2019 Volume 247 Issue 2 Pages 139-147
2019 Volume 247 Issue 2 Pages 139-147
About 20% of patients with breast cancer are likely to develop breast cancer-related lymphedema (BCRL) following an axillary clearance, and BCRL can be refractory or irreversible to treatment. The aim of this pilot randomized controlled study was to evaluate the effectiveness of a 10-min holistic self-care program for patients with BCRL in Japan. The intervention group (n = 22) practiced the BCRL self-care program including 1) modified Japanese Radio Taiso (Rajio Taiso, national calisthenics in Japan), 2) gentle arm exercises combined with deep breathing, 3) central lymphatic drainage, and 4) skin care using a traditional lymphatic drainage technique daily for 6 months, while the control group (n = 21) received usual care from their hospitals. There was significant group*time interaction in the relative edema volume and relative volume change of the hand, with the intervention group having the better outcome. The intervention group showed significant improvement in transepidermal water loss as well as the mental health component summary score of the SF-8, most of BCRL-related symptoms, self-care time and score, frequencies of exercise, self-lymphatic drainage and skin care, and perceived adherence and effectiveness to self-care, although we were unable to exclude the possibility of the Hawthorne effect. Notably, even in the control group, the self-care was similarly increased, but the significant improvements were detected only in transepidermal water loss on the forearm and upper arm, pain and coldness. In conclusion, the patients who practiced the holistic BCRL self-care for 6 months have shown greater improvement.
Following an axillary clearance for breast cancer approximately 20% of patients are likely to develop breast cancer-related lymphedema (BCRL) and it can be refractory or irreversible to treatment. As BCRL can affect upper extremity function and the quality of life of patients (Kibar et al. 2017), patients generally receive education regarding self-care strategies to reduce the risk of BCRL. This education of self-care is mainly based on the phase 2 of complex decongestive therapy (CDT) which includes skin care, full-body exercise, compression, and self-lymphatic drainage (SLD). CDT is likely to control lymphedema effectively (Ridner et al. 2012). However, patients and health care workers must ideally undergo formal training of lymphatic drainage because of its complexity. Furthermore, maintaining good skin condition is essential for BCRL patients as they suffer from skin problems including dry skin, fibrosis, poorly healing wounds, and resultant cellulitis (Bernas 2013). Many manual lymphatic drainage (MLD) therapists believe that the use of skin emollient during performing SLD reduces its effectiveness even though this notion is not evidenced in the formal literature. Patients are therefore taught to apply skin emollient separately from SLD. In contrast, some studies report that lymphatic drainage performed with cream or aroma oil can reduce limb volume (Kirshbaum 1996; Barclay et al. 2006).
Often adherence to prescribed self-care was not undertaken as health care workers expected (Brown et al. 2014). Thus it has been indicated that even a daily single or double 20-min practice of SLD and other BCRL risk minimization strategies may be overwhelming for BCRL patients (Armer et al. 2011).
To introduce a simpler, yet effective, and feasible self-care program which patients can adhere over time, we developed a 10-min holistic BCRL self-care program and evaluated it in previous studies (Arinaga et al. 2015, 2016). This program consisted of 1) Japanese Radio Taiso (Radio Taiso, Radio calisthenics or Radio exercise) is the national calisthenics in Japan (Japan Post Insurance: https://www.jp-life.japanpost.jp/aboutus/csr/radio/abt_csr_rdo_movie.html), 2) gentle arm exercises combined with deep breathing (Moseley et al. 2005), 3) skin moisturizing care with grapefruit essential oil and sweet almond massage oil using a traditional self-lymphatic drainage technique, and 4) 1 min of central lymphatic drainage around the subclavian vein. In this previous study (Arinaga et al. 2015, 2016), the volume of the affected limb and tissue resistance at all measured sites were significantly reduced, and BCRL-related symptoms were also significantly improved after 6 months. We therefore conclude that the 10-min BCRL self-care program showed benefits, safety and feasibility for BCRL patients in this phase 1 study.
In the present study, we conducted the phase 2 trial to evaluate the effectiveness of the 10-min holistic BCRL self-care program.
This pilot randomized controlled study evaluating the effectiveness of the 10-min holistic self-care program for BCRL patients was approved by the Institutional Ethics Committees at Tohoku University Hospital, Fukushima Medical University Hospital, Tohoku Kosai Hospital and Miyagi Cancer Center. Informed consent to participate in this study was obtained from all patients. This study was carried out in accordance with the approved guidelines. The clinical trial registration number is UMIN000014700 and the date of registration was July 29, 2014.
