,
et al. (2012) Update on World Health Organization HIV drug resistance prevention and assessment strategy: 2004-2011. Clin. Infect. Dis., 54 Suppl 4, S245-249.
-
Kozal,
M.J.,
Shah,
N.,
Shen,
N.,
Yang,
R.,
Fucini,
R.,
Merigan,
T.C.,
Richman,
D.D.,
Morris,
D.,
Hubbell,
E.,
Chee,
M. &
Gingeras,
T.R.
(1996) Extensive polymorphisms observed in HIV-1 clade B protease gene using high-density oligonucleotide arrays. Nat. Med., 2, 753-759.
-
Kulkarni,
R.,
Babaoglu,
K.,
Lansdon,
E.B.,
Rimsky,
L.,
Van Eygen,
V.,
Picchio,
G.,
Svarovskaia,
E.,
Miller,
M.D. &
White,
K.L.
(2012) The HIV-1 reverse transcriptase M184I mutation enhances the E138K-associated resistance to rilpivirine and decreases viral fitness. J. Acquir. Immune Defic. Syndr., 59, 47-54.
-
Lan,
Y.,
Zhu,
W.,
Hu,
F.,
Tang,
S.,
Li,
L.,
Cai,
X.,
Tang,
X. &
Cai,
W.
(2018) Genetic characterization of a novel HIV-1 CRF01_AE/CRF07_BC recombinant form among men who have sex with men in Guangdong, China. Arch. Virol., 163, 3093-3097.
-
Li,
L.,
Wei,
D.,
Hsu,
W.L.,
Li,
T.,
Gui,
T.,
Wood,
C.,
Liu,
Y.,
Li,
H.,
Bao,
Z.,
Liu,
S.,
Wang,
X. &
Li,
J.
(2015) CRF07_BC strain dominates the HIV-1 epidemic in injection drug users in Liangshan Prefecture of Sichuan, China. AIDS Res. Hum. Retroviruses, 31, 479-487.
-
Li,
X.P.,
Xing,
H.,
Wang,
Z.,
Si,
X.F.,
Wang,
L.E.,
Cheng,
H.,
Cui,
W.G.,
Jiang,
S.L.,
Liao,
L.J.,
Zhou,
H.W.,
Huang,
J.H.,
Peng,
H.,
Ma,
P.F. &
Shao,
Y.M.
(2007) Study of HIV-1 drug resistance in patients receiving free antiretroviral therapy in China. Virol. Sin., 22, 233-240.
-
Liao,
L.,
Xing,
H.,
Li,
X.,
Ruan,
Y.,
Zhang,
Y.,
Qin,
G. &
Shao,
Y.
(2007) Genotypic analysis of the protease and reverse transcriptase of HIV type 1 isolates from recently infected injecting drug users in western China. AIDS Res. Hum. Retroviruses, 23, 1062-1065.
-
Manasa,
J.,
Lessells,
R.J.,
Skingsley,
A.,
Naidu,
K.K.,
Newell,
M.L.,
McGrath,
N. &
de Oliveira,
T.;
Southern African Treatment and Resistance Network
(2013) High-levels of acquired drug resistance in adult patients failing first-line antiretroviral therapy in a rural HIV treatment programme in KwaZulu-Natal, South Africa. PLoS One, 8, e72152.
-
National Bureau of Statistics of China
(2011) Communiqué of the National Bureau of Statistics of People’s Republic of China on Major Figures of the 2010 Population Census [1] (No. 1) http://www.stats.gov.cn/english/NewsEvents/201104/t20110428_26449.html [Accessed: April 28, 2011].
-
Shao,
Y.,
Zhao,
F. &
Yang,
W.
(1999) The identification of recombinant HIV-1 strains in IDUs in southwest and northwest China. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi, 13, 109-112.
-
Su,
L.,
Zhou,
X.,
Yuan,
D.,
Yang,
H.,
Wei,
D.,
Qin,
G. &
Liang,
S.
(2014) Prevalence and patterns of drug-resistance mutations among HIV-1 patients infected with CRF07_BC strains in Sichuan province, China. Virol. Sin., 29, 237-241.
-
The Chinese Center for AIDS Prevention and Control (NCAIDS); The Chinese Center for Sexually Transmitted Disease Prevention and Control (NCSTD); The Chinese Center for Disease Prevention and Control (China CDC)
(2016) Update on the AIDS/STD epidemic in China and main response in control and prevention in February, 2016. Chin. J. AIDS STD, 22, 585.
-
The Chinese Center for AIDS Prevention and Control (NCAIDS); The Chinese Center for Sexually Transmitted Disease Prevention and Control (NCSTD); The Chinese Center for Disease Prevention and Control (China CDC)
(2018) Update on the AIDS/STD epidemic in China in May, 2018. Chin. J. AIDS STD, 24, 645.
-
van Maarseveen,
N.M.,
de Jong,
D.,
Boucher,
C.A. &
Nijhuis,
M.
(2006) An increase in viral replicative capacity drives the evolution of protease inhibitor-resistant human immunodeficiency virus type 1 in the absence of drugs. J. Acquir. Immune Defic. Syndr., 42, 162-168.
-
Vandamme,
A.M.,
Van Laethem,
K. &
De Clercq,
E.
(1999) Managing resistance to anti-HIV drugs: an important consideration for effective disease management. Drugs, 57, 337-361.
-
World Health Organization (WHO)
(2012) The HIV drug resistance report. World Health Organization, Geneva.
-
World Health Organization (WHO)
(2013) Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. World Health Organization, Geneva.
-
World Health Organization (WHO)
(2017) HIV Data and statistics. http://www.who.int/hiv/data/en/ [Accessed: June 06, 2018].
-
Xing,
H.,
Ruan,
Y.,
Li,
J.,
Shang,
H.,
Zhong,
P.,
Wang,
X.,
Liao,
L.,
Li,
H.,
Zhang,
M.,
Xue,
Y.,
Wang,
Z.,
Su,
B.,
Liu,
W.,
Dong,
Y.,
Ma,
Y.,
et al. (2013) HIV drug resistance and its impact on antiretroviral therapy in Chinese HIV-infected patients. PLoS One, 8, e54917.
-
Yuan,
D.,
Su,
L.,
Liu,
H.,
Yu,
H.,
Yang,
H.,
Ye,
L.,
Wei,
D.,
Pei,
X. &
Liang,
S.
(2015) Drug-resistance characteristics of CRF01_AE and CRF07_BC subtypes of HIV-1 strains in Sichuan province. Zhonghua Yu Fang Yi Xue Za Zhi, 49, 901-906.
-
Zhao,
D.C.,
Wen,
Y.,
Ma,
Y.,
Zhao,
Y.,
Zhang,
Y.,
Wu,
Y.S.,
Liu,
X.,
Au,
E.,
Liu,
Z.F. &
Zhang,
F.J.
(2012) Expansion of China’s free antiretroviral treatment program. Chin. Med. J. (Engl.), 125, 3514-3521.
-
Zhong,
P.,
Kang,
L.,
Pan,
Q.,
Konings,
F.,
Burda,
S.,
Ma,
L.,
Xue,
Y.,
Zheng,
X.,
Jin,
Z. &
Nyambi,
P.
(2003) Identification and distribution of HIV type 1 genetic diversity and protease inhibitor resistance-associated mutations in Shanghai, P. R. China. J. Acquir. Immune Defic. Syndr., 34, 91-101.