2019 年 247 巻 1 号 p. 41-49
2019 年 247 巻 1 号 p. 41-49
Esophageal achalasia is a disease characterized by the impaired esophageal peristalsis and non-relaxation of the lower esophageal sphincter muscle with unknown causes. Clinical manifestation of the disease is nonspecific (e.g., weight loss, vomiting, and persistent cough); namely, early diagnosis of the disease is often difficult. Delayed diagnosis of the disease is known to impair the patients’ quality of life. Identifying the diagnostic factors that could cause diagnostic delay is needed. In this study, we collected data from 38 patients with achalasia and searched for diagnostic factors associated with delayed diagnosis (i.e., ≥ 6 months from the first hospital visit to diagnosis). The enrolled patients, diagnosed with achalasia based on esophageal manometry findings, had undergone surgical myotomy. As a result, the diagnosis of achalasia was likely to be delayed when the physician who had first contacted the patient did not perform a barium swallow test (p < 0.0001) or chest CT scan (p < 0.01) in a timely fashion. Among the patients with a delayed diagnosis (n = 15), none underwent a barium swallow test or chest CT within 6 months from their first hospital visit. The estimated sensitivities of diagnostic examinations for achalasia based on the enrolled 38 patients were higher than 80% for the barium swallow test and chest CT scan, but only 50-81% for endoscopy. To avoid the delayed diagnosis of achalasia, performing a barium swallow test or chest CT scan in a timely fashion, in addition to routine endoscopy, appears to be highly important.
Esophageal achalasia is a disease involving disturbed relaxation of the sphincter muscle in the cardiac region of the esophagus (O’Neill et al. 2013). Based on the failure of relaxation in this region, many nonspecific symptoms mainly related to chest discomfort or eating disorders can occur (Boeckxstaens et al. 2014). Annual incidence of achalasia is thought to be about 1 in 100,000 individuals and its prevalence is thought to be about 10 in 100,000 (Francis and Katzka 2010; Vaezi et al. 2013). Sex or racial difference in the incidence rate of the disease has not been known. Because the chief complaints in achalasia are nonspecific (e.g., weight loss, vomiting, and persistent cough), this disease has many differential diagnoses, such as anorexia nervosa, gastroesophageal reflux disease, psychosomatic disease, and cardiovascular ischemic disease (Bennett 2001; Desseilles et al. 2006; Badillo and Francis 2014; Reas et al. 2014; Jeon et al. 2017). As a result, if not recognized in the early phase, the diagnosis of achalasia is often delayed (Gockel et al. 2012). A delayed diagnosis of achalasia has been known to impair quality of life significantly (Liu et al. 2015). Therefore, elucidating the diagnostic factors that could cause a delayed diagnosis of achalasia could be clinically important, especially in the primary care setting.
At present, the diagnosis of achalasia is performed empirically based on multiple examinations such as the barium swallow test, esophageal manometry, chest CT, and endoscopy (Pohl and Tutuian 2007; O’Neill et al. 2013). Among these examinations, esophageal manometry is believed to be the gold standard for the definitive diagnosis of achalasia, but routinely performing manometry in the primary care setting is not currently realistic (Moonen and Boeckxstaens 2014). In the actual primary care setting, endoscopy is the most popular initial approach, but other examinations are not performed frequently in the early phase. Such biased selection regarding diagnostic examinations for achalasia in the primary care setting could lead to a delayed diagnosis of achalasia in many patients.
Therefore, in the present study, we retrospectively collected data from patients with achalasia to estimate the sensitivity of each diagnostic examination (i.e., upper endoscopy, barium swallow test, chest CT, manometry). In addition, we investigated the timing of each diagnostic examination in the enrolled patients to elucidate the factors that could cause a delayed diagnosis.
Enrolled patients were those diagnosed with achalasia based on esophageal manometry findings who had undergone surgical myotomy at Tohoku University Hospital between October 2006 and June 2015. A total of 38 patients with achalasia met these criteria and were enrolled in the study.
Study variablesAmong the 38 enrolled patients with achalasia, the following variables were comprehensively collected: sex, onset age, body-mass index, chief complaint at onset, type of achalasia, history and timing of diagnostic examinations for achalasia (i.e., endoscopy, barium swallow test, chest CT scan), and time (months) from the first hospital visit to the definite diagnosis of achalasia.