ParticipantsPatients were recruited from four institutions in the Tohoku (Northeast) area of Japan. Eligibility criteria of patients are: 1) age of 20 years or more; 2) at least grade 1 unilateral BCRL assessed by Common Terminology Criteria for Adverse Events (CTCAE) v4.0; 3) six months since their last active treatment; 4) Eastern Cooperative Oncology Group (ECOG) Performance Status 0-2; and 5) to be able to respond to the study questionnaires and perform self-care. Exclusion criteria were: 1) acute inflammation or skin damage on the affected arm; 2) cancer recurrence; 3) pregnant or attempting conception; and 4) presence of a cardiac pacemaker or implantable cardioverter defibrillator (ICD) (Fig. 1).
BCRL patients were randomly allocated to either the intervention group or control group. Block randomization was used by a co-researcher and the allocation result was revealed to the investigator and patients after the written consent was submitted.
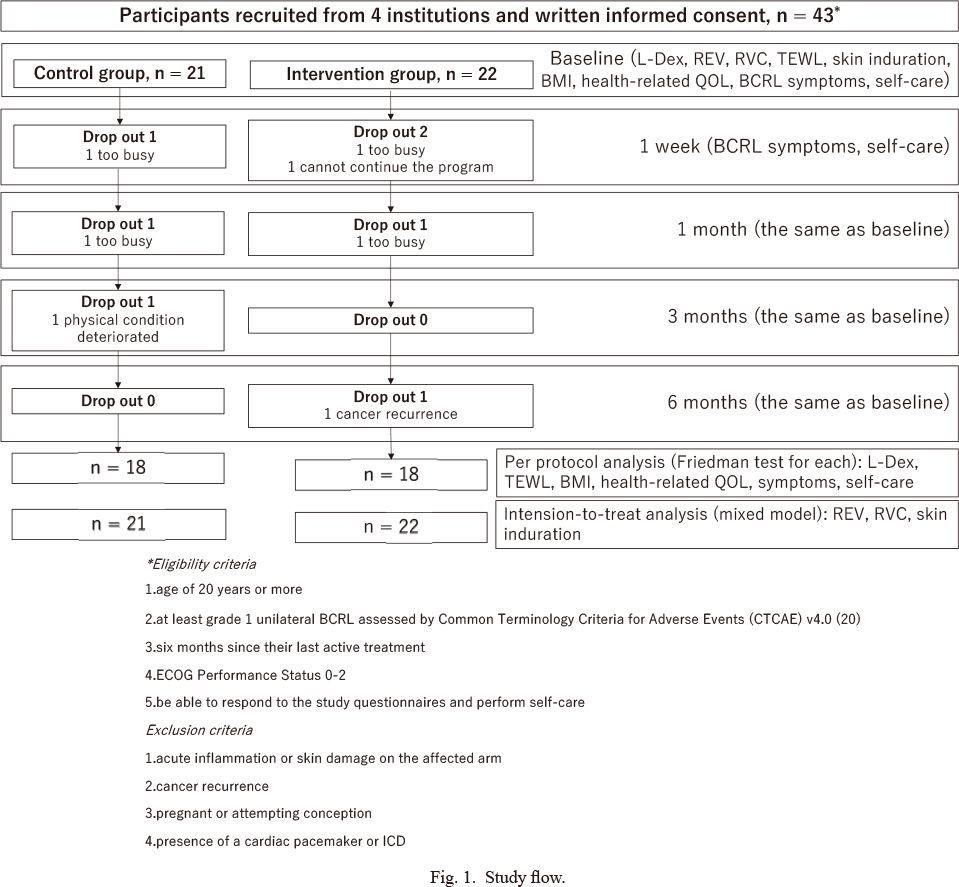
Study flow.
Forty-three participants were recruited from 4 institutions and submitted written informed consent. They were randomly allocated to the control group (n = 21) or the intervention group (n = 22), and were followed for 6 months. Totally 7 participants were dropped out during this period (n = 3 in the control group and n = 4 in the intervention group). The examinations included L-Dex, relative edema volume (REV), relative volume change (RVC), transepidermal water loss (TEWL), skin induration, body mass index (BMI), health-related quality of life (health-related QOL), breast cancer-related lymphedema (BCRL) symptoms and self-care at baseline, one month, 3 months and 6 months, and BCRL symptoms and self-care at one week. Statistical analysis was performed by Freedman test and intension-to-treat analysis.
The intervention group practiced our 10-min daily holistic BCRL self-care program which consisted of 4 elements including 1) modified Japanese Radio Taiso No. 1 (about 3 min), 2) gentle arm exercises combined with deep breathing (about 1 min) (Moseley et al. 2005), 3) central lymphatic drainage (about 1 min), and 4) skin moisturizing care using a traditional lymphatic drainage technique (about 3 min) for 6 months. They also received a leaflet explaining basic BCRL self-care (International Lymphoedema Framework 2006; Poage et al. 2008) and standard care.
Radio Taiso was introduced to maintain and improve Japanese citizen’s health in 1928 and is broadcast on TV and radio several times a day. Thus, most Japanese know Radio Taiso. A retrospective study of Radio Taiso has shown a higher basal metabolic rate, as well as improvements in muscle mass, vascular age, respiratory function, bone density, physical strength and health-related quality of life in those who regularly participate in it (Japan Research Institute 2016). Additionally, in a pre-study, we found about 50-60-ml fluid reduction from upper body immediately after Radio Taiso No. 1 (Arinaga 2014). Therefore, this Radio Taiso was used in our phase 1 study (Arinaga et al. 2016) and the present phase 2 study as well.
The intervention group was told to practice a modified Radio Taiso No.1, which is more popular than No. 2 due to its simplicity and easier motion, once a day. Although the timing to practice Radio Taiso was decided by patients for their convenience, we requested them that the timing should be same every day and so they could make it part of their daily routine. All activities were performed at half-speed to avoid injury or pain due to fibrosed tissue, stiff muscles and joint contracture and the stronger centrifugal forces if conducted at normal speed, which may lead to a tendency for fluids to move to the distal parts of the limb. Gentle arm exercises combined with deep breathing was scheduled before bathing to make it a regular part of daily life (Moseley et al. 2005). The central lymphatic drainage focusing on the subclavian drainage points was undertaken at the patient’s bath time. This central lymphatic drainage is aimed at clearing the fluid from around the shoulder and upper body after emptying central lymphatic system by gentle arm exercises combined with deep breathing. We simplified this technique from a complex traditional technique, to slowly stroking each area once toward the thoracic duct. In skin moisturizing care using a traditional lymphatic drainage technique, the milky lotion (DRX®-AD perfect barrier® body milk, ROHTO Pharmaceutical Co. Ltd., Osaka, Japan) was applied using a lymphatic drainage technique after their bath time. This drainage technique starts with gently stroking the skin around the anterior shoulder toward the thoracic duct first, then the upper arm toward the shoulder, followed by the forearm toward the upper arm, and finally the hand toward the thoracic duct. A study showed DRX-AD milky lotion is effective and safe even when there is atopic dermatitis (Kikuchi et al. 2009). As we experienced 2 incidences of mild skin reaction from the massage oil in phase 1 study (Arinaga et al. 2016), the emollient was very carefully chosen to avoid any adverse reaction as the skin of edematous limb is vulnerable and easily irritated.
The control group received standard care from their respective institutions and a leaflet as well.
MeasurementsPrimary outcome was L-Dex, the lymphedema index (ImpediMed, Brisbane, Australia), which was often used for evaluation of lymphedema lately (Kaufman et al. 2017; Iyigun et al. 2018; Whitworth and Cooper 2018). A higher L-Dex reading indicates additional extracellular fluid in the affected limb. In a study (Fu et al. 2013), the L-Dex ratio > +7.1 can be a patient at risk of BCRL. Although BCRL is not only a matter of fluid, L-Dex is still good at measuring BCRL. L-Dex was, therefore, measured at baseline, 1, 3 and 6 months.
Seven kinds of secondary outcomes were measured in this study; relative edema volume (REV), relative volume change (RVC), transepidermal water loss (TEWL), skin induration, BCRL-related symptoms, health-related quality of control (QOL), and self-care.
REV was an estimate of the relative edema volume (%), which was provided by the segmental and whole arm volume difference between the affected and unaffected arms. The whole arm volume calculation was derived from the combined upper arm, forearm and hand volumes. The hand volume was measured by water displacement. The forearm and upper arm volumes were measured by Taylor’s method (Taylor et al. 2006) which used circumferential measurement using a weighted tape measure at baseline, 1, 3 and 6 months.
RVC of hand, forearm, upper arm and whole arm was calculated by the formula [(affected arm volume at the time point/unaffected arm volume at the time point)/(affected arm volume at baseline/unaffected arm volume at baseline)−1] (Ancukiewicz et al. 2011), as this can detect smaller changes in their affected arms from the baseline.
TEWL is often used to evaluate the barrier function of the stratum corneum, which can be damaged due to lymphedema. TEWL was measured on the forearm, upper arm and breast at baseline, 1, 3 and 6 months, 3 times per each point using the H4500® (NIKKISO-THERM Co. Ltd., Tokyo, Japan), a reliable tool to measure TEWL (Kikuchi et al. 2017), and then calculated the average for statistical analysis. The site of measurement on forearm and upper arm was 5 cm below and 5 cm above the olecranon fossa, respectively. The measurement point on breast was at the intersection of the axillary and midclavicular lines. A higher TEWL indicates a poorer barrier function of the skin.