Before the therapeutic intervention for achalasia, a barium swallow test was performed in 29 (76.3%) of the patients, endoscopy in 31 (81.6%), chest CT scan in 31 (81.6%), and esophageal manometry in all 38 (100.0%); however, the manometry data in one patient was missing and unavailable. Regarding esophageal manometry, lower esophageal sphincter (LES) pressure ≥ 10-15 mmHg was considered to be abnormal and suggestive of achalasia (Holloway et al. 1986; Richter and Boeckxstaens 2011; Moonen and Boeckxstaens 2014). Regarding the chest CT scans, an abnormally dilated lower esophagus with an internal air–fluid contrast level was considered to be the most important finding suggestive of achalasia (Rabushka et al. 1991); the sensitivity of chest CT scans for achalasia was estimated based on an interpretation report by radiologists. The established characteristic findings in the diagnostic examinations for achalasia are listed in Table 1. For reference, the characteristic findings in one patient with achalasia treated in our hospital are shown in Fig. 1. Based on these established characteristic findings in the 38 enrolled patients, the sensitivity of each diagnostic examination for achalasia was estimated retrospectively.

Characteristic findings for the diagnosis of achalasia.
Characteristic findings for the four popular diagnostic examinations for achalasia are listed in this table.
EGJ, esophagogastric junction; IRP, integrated relaxation pressure; LES, lower esophageal sphincter.

Characteristic findings of diagnostic examinations in a 69-year-old male patient with achalasia.
(A) Finding from upper gastrointestinal endoscopy showing a dilated esophagus with stagnated intraesophageal liquid. (B) Finding from the barium swallow test, showing “bird-beak narrowing” deformity. (C) Finding from non-contrast CT showing a markedly dilated esophagus with stagnated liquid (white arrow).
To identify the factors that could cause delayed diagnosis of achalasia, the 38 enrolled patients were divided into the following two groups based on the time from the first hospital visit to the definite diagnosis of achalasia: < 6 months (Non-delayed Group: n = 23) and ≥ 6 months (Delayed Group: n = 15). The history and timing of each diagnostic examination were then compared between the two groups to identify the factors that could cause a diagnostic delay.
Statistical analysisAll of the studied variables described in the previous section were compared between the Non-delayed Group and Delayed Group to elucidate the factors that could cause a delayed diagnosis of achalasia.
Comparisons of the numerical data with a normal distribution between the two groups were conducted using the Student’s t-test, while those of the frequencies were conducted using the chi-square or Fisher’s exact test. Because of the simultaneous comparisons, p-values < 0.01 were regarded to be statistically significant by applying Bonferroni’s correction.
All statistical analyses were conducted using SPSS Statistical Base 22 software (IBM, Armonk, NY, USA) and MATLAB R2015a (MathWorks, Natick, MA, USA).
Institutional review boardTohoku University Hospital Institutional Review Board approved all research protocols of this study (IRB No. 2017-1-222). All methods of this study were carried out in accordance with relevant guidelines and regulations. All enrolled patients gave informed consent prior to participation for this study about the possible enrollment for observational studies related to achalasia in the future.
The history of each diagnostic examination and the presence of characteristic abnormal findings in each examination suggestive of achalasia in the 38 enrolled patients are listed in Table 2.
The frequency of abnormal findings in each diagnostic examination for achalasia at the first attempt (i.e., excluding the second or third attempt) was as follows: 21/31 (67.7%) in endoscopy, 29/29 (100.0%) in the barium swallow test, 30/31 (96.8%) in the chest CT scan, and 37/37 (100.0%) in esophageal manometry.
As a result, the suggested 95% confidence interval of the sensitivity of each diagnostic examination for achalasia was as follows: 50.1-81.4% for endoscopy, 88.3-100.0% for the barium swallow test, 83.8-100.0% for the chest CT, and 90.6-100.0% for esophageal manometry (Julious 2005).
For reference, in the gastrointestinal endoscopy, resistance was felt by the examiner only in 40-60% of the studied achalasia patients, when the fiber passed through the esophago-gastric junction (EGJ). This fact suggests that the absence of resistance when the fiber pass EGJ would not be a reliable information for ruling out achalasia.