Skin induration was measured by the tonometer which is a reliable tool to measure tissue tonicity and used in BCRL studies (Pallotta et al. 2011; Vanderstelt et al. 2015; Douglass et al. 2017), as lymphedema often involves skin induration or fibrosis. The degree of skin induration on the forearm, upper arm and breast were measured at the same points as TEWL for consistency of measured sites each time and the need of a flat skin for accurate measure by this device. Each site was measured three times, and then calculated the average using a tonometer (Biomedical Engineering, Flinders Medical Centre, Adelaide, Australia) at baseline, 1, 3 and 6 months. Higher numbers indicate harder skin (fibrosis).
The items of BCRL-related symptoms were produced by a quality-of-life measure for limb lymphoedema (LYMQOL) (Keeley et al. 2010) and Upper limb lymphedema 27 (ULL27) (Launois and Alliot 2000) and from professionals and researcher advice, after face validity was examined by breast cancer specialists, dermatologists, and breast cancer researchers. BCRL symptoms, shown in Table 2, were self-reported by a 7-point (0-6) semantic differential scale (SD scale) at baseline, a week, a month, 3 months and 6 months later. 0 to 6 indicated ‘not at all’ to ‘extremely strong’, respectively. Their perceived condition and perceived change on the affected side were rated on a seven-point scale with 0 being extremely good to 6 being extremely bad. The higher scores indicate worse symptoms. These were rated at baseline, 1 week, 1 month, 3 months and 6 months.
Health-related QOL (SF-8: The Medical Outcomes Study 8-item Short Form Health Survey) (Fukuhara and Suzukamo 2004) is a short version of SF-36 which measures health-related QOL using 8 subscales. Two summary scores, physical health component summary score (PCS) and mental health component summary score (MCS), are calculated from the 8 subscale scores. A higher score indicates better quality of life. PCS and MCS were measured at baseline, 1month, 3 months and 6 months.
Some dimensions of self-care were measured. We explored the patient’s management strategies for their BCRL such as exercise, SLD, skin care and how frequently it was undertaken. (not at all, less than twice a week, more than three times a week or almost daily). The self-care score was an overall total of the points from the checklist (0-14 points) and a higher score indicates a better daily self-care practice. The knowledge and self-efficacy can influence adherence to risk management behavior, and lower distress, and higher self-regulatory ability to manage distress were associated with increased adherence (Sherman et al. 2015). Therefore, perceived adherence, effectiveness, burden to self-care (0-6 points, not at all to strongly agree) using the SD score and the average time for daily BCRL self-care were also self-reported at baseline, 1 week, 1 month, 3 months and 6 months.
Statistical analysisIntension-to-treat analysis was implemented and the imputation methods of missing data were mean substitutions from all data in each measurement.
Random intercept mixed effect linear models were used for normally distributed interval variables. The models tested the effect of treatment, time and the interaction between group and time. Dummy variables were allocated to the intervention group (1) and the control group (0).
For analysis of repeated measures of ordinal valuables and non-normally distributed valuables in interval variables, per protocol analysis using the Friedman test was implemented to test measures across all time points within each group. Post hoc pairwise multiple comparisons were applied after Friedman test. For the comparison between groups, student’s t-test and Fisher’s exact test were used.
Analysis was conducted using SPSS version 22 (SPSS, Japan). All tests were two tailed and level of significance was set at 5%.
The demographic and clinical data at baseline are shown in Table 1. There was no significant difference in the demographic data and clinical characteristics at baseline between the control group and the intervention group (Table 1). Other clinical characteristics, such as type of surgery, the level of axillary lymph nodes dissection, the period after surgery, type of adjuvant therapy and the period of BCRL, were also not significantly different between the groups (data not shown in the Table). There were non-normally distributed valuables in interval variables including BMI, L-Dex, TEWL, time for self-care and SF-8. Therefore, we used Friedman test to see the change in 6 months in each group for these variables using the raw data (control group = 18, intervention group = 18) as well as other categorical and ordinal variables (Table 2).
In the control group, 66.7% performed it for less than 10 min including 33.3% who did not practice self-care at all. In the intervention group, 77.3% performed it for less than 10 min including 36.4% who did not practice self-care at all.
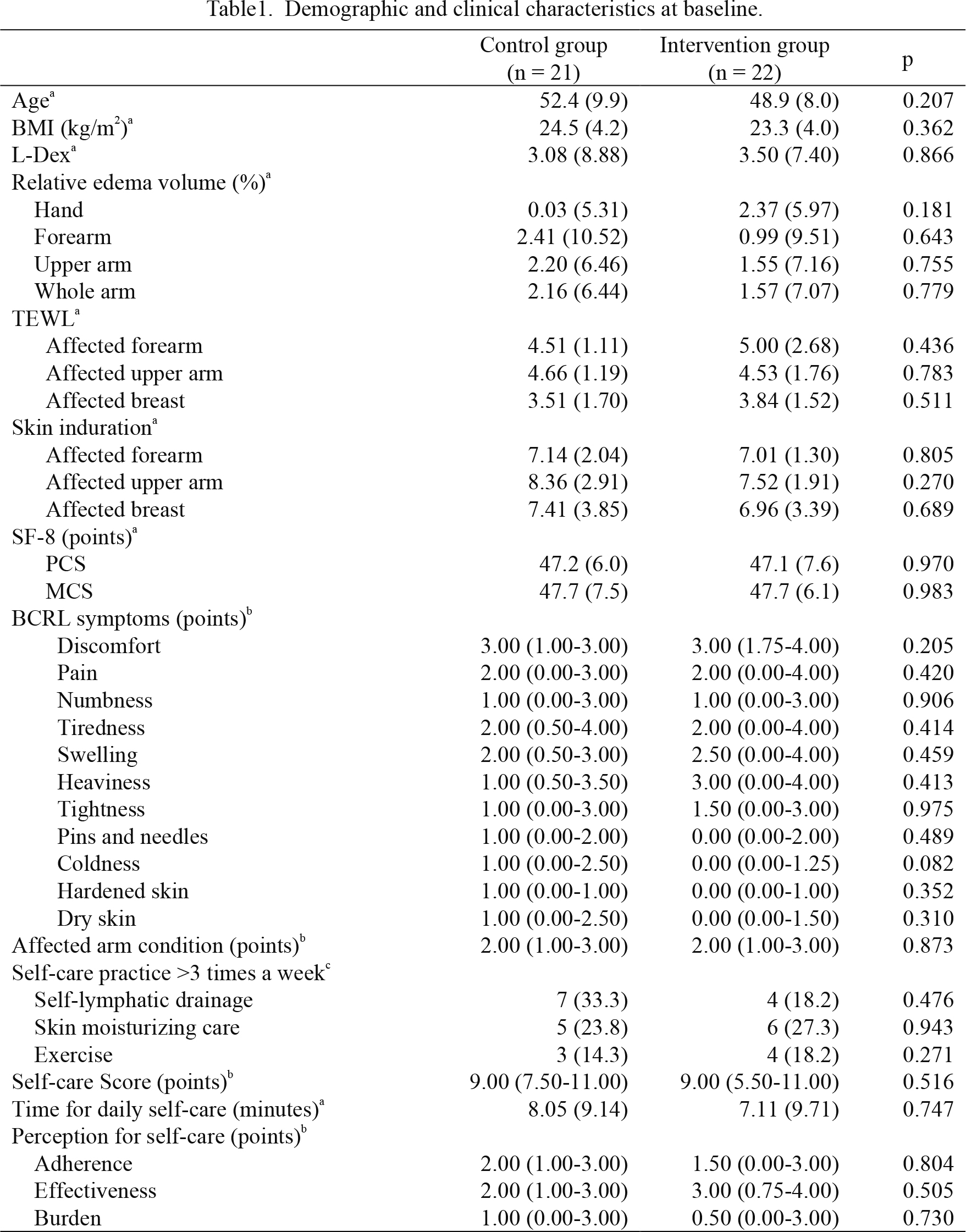
Demographic and clinical characteristics at baseline.
aData are shown as mean (SD). The difference of variables between two groups were analyzed by Student’s t-test.
bData are shown as median (25th-75th). The difference of variables between two groups were analyzed by Fisher’s exact test.
cData are shown as numbers of subjects (%). The difference of variables between two groups were analyzed by Fisher’s exact test.
BMI, body mass index; TEWL, Transepidermal water loss; SF-8, Medical Outcomes Study 8-Item Short-Form Health Survey; PCS, physical component score; MCS, mental component score; BCRL, breast cancer-related lymphedema.
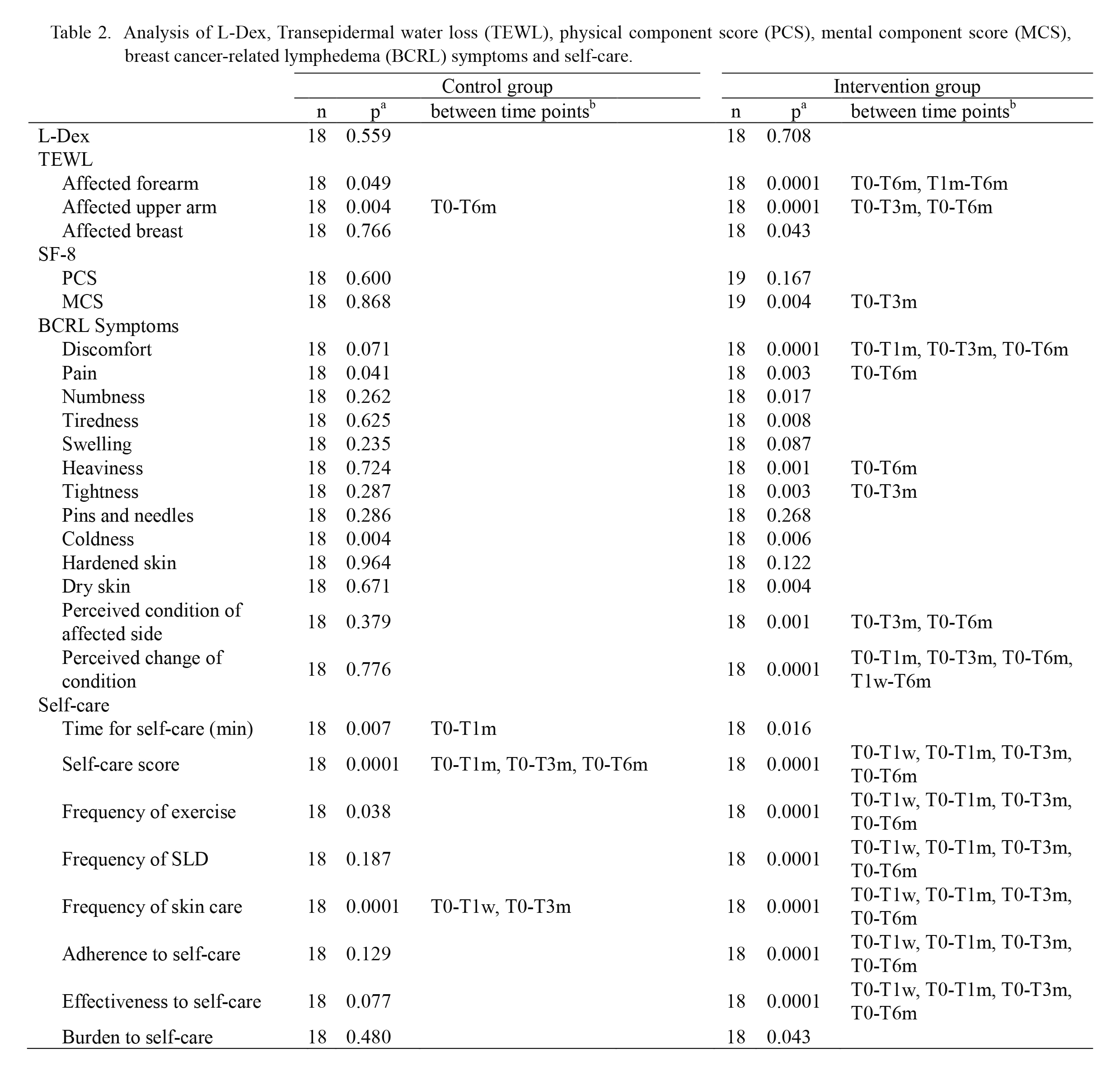
Analysis of L-Dex, Transepidermal water loss (TEWL), physical component score (PCS), mental component score (MCS), breast cancer-related lymphedema (BCRL) symptoms and self-care.
aSignificant difference over time was analyzed by Friedman test.
bSignificant difference between time points was analyzed using adjusted p values by post hoc pairwise multiple comparisons after Friedman test, and the time point intervals with significant difference (p < 0.05) are shown.
T0, baseline; T1w, 1 week; T1m, 1 month; T3m, 3 months; T6m, 6 months; SF-8, medical outcomes study 8-item short-form health survey; SLD, self-lymphatic drainage.
L-Dex showed no significant differences in either group over time (Table 2).
Secondary outcomesREV in hand showed a significant group*time interaction (p < 0.0001) and significant difference with time (p = 0.001) (Table 3). There was the significant difference between groups (p = 0.013), whereas the t-test at baseline showed no difference. There were no significant group*time interactions in forearm, upper arm and whole arm REV.
RVC in hand showed significant group*time interaction (p = 0.0001) and significant difference with time (p < 0.0001) (Table 3). There were no significant group*time interactions in forearm, upper arm and whole arm.
TEWL at forearm showed significant differences within both the control (p = 0.049) and the intervention (p < 0.0001) groups (Table 2). At upper arm, significant differences were shown within both the groups. At the breast, significant difference was only shown in the intervention group (p = 0.043).
Skin induration showed no significant group*time interactions in forearm, upper arm and breast (Table 3).
PCS showed no significant differences in either group over time (Table 2). By contrast, MCS showed a significant difference only in the intervention group (p = 0.004) (Table 2).
In BCRL related symptoms (Table 2), the significant differences over time were observed in discomfort (p = 0.001), pain (p = 0.003), numbness (p = 0.017), tiredness (p = 0.008), heaviness (p = 0.001), tightness (p = 0.003), coldness (p = 0.006), dry skin (p = 0.004), perceived condition (p = 0.001) and perceived change of condition (p < 0.0001) in the intervention group, and pain (p = 0.041) and coldness (p = 0.004) in the control group.
In self-care (Table 2), the intervention group showed significant difference in time for self-care (p = 0.016), self-care score (p < 0.0001), frequencies of exercise (p < 0.0001), SLD (p < 0.0001) and skin care (p < 0.0001), and perceived adherence (p < 0.0001), effectiveness (p < 0.0001) and burden (p = 0.043) to self-care. By contrast, the median time of self-care was 5 min at baseline and 10 min at 6 months in the control group, while it was 2 min at baseline and 10 min at 6 months in the intervention group (data not shown).
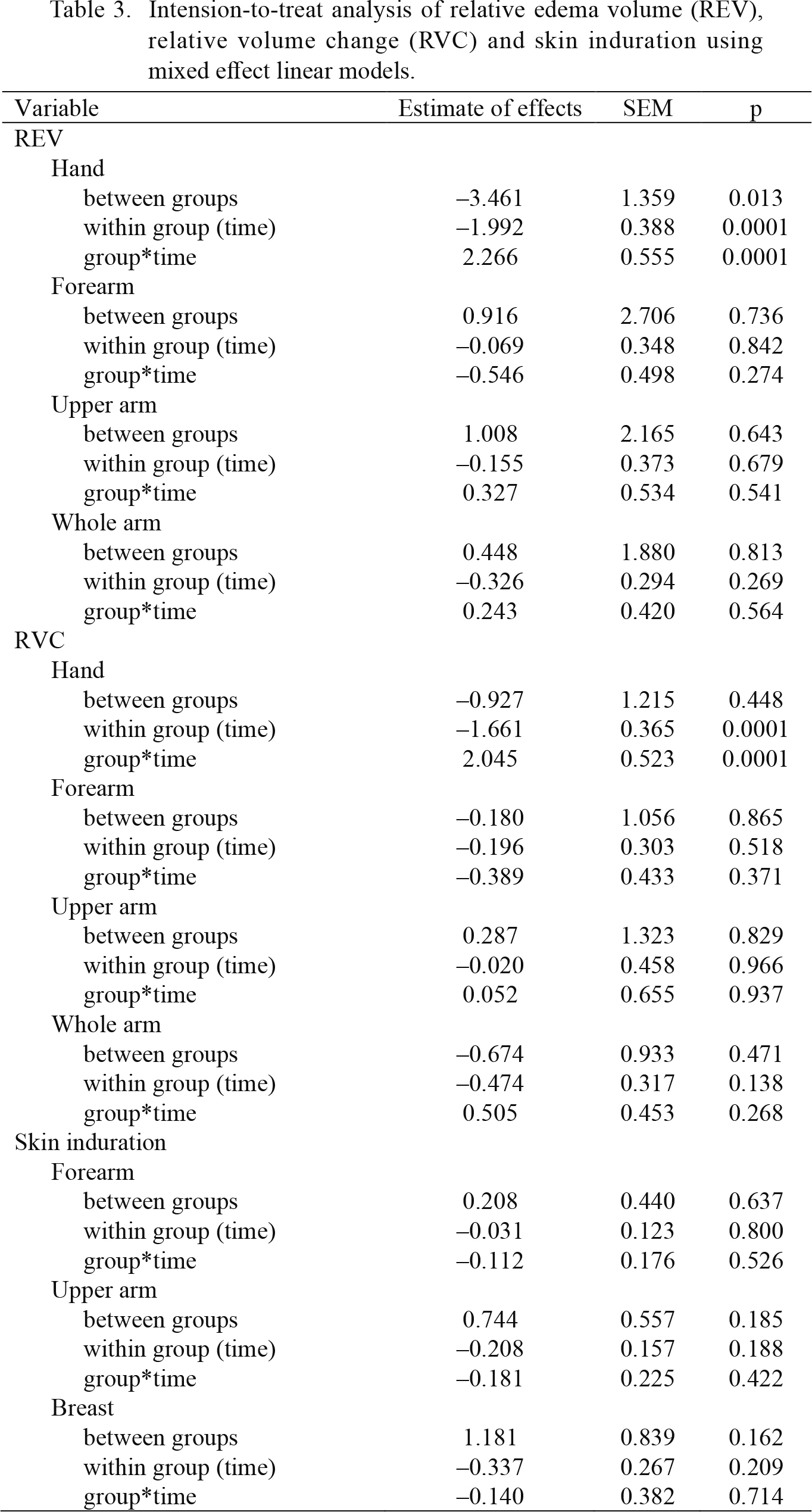
Intension-to-treat analysis of relative edema volume (REV), relative volume change (RVC) and skin induration using mixed effect linear models.
Dummy codes for groups were 0 (control group) and 1 (intervention group).
SEM, standard error of mean estimate of effects.
In the present study, the secondary outcomes showed many significant improvements in the intervention group compared with the control, although the primary outcome showed no significant difference in L-Dex. There was no significant difference in baseline characteristics between the intervention and control groups. The significant differences between the groups shown at the end of the trial, therefore, should provide a strong statistical evidence on the benefits of the BCRL self-care program. In recent studies, assessing lymphoedema by L-Dex only can be seen problematic as it cannot detect some cases (Fu et al. 2013; Sen et al. 2018). The assessment of BCRL should be more holistic including subjective measures and combination of some of objective measures such as L-Dex, RVC, MRI or ultrasonography.
RVC of the hand had a significant group*time interaction and difference over time. The result indicated the intervention group had a greater reduction in RVC than the control group. REV of the hand also had a significant group*time interaction and difference in time.
Significant decreases of TEWL for the forearm and upper arm indicate that the skin barrier function improved in both groups. This improvement can be explained by the significant increment of frequency of skin care in both groups. The skin care is important part in BCRL self-care as its pathology impacts their skin. However, TEWL for the breast only decreased significantly in the intervention group. This indicates intervention group gains greater benefits from our program.
Most of BCRL-related symptoms including discomfort, pain, numbness, tiredness, heaviness, tightness, coldness and dry skin were significantly improved in the intervention group while pain and coldness were only symptoms that improved in the control group. In addition, the perceived condition and perceived change in the condition on the affected side improved only in the intervention group.
At baseline, most of patients had practiced BCRL self-care less than 5 min, and some patients did not practice even though they had some BCRL-related symptoms. However, interestingly, we found that patients in both groups started the self-care, including exercise and skin care which were essential components of our program. It is noteworthy that the median time of self-care was 5 min and 2 min at baseline in the control group and the intervention group, respectively. Moreover, the median time of self-care increased to 10 min at 6 months in both the groups. Probably, the patients in the control group were inspired by our basic self-care leaflet and measurements, and thus they started self-care for BCRL. On the other hand, the adherence to self-care and perceived effectiveness for self-care were significantly improved only in the intervention group.
Although the average of self-care time and self-care scores were significantly improved in both groups, the intervention group showed greater improvements in many of the measures of the impact of BCRL. Practicing the determined simple self-care everyday might made the patients confident and sensitive for its effectiveness in the intervention group. The burden for self-care increased only in the intervention group. It is understandable for us as the new customs in daily life might be burdensome.
MCS significantly improved in the intervention group only. It is known that patients with lymphedema have higher distress than patients without lymphedema (Chachaj et al. 2010). A previous study suggests that the perception for effectivity in treatment and controllability of lymphedema and lymphedema symptoms can affect depression, anxiety, and stress in these patients (Alcorso and Sherman 2016). Patients who practiced our holistic self-care program may begin to believe that they are able to control their BCRL by self-care as their symptoms were improved.
There were some limitations of this study, however. First, the sample size was relatively small as this is a pilot randomized controlled trial. The power was therefore not enough to detect and show many statistically significant differences. We strongly hope that the phase 3 studies are conducted by us and/or other researchers. In addition, the basic leaflet and measurements could motivate them for self-care even though it was not our intention. It is difficult to avoid the Hawthorne effect in this kind of study, as the patients’ behavior in the control group might be influenced by participating in this study.
In conclusion, although the Hawthorne effect might occur in this study, patients who practiced this BCRL self-care for 6 months showed greater improvement in a wider range of our measured parameters compared with the control group. We propose that the 10-min holistic self-care program is effective for patients with BCRL.
We would like to express our deepest gratitude to the patients, the staff at cooperated institutions, Drs. Kakamu, Hirakawa and Kawai. This work was supported by JSPS KAKENHI Grant Number 25463419.
The authors declare no conflict of interest.