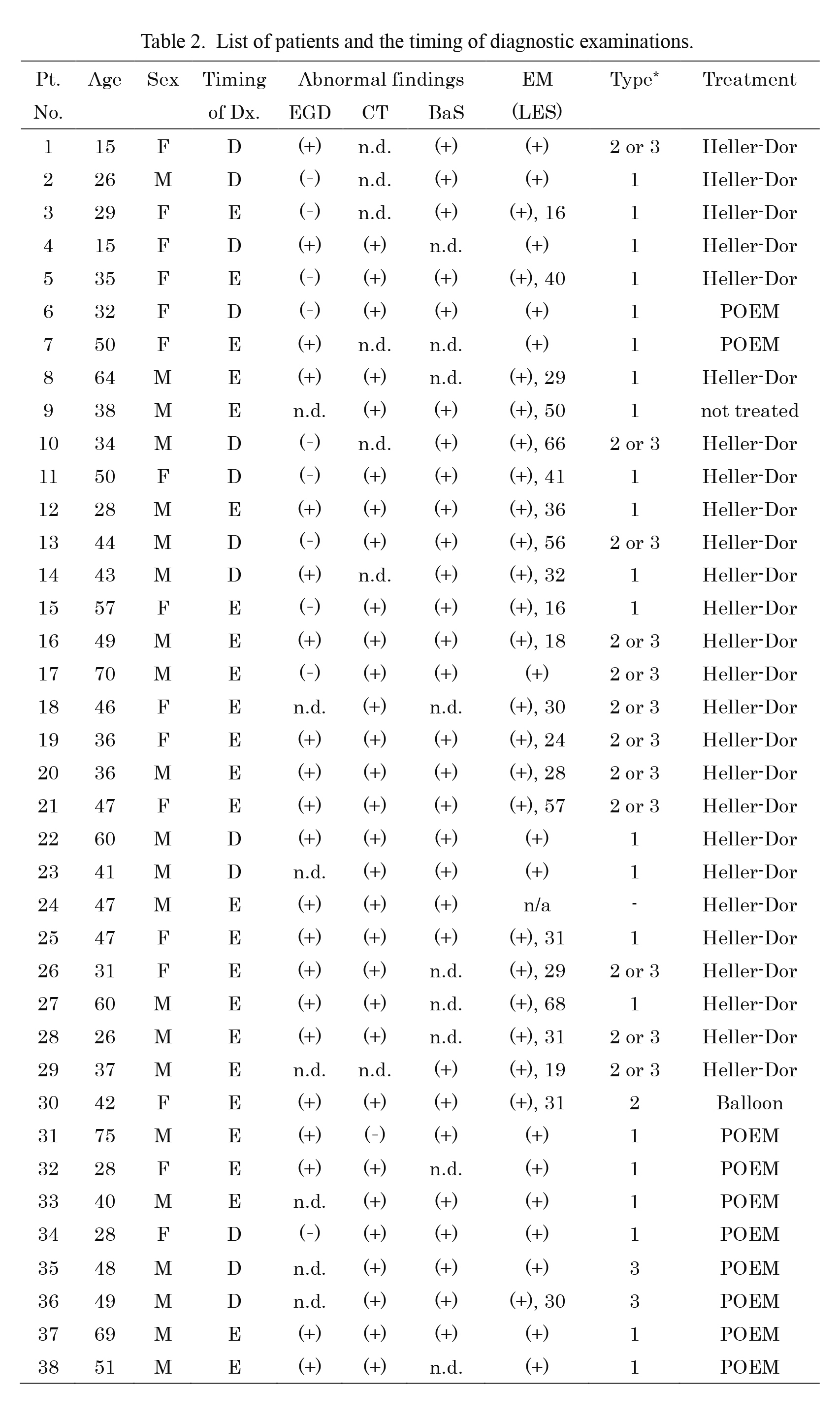
List of patients and the timing of diagnostic examinations.
Type-2 or type-3 achalasia, based on the latest Chicago classification, could not be determined in patients who did not undergo high-resolution manometry. Heller-Dor operation is a minimally-invasive laparoscopic myotomy of the lower esophageal sphincter muscle (Heller myotomy), followed by Dor fundoplication.
BaS, barium swallow test; D, delayed diagnosis; Dx., diagnosis; E, early (non-delayed) diagnosis; EGD, esophago-gastro-duodenoscopy; F, female; M, male; n/a, not available; n.d., not done before consultation at our hospital; POEM, peroral endoscopic myotomy; Pt, patient; (+), positive for abnormal findings in the examination; (−), negative for abnormal findings in the examination.
*Type of achalasia was determined based on the Chicago classification (version 3.0).
A histogram of the time from the first hospital visit for an episode resulting from achalasia to definite diagnosis of the disease is shown in Fig. 2. As shown in the figure, those patients who were not correctly diagnosed with achalasia within 6 months from the first hospital visit were not likely to receive a definite diagnosis for a long time.
For reference, among the 23 patients of the Non-delayed Group, 17 (73.9%) were correctly diagnosed with achalasia within 1 month from their first hospital visit. This asymmetrical bimodal distribution is part of the rationale to suspect that some unknown diagnostic factors could have caused the delayed diagnosis in the Delayed Group.

Histogram of the time from the first hospital visit to the diagnosis of achalasia.
Non-delayed Group consists of patients with achalasia whose time from the first hospital visit to the diagnosis of achalasia was < 6 months (n = 23). Delayed Group consists of patients whose time from the first hospital visit to diagnosis was ≥ 6 months (n = 15).
The results of the comparison of the background characteristics between the Non-delayed and Delayed Groups are summarized in Table 3. As shown in the table, no statistically significant differences were seen in any of the studied variables, including the esophageal shape (i.e. sigmoid or straight) or the clinical subtypes based on the distribution of esophageal pressurization.
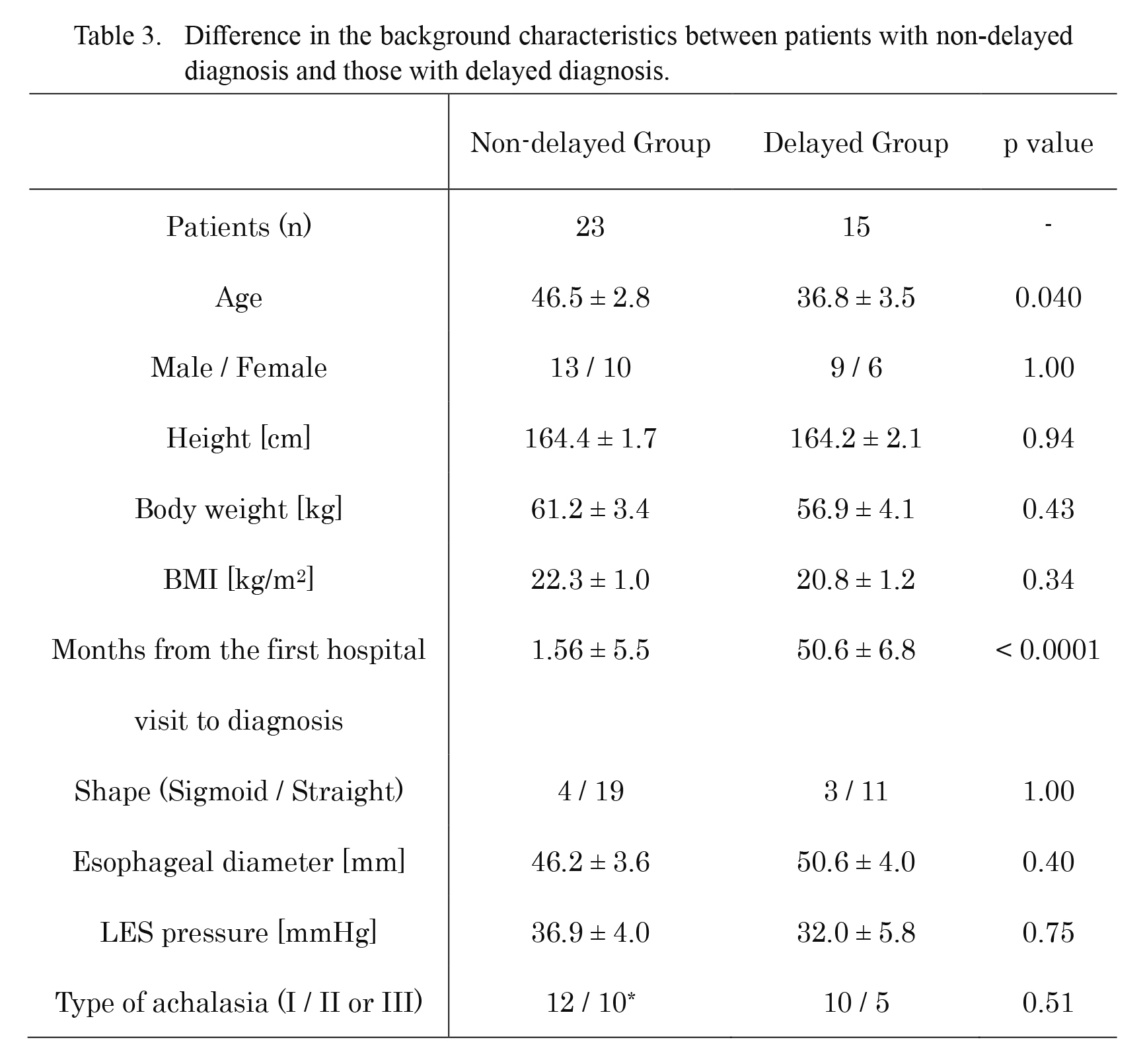
Difference in the background characteristics between patients with non-delayed diagnosis and those with delayed diagnosis.
Clinical information are listed and compared between the Non-delayed and Delayed Groups. Data are expressed as mean ± standard deviation. Because only p values < 0.01 were considered to be statistically significant, no significant differences in background characteristics were observed between the patients with non-delayed diagnosis and those with delayed diagnosis.
BMI, body mass index; LES, lower esophageal sphincter.
*The total number of patients for the type of achalasia in non-delayed group was 22, because one of the 23 patients was unable to be categorized into a specific classification.
The results of the comparison of clinical symptoms at disease onset, initial diagnosis at the first hospital visit, timing of diagnostic examinations, and the person who initially suspected the diagnosis of achalasia between Non-delayed and Delayed Groups are summarized in Table 4.
No differences in chief complaints were observed between the two groups. Earlier performance of the barium swallow test (p < 0.0001) and CT scan (p < 0.01) contributed to an earlier diagnosis. Whether physicians who first contacted the patients could have suspected achalasia significantly affected the subsequent speed of the diagnosis (p < 0.01).
The timings of the diagnostic examinations other than manometry and the presence of characteristic abnormal findings for achalasia in the 15 patients of the Delayed Group are listed in Table 5. No patients underwent chest CT or a barium swallow test within 6 months from the first hospital visit to diagnosis. The delayed performance of chest CT and a barium swallow test were identified as factors that led to a delayed diagnosis of achalasia.

Differences in the clinical manifestation and timing of diagnostic examinations between Non-delayed (n = 23) and Delayed (n = 15) Groups.
The frequencies of performing chest CT scans and of performing barium swallow tests within 6 months from the first hospital visit were significantly higher in Non-delayed Group than in Delayed Group.
*p < 0.01; ***p < 0.0001.

Timing of each diagnostic examination in the Delayed Group (n = 15).
There was no one who was performed CT scan or barium swallow test within 6 months from the first hospital visit in the Delayed Group.
BaS, barium swallow test; EGD, esophago-gastro-duodenoscopy; F, female; M, male; n/a, not available; n.d., not done before the treatments; (+), positive for abnormal findings in the examination; (−), negative for abnormal findings in the examination.
Symptoms related to achalasia more than 1 year after the surgery was followed up in 31 of the 38 enrolled patients (n = 20 in Non-delayed Group and n = 11 in Delayed Group). Significant improvement in the achalasia-related symptoms was observed in 14 of the 20 patients in Non-delayed Group (70.0%) and in 10 of the 11 patients in Delayed Group (90.9%). The ratio of significant improvement after surgical intervention was not different between the Non-delayed and Delayed Groups (p = 0.37, Fisher’s exact test).
In this study, we demonstrated that a diagnosis of achalasia was significantly delayed when the physicians who first came in contact with patients complaining about chest discomfort or an eating disorder failed to perform a chest CT scan or barium swallow test, in addition to routine endoscopy, in a timely fashion. Because esophageal manometry is not usually performed in the primary care setting, performing a chest CT scan or barium swallow test in a timely fashion in patients with prolonged complaints such as chest discomfort, dysphagia, or eating disorders, is highly important to avoid a delayed diagnosis of achalasia. In contrast to endoscopy, for which the sensitivity for achalasia has been previously questioned (Howard et al. 1992; Dughera et al. 2008), chest CT and barium swallow tests can be performed easily by physicians other than gastroenterologists. Moreover, the sensitivities of chest CT and the barium swallow test for achalasia are much higher than that of endoscopy. These results suggest that at least one of these examinations should be performed in addition to endoscopy in patients with prolonged eating-related symptoms to avoid a delayed diagnosis of achalasia.
Another significant finding of this study is that the sensitivity of each diagnostic examination for achalasia was estimated with a relatively narrow range by comprehensively studying a relatively large number of patients with achalasia. The results showed that the sensitivities of the barium swallow test (88.3-100.0%) and chest CT (83.8-100.0%) for achalasia were adequately high, but that for endoscopy (50.1-81.4%) was relatively low; this finding was consistent with that of a previous report noting that about 40% of patients with achalasia show normal findings in endoscopy (Howard et al. 1992). Practically speaking, because many patients with prolonged eating-related disorders are followed up only with endoscopy in the primary care setting, we estimate that there are many potential undiagnosed patients with achalasia. Therefore, establishing methodologies to prevent or identify such overlooked patients would be the desired next step of research.
Regarding the diagnostic process for achalasia, the conventional standard diagnosis was mainly based on esophageal manometry, which measures the pressure of the LES muscle (Pohl and Tutuian 2007; Agrawal et al. 2008). In the recent Chicago classification criteria of esophageal motility disorders, high-resolution manometry (HRM), which utilizes a transducer to continuously measure LES pressure, has been introduced and adopted (Bredenoord et al. 2012; Muller 2015). Another report recommended performing upper endoscopy, HRM, barium swallow tests, and CT scans as routine screening examinations for patients with a clinical history suggestive of esophageal motility disorders (Tuason and Inoue 2017). Certainly, comprehensively performing these updated diagnostic examinations would minimize the risk of overlooking patients with achalasia. However, few facilities are capable of performing all of these examinations, and these diagnostic criteria would be difficult to practice in many primary care settings. Besides, measuring LES pressure is somewhat invasive and painful. In the primary care setting, manometry should be performed after other examinations such as endoscopy, barium swallow tests, or chest CT scans, although it should eventually be performed ahead of any invasive treatments such as pneumatic dilatation or surgical myotomy (Richter 2010). Considering these facts and the results of this report, the suggested appropriate diagnostic process for achalasia in the primary care setting to avoid delayed diagnosis is as follows:
1. Upper intestinal endoscopy as the initial screening
2. Adding chest CT or a barium swallow test for patients whose endoscopic results are normal but have ongoing eating-related symptoms.
3. Adding esophageal manometry or HRM after these three examinations in capable facilities.
Especially, we would like to emphasize the usefulness of barium swallow test in the primary care setting to avoid a misdiagnosis of achalasia. Based on the results of this study and previous reports, more than 90% of achalasia patients would show some kind of esophageal motility-related abnormalities in the barium swallow test. This sensitivity of barium swallow test is as high as that of CT scan and much higher than that of endoscopy. The method of endoscopy is much more difficult than that of barium swallow test, requiring a long-term training as a gastroenterologist. In addition, CT scan may not be sufficiently available in some developing countries. On the other hand, barium swallow test can be performed relatively easily, if the examiners understand the correct procedure and interpretation of the results.
Lastly, this study did have some limitations. First, there may have been many undiagnosed patients with achalasia in the region covered by our facility. Second, the 38 enrolled patients were all Asian, and thus, the results of this study are waited to be verified in different races in the future. Such verification of the results by facilities in other countries would be surely helpful to establish an efficient screening method for achalasia in the primary care setting. Third, several previous reports have mentioned the possible inadequate sensitivity of the barium swallow test for achalasia, which is inconsistent with the results of this study (El-Takli et al. 2006; von Rahden et al. 2014). Certainly, interpreting the results of a barium swallow test can inevitably involve subjective factors to some extent; however, if performed and interpreted properly by trained physicians, it remains a very strong diagnostic tool to identify undiagnosed patients with achalasia. Besides, the report by El-Takli et al. (2006) described that some kinds of abnormalities were pointed out with barium-swallow test in 48 of the enrolled 51 patients (94.1%), though not diagnostic for achalasia in some of them. This result is almost consistent with ours. In the present study, all of the results from the barium swallow test were interpreted by skilled gastroenterologists with clinical experience of more than 5 years in the field. Performing a barium swallow test in a timely fashion will certainly reduce the risk of a delayed diagnosis of achalasia. The last limitation is that there are about 80 achalasia patients other than the enrolled 38 patients, who did not undergo surgical treatment and followed by the Department of Psychosomatic Medicine, Tohoku University Hospital. However, selection bias for this study is unlikely, because both departments keep in frequent touch and the selection of treatment is mainly left up to the patients’ decision. Disease severity or sensitivity of the diagnostic examinations was not significantly different between the patients treated by the two departments.
In conclusion, chest CT scans and barium swallow tests, as screening methods with quite high sensitivities, are useful diagnostic examinations for achalasia. Compared with endoscopy and manometry, these examinations not only are less invasive and painful, but also have higher sensitivities for achalasia. The performance of chest CT scans and barium swallow tests in a timely fashion by the physician who first examines the patient would be expected to reduce the risk of a delayed diagnosis of achalasia.
The authors declare no conflict of interest